 |
A 74-year-old man presented to the office with a chief complaint of poor vision, OS>OD “for years.” He said the issue gradually became worse, making his left eye substantially weaker than the right. He did not report any pain. He denied trauma, systemic disease and allergies of any kind. He reported no medication use.
Clinical Findings
His best-corrected entering visual acuities were 20/40 OD and 20/60 OS. His external examination was unremarkable, with no evidence of an afferent pupillary defect. Confrontation fields were normal. Goldmann applanation tonometry measured 17mm Hg OU.
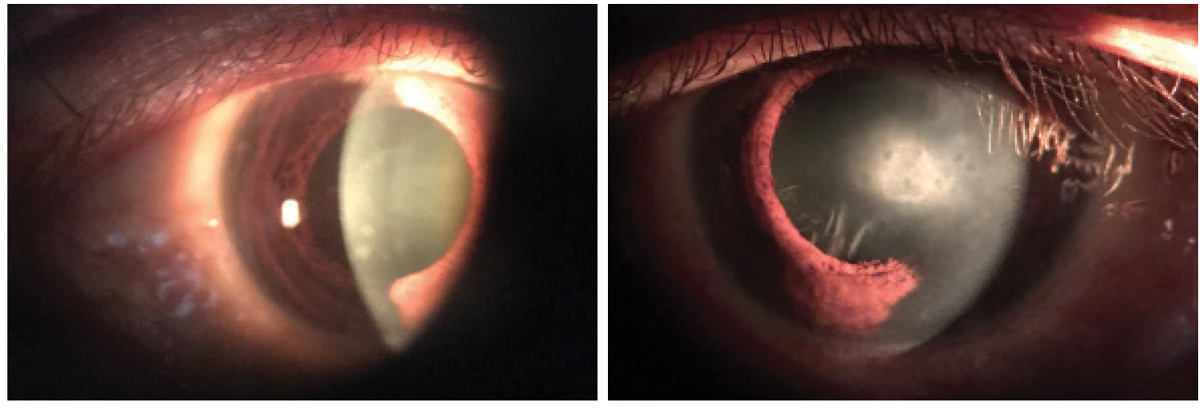
The pertinent anterior segment findings are demonstrated in the photographs below.
For More Information
Additional studies included refraction to determine if an updated spectacle prescription might improve his function. Laser interferometry could be completed to assess retinal function to ensure that if a surgical approach (cataract or corneal) were undertaken, no retinal contraindications would prevent a good outcome. Corneal staining with sodium fluorescein and rose bengal would permit understanding of the cornea’s overall health status.
 |
|
The anterior segment findings in our patient, OD (left) and OS (right). Do these presentations lead to any possible diagnoses to consider? Click image to enlarge. |
Diagnosis
The condition presented this month is Reis-Bucklers corneal dystrophy (RBD). Corneal dystrophies typically result in gradual bilateral visual changes in eyes with minimal symptoms.1-3 A hereditary corneal disorder, Reis-Bücklers is an anterior-localized corneal dystrophy characterized by superficial reticulated opacities. It occurs with or without concurrent recurrent corneal erosion.2 In general, corneal dystrophies affect approximately 0.09% of the population.4 They are identified based on their phenotype, genotype and evidence gathered during the time of their diagnosis.1-4
The clinical and pathologic features of the anterior basement membrane dystrophies overlap, presenting with many variations.1-3 Some have even speculated that these presentations represent a relative spectrum of the same entity.3
Anterior corneal dystrophies in general all present with symptoms that begin in childhood.3 They have a dominant pattern of heredity and can produce painful, recurrent corneal erosions.1-3 There are a subset of these dystrophies that differ from the usual presentations by causing visual symptoms later in life and with minimal signs of recurrent erosion.3 Fortunately, epithelial defects often occur in the disease’s later stages.
Histopathology of RBD reveals a thickening of the anterior corneal stroma secondary to an addition of partially disorganized and degenerating corneal tissue in which collagen Type III (fetal or repair collagen) is intermixed with the normal (mature) Type I collagen. This is accompanied by irregular swelling of the corneal basal epithelial cells and hyperplasia of the basement membrane (collagen Type IV, laminin and fibronectin), suggesting an aberrant influence of the epithelium on collagen synthesis.3
Management
Treatment of corneal dystrophies in general should be stage-related. Clinical and histopathological knowledge, along with experience, is indispensable. Topical supportive and antibiotic medications, therapeutic contact lenses, biotissue contact lenses and various microsurgical approaches are all viable approaches. In superficial dystrophies of the epithelium, basal membrane and/or Bowman’s layer (map-dot-fingerprint, Meesmann, Lisch, Reis-Bücklers, Thiel-Behnke) defects will induce recurrent epithelial defects, which complicate the clinical picture.1-3
Functional symptoms such as pain, edema secondary to recurrent erosions, visual loss, photophobia and foreign body sensation are frequently what provokes the patient to seek care. Medical treatments consist of drops to promote healing, ointments, hyperosmotic agents and bandage and biotissue contact lenses. Scleral contact lenses capable of creating an advantageous moisture environment have recently experienced a resurgence.5
Phototherapeutic keratectomy (PTK) using a 193nm excimer laser is often chosen as an option as well.1-3 Further, since PTK can be repeated several times more invasive corneal procedures can be postponed.1 Three major goals may be achieved by PTK depending on the diagnosis: (1) remove superficial opacities (2) regularize the surface and treat irregular astigmatism, and (3) improve the adherence of the epithelium.1
Less invasive surgical treatments include phototherapeutic keratectomy and lamellar keratectomy.1-4 More invasive procedures, such as lamellar or penetrating keratoplasty, can be considered when all other treatments fail.1-3 Anterior lamellar and endothelial keratoplasty are now preferred to penetrating keratoplasty.
We treated this patient supportively with artificial tear drops and ointments at bedtime. The lack of signs and symptoms dictated a conservative approach. We did educate the patient to the presence of the process, making him aware that treatment was available if new signs or symptoms developed.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Seitz B, Lisch W. Stage-related therapy of corneal dystrophies. Dev Ophthalmol. 2011;4(48):116-53. 2. Eggink FA, Geerards AJ, Beekhuis WH. Recovery of the visual acuity in a family with Reis-Bückler dystrophy. Cont Lens Anterior Eye. 2002;25(2):67-72. 3. Chan CC, Cogan DG, Bucci FS, et al. Anterior corneal dystrophy with dyscollagenosis (Reis-Bücklers type?). Cornea. 1993;12(5):451-60. 4. Bourges JL. Corneal dystrophies. J Fr Ophtalmol. 2017 Jun;40(6):e177-e192. 5. Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012;35(6):272-6. |

