History
A 22-year-old black female reported to the office with a chief complaint of pain in her left eye for one week. She explained that it started hurting after she participated in an experiment involving the installation of electrodes to her left eye. Her systemic and ocular histories were unremarkable. She denied allergies of any kind.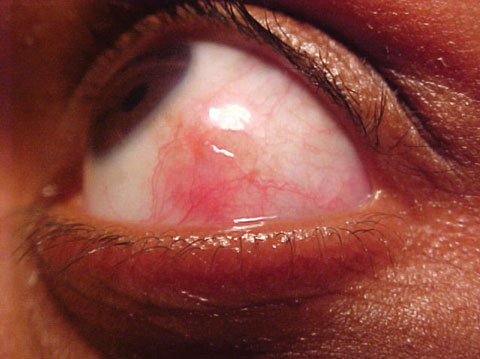 |
| This 22-year-old patient had been experiencing eye pain for about a week. In addition to her history, can this photo help you uncover the cause of her discomfort? Click image to enlarge. |
Diagnostic Data
Her best-corrected entering visual acuities were 20/20 OD and 20/20 OS at distance and near. Her external examination demonstrated observable injection OS with pain upon ocular movement OS. There was no evidence of afferent pupil defect. The pertinent biomicroscopic examination of the anterior segment, OS, is demonstrated in the photograph. There was no frank cell and flare OU. Goldmann applanation tonometry measured 15mm Hg OU. The dilated examination found no peripheral pathologies OU.
Diagnosis
Additional studies included exposure testing for photophobia, the phenylephrine blanch test (to determine the depth of inflammation), palpation of the nodes (to rule out infective processes), inspection of the conjunctiva (to establish sectoral presentation), sodium fluorescein staining (to rule out foreign body tracking), eversion of the superior lids (to rule out foreign bodies).
The diagnosis for this patient was Episcleritis, an inflammatory condition of the external eye involving the conjunctiva and its underlying connective tissue.1-11 The signature presentation demonstrates a sectorial injection involving both the episcleral tissues and overlying conjunctiva, usually concentrated in either the nasal or temporal quadrant without discharge.1-10 It is hard to document epidemiologic data as the inflammation is primarily a response to either a noxious/toxic exposure (solid, liquid, gas) or secondary to an underlying systemic disease.1-7 Idiopathic cases have been documented and seem to account for a full 33% of occurrences.12,13 Acute onset is typical, with patients often reporting that they woke up with a red eye.7 Superior injection has the potential to go unnoticed and may be completely masked by the upper eye lid in primary gaze. Most cases of episcleritis are unilateral, however, it may occur bilaterally in cases of exposure or cases precipitated by underlying systemic disease.7 Occasionally, a translucent white nodule is seen within the inflamed area (nodular episcleritis).7,11 Nodular episclersitis represents focal concentration of the inflammatory response.7,11 The nodule is often linked to underlying tissues and can be distinguished from cysts and phylectenular lesions by its characteristic lack of mobility with the conjunctiva.7,11 Patients may complain of mild pain or tenderness to the affected region, pain upon manipulation or a stabbing sensation upon moving the eyes (particularly saccadic movement). Visual acuity is unaffected.1-12 The cornea is also unaffected, although long-standing or recurrent episcleritis may lead to dellen formation.8 While it is rare that episcleritis provokes anterior iritis/uveitis, like all ocular inflammatory reactions, it is possible anterior chamber cells may be seen in more pronounced cases.1-12
Diagnostically, most cases of episcleritis will blanch with the application of topical 2.5% phenylephrine.11 In contrast, more significant ocular inflammations such as scleritis and uveitis will not blanch. Gently manipulating the inflamed region with a cotton-tipped applicator may also help distinguish the level of inflammation.
Episcleritis represents an inflammation of the episclera, the highly vascularized ocular tunic that encircles the globe between the overlying conjunctiva and the underlying sclera.1,7-12 The inflammatory response in these cases remains localized to the superficial episcleral vascular network with the histopathology showing nongranulomatous inflammation and vascular dilatation with perivascular infiltration.14 The disorder may be idiopathic or in association with some underlying systemic disease.1-12,15,16 Among those conditions linked to chronic or recurrent episcleritis are: rheumatoid arthritis, polyarteritis nodosa, systemic lupus erythematosus, inflammatory bowel disease, sarcoidosis, Wegener’s granulomatosis, tuberculosis, Lyme disease, gout, Herpes zoster and syphilis.4,6,7,10,11,15,16 The nodular form comprises the minority of cases.14
Most cases of episcleritis are self-limiting, resolving spontaneously within two to three weeks even in the absence of treatment.7,11,12 Patients who are symptomatic or who do not like their cosmetic appearance may benefit from a regimen of cold compresses, lubricants, topical nonsteroidal anti-inflammatory preparations and topical corticosteroids.1-12 Since the inflammation produced in episcleritis is relatively superficial, virtually all topical steroids are acceptable, including fluorometholone, rimexolone, loteprednol, prednisolone and difluprednate. Dosing on both the topical NSAID and topical steroid typically range from BID-Q4H.1,7,11,12 Cycloplegia is rarely necessary but can added for highly symptomatic cases exhibiting iritis. Recalcitrant or severe cases associated with systemic disease may require oral nonsteroidal anti-inflammatory drugs. Viable options for these rare instances include ibuprofen (600-800 mg BID-QID), naproxyn sodium (250-500 mg tid), or indomethacin (25-75 mg bid).1,7,11,12
The follow up on these cases should be weekly. Patients placed on steroids of any kind (topical, oral or inhaled) are at risk for steroid-induced elevation of IOP.17 Difluprednate also possesses a similar risk profile for this event.18 However, the addition of topical aqueous suppressants along with some modulation of the topical steroidal agent almost always mitigates the pressure spike. Because of the association with systemic disorders, patients with extremely severe presentations or more than three recurrences should be referred for a medical evaluation. 4,6,7,10,11,15,16
Care must be taken to distinguish episcleritis from the more severe scleritis, which has more serious implications for visual compromise and ocular sequellae. Scleritis is typically more painful, more commonly encountered bilaterally and much more likely to demonstrate an attendant uveitis. Unlike episcleritis, 2.5% phenylephrine will not induce blanching of the vascular injection in cases of true scleritis. Not every case of sectorial injection is episcleritis. Trichiasis, may mechanically induce a “pseudo-episcleritis.” Signs and symptoms should be considered before prescribing any medications.
This patient was cycopleged with cyclopentolate and started on prednisolone acetate QID, OS. Rest, light protection, cold compresses and oral over the counter analgesics were prescribed to increase comfort. The follow up was set at three days were progress and IOP would be checked. The patient recovered over the course of one week and was tapered to BID use for one week with subsequent discontinuation and dismissal.
| 1. Kirkwood BJ, Kirkwood RA. Episcleritis and scleritis. Insight. 2010;35(4):5-8. 2. Akpek EK, Uy HS, Christen W, Gurdal C, et al. Severity of episcleritis and systemic disease association. Ophthalmology. 1999;106(4):729-31. 3. Rajoo SG, Gandhewar J. Recurrent episcleritis in relation to menstruation: a case report. Cornea. 2011;30(9):1035-6. 4. Chatziralli IP, Kanonidou E, Chatzirallis A, et al. Episcleritis Related to drug-induced lupus erythematosus following infliximab therapy: a case report. Case Report Med. 2011;2011:696285. 5. Sohn EH, Wang R, Read R, Roufas A, et al. Long-term, multicenter evaluation of subconjunctival injection of triamcinolone for non-necrotizing, noninfectious anterior scleritis. Ophthalmology. 2011;118(10):1932-7. 6. Yoo JH, Chodosh J, Dana R. Relapsing polychondritis: systemic and ocular manifestations, differential diagnosis, management, and prognosis. Semin Ophthalmol. 2011;26(4-5):261-9. 7. Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: Clinical features and treatment results. Am J Ophthalmol 2000; 130(4):469-76. 8. Casser L, Lingel NJ. Diseases of the cornea. In: Bartlett JD, Jaanus SD, eds. Clinical Ocular Pharmacology, 3rd Edition. Boston: Butterworth-Heinemann, 1995:679-745. 9. Sainz de la Maza M, Jabbur NS, Foster CS. Severity of scleritis and episcleritis. Ophthalmology 1994; 101(2):389-96. 10. Pavesio CE, Meier FM. Systemic disorders associated with episcleritis and scleritis. Curr Opin Ophthalmol 2001; 12(6):471-8. 11. Goldstein DA, Tessler HH. Episcleritis, scleritis and other scleral disorders. In: Yanoff M, Duker JS. Ophtalmology 2nd Ed. Mosby, Philadelphia, 2004: 511-519. 12. Williams CP, Browning AC, Sleep TJ, et al. A randomised, double-blind trial of topical ketorolac vs artificial tears for the treatment of episcleritis. Eye (Lond). 2005;19(7):739-42. 13. Watson PG, Hayreh SS. Scleritis and episcleritis. Br J Ophthalmol. 1976;60(3):163-91. 14. Kalantan H, Al-Shawan S, Al-Katan H, et al. Nodular episcleritis in a young patient. Saudi Journal of Ophthalmol. 2006;20(3): 191-193. 15. Sadiq SA, Jennings CR, Jones NS, Downes RN. Wegener's granulomatosis: the ocular manifestations revisited. Orbit. 2000;19(4):253-261. 16. Tarabishy AB, Schulte M, Papaliodis GN, Hoffman GS. Wegener's granulomatosis: clinical manifestations, differential diagnosis, and management of ocular and systemic disease. Surv Ophthalmol. 2010;55(5):429-44. 17. Razeghinejad MR, Katz LJ. Steroid-induced iatrogenic glaucoma. Ophthalmic Res. 2011;47(2):66-80. 18. Meehan K, Vollmer L, Sowka J. Intraocular pressure elevation from topical difluprednate use. Optometry. 2010;81(12):658-62. |

