 |
Q:
Are these individuals at higher risk for corneal endothelial damage from cataract surgery? What precautions should I heed when referring them? How can I best protect them pre- and postoperatively?
Corneal microstructural changes in endothelial cell measurements in people with diabetes compared with those without the condition is well documented. Here’s the rub, though—do these morphometric changes lead to poorer post-op recovery and impaired function following cataract surgery in clinical practice? “The evidence for this is still confounding and predominantly theoretical, likely because surgical techniques have become advanced and adverse outcomes minimized with contemporary best practices and technology,” says Bhawan Minhas, OD, of The Eye Institute at Salus University. That being said, effective comanagement requires careful awareness of differences for our diabetic patients—you can’t look out for what you don’t know, she adds.
 |
|
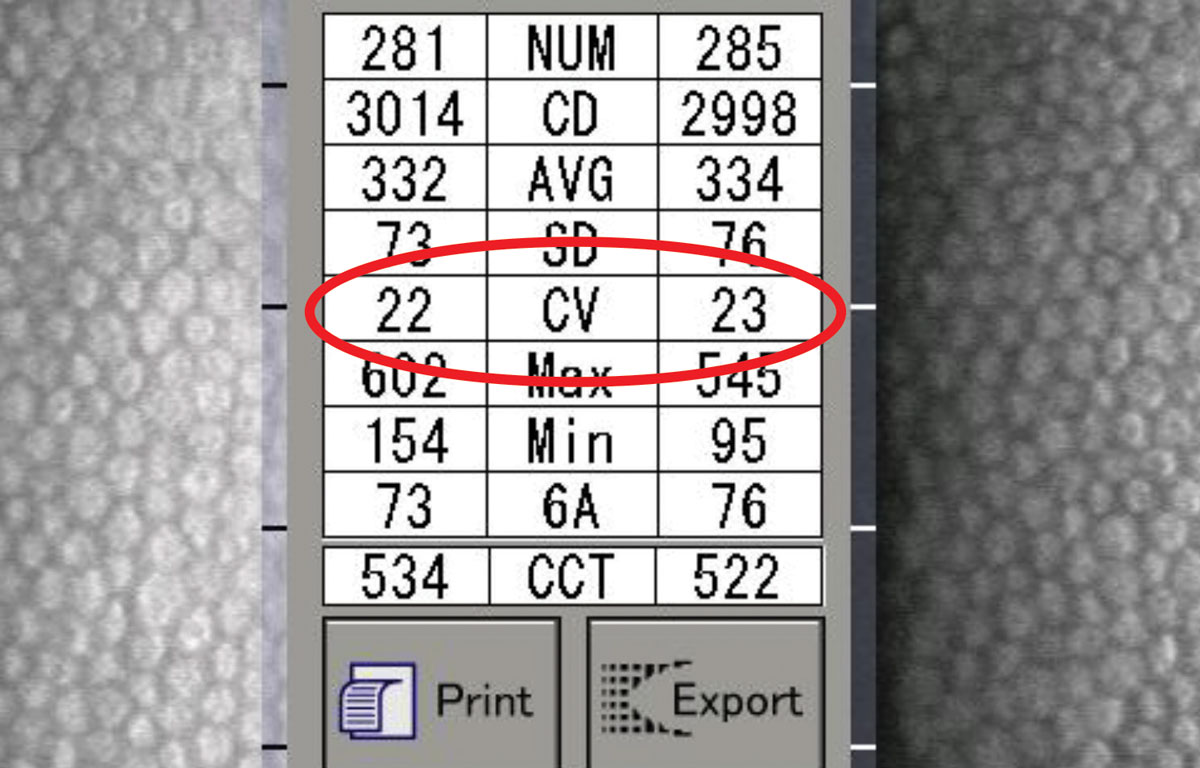
A CV less than 40 is normal. Note that CV here is of typical condition. Click image to enlarge. |
Diabetes and Cataract Surgery
Here’s an overview of what we know about undergoing cataract surgery via phacoemulsification for patients with diabetes. This population has a higher percentage coefficient of variation (CV), as measured by specular microscopy, at a three month post-op mark compared to pre-op. This metric represents how much variation there is or degree in which endothelial cells’ size differ (i.e., polymegethism). The system can measure how much cell loss occurs through the size variation between those endothelial cells, with a CV of 40 or less being normal. However, this change is also significantly less than non-diabetic patients, indicating that these individuals start with a higher CV and don’t change much after surgery.1
A higher CV suggests slower and weaker recovery of endothelial cells, according to Dr. Minhas. In a similar trend, endothelial cell density loss is also higher in these individuals compared to non-diabetic patients at one month and three months post-op.1 Thus, endothelial cell count remains important to measure and compare in the pre- and post-op period. Central corneal thickness is noted to be significantly higher at one month for these patients compared with non-diabetic patients. However, the difference stabilizes by three months post-op, warranting careful measurements for the pre- and post-op period.1
Both these suggestions would be out of an abundance of caution for diabetic patients. Decrease in the percent of hexagonality has been noted in those with and without diabetes at one month and three months post-op, too.1 However, different studies conflict on if this difference is statistically significant, she cautions.2
The minor increase between average ultrasonic energy used for phacoemulsification in diabetic individuals compared with those without is not significant in cataracts graded III or below on the Lens Opacities Classification System III scale.1
“It can be postulated that very hard nuclei would require higher energy, thus potentially showing a more significant difference, given that those with diabetes have a lower functional reserve and their corneas are theoretically more vulnerable to injury,” notes Dr. Minhas.
As for other considerations, CV is significantly higher and percentage of hexagonality significantly lower in patients who wear contact lenses compared with those who do not and non-diabetic patients.3 “As a precaution, those who wear contact lenses should be even more closely monitored in the pre- and post-op setting. There is no difference in endothelial cell density among the various degrees of diabetic retinopathy, nor with a history of photocoagulation, so the modifiable risk factor remains glycemic control,” Dr. Minhas explains.4
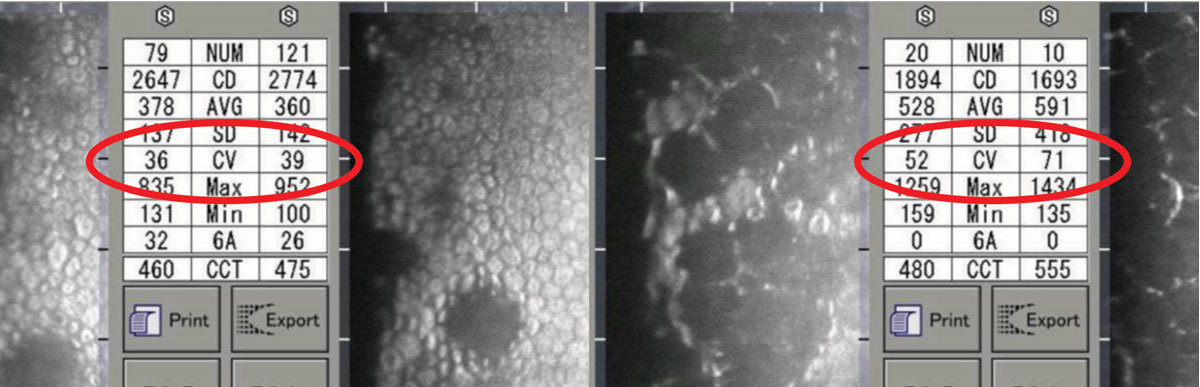 |
As CV value increases, the greater the variation seen in the size of endothelial cells. Both left and right photos show less uniform cells and greater CV values, accordingly. Click image to enlarge. |
Comanagement
Given this data, what best practices should comanaging optometrists employ? It is proven that endothelial cell density is inversely correlated with duration of disease and HbA1c, so a modifiable risk factor for post-op complication is good glycemic control as measured by HbA1c.
“Comprehensive and ongoing patient education and comanagement with endocrinology is strongly suggestive of improved outcomes,” Dr. Minhas advises. “Furthermore, comanagement with nutritionists and dieticians can help empower patients to make better choices in the early stages of the disease.”
Given the relationship to duration, timely and even early referral for cataract extraction may be considered. Remember that a harder nucleus would require more ultrasonic energy during phaco and cause further damage to the endothelium, she adds.
Considerations for discontinuation of all contact lens use prior to cataract surgery evaluation in these patients may prime the cornea for scheduled injury with known handicaps. This ‘washout’ period theoretically may allow for the known difference of CV and percent hexagonality to stabilize in diabetic patients prior to going under the knife. This would be done out of caution and would likely be reserved for the most uncontrolled cases. Finally, comanaging optometrists could consider performing endothelial cell count and use reliable means to measure central corneal thickness in high-risk individuals undergoing cataract extraction during pre-op and at multiple stages in the post-op period (consider one week, one month, three months, and six months). That being said, ophthalmologists have easy access to these measurement tools, and all that may be needed is to alert the surgeon upon referral if they have a higher-risk case on their hands—those include patients with higher HbA1c, concurrent retinopathy or proliferative disease and previous use of contact lenses.
A majority of research demonstrates that although microstructural changes can be seen, they return to pre-op values—albeit more slowly in this patient population. Dr. Minhas advises other practitioners to keep in mind that “watchful monitoring and timely intervention in the pre- and post-op period should these negative outcomes present themselves, are the only precautions we can take as comanaging providers.”
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.| 1. Sahu PK, Das GK, Agrawal S, Kumar S. Comparative evaluation of corneal endothelium in patients with diabetes undergoing phacoemulsification. Middle East Afr J Ophthalmol. 2017;24(2):74-80. 2. Hugod M, Storr-Paulsen A, Norregaard JC, et al. Corneal endothelial cell changes associated with cataract surgery in patients with type 2 diabetes mellitus. Cornea. 2011;30:749-53. 3. Leem HS, Lee KJ, Shin KC. Central corneal thickness and corneal endothelial cell changes caused by contact lens use in diabetic patients. Yonsei Med J. 2011;52(2):322-35. 4. Pont C, Ascaso FJ, Grzybowski A, Huerva V. Corneal endothelial cell density during diabetes mellitus and ocular diabetes complications treatment. J Fr Ophtalmol. 2020;43(8):794-98. |

