Q. I have a patient with parathyroid dysfunction and significant corneal disease. Are there any new treatments for band keratopathy?

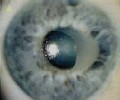
A. Varying degrees of calcium deposition, including band keratopathy, are among the complications of hyperparathyroidism. This can result in chronic foreign-body sensation, induced astigmatism or a drop in visual acuity due to corneal opacification.
There are many treatments available. Whether from parathyroid dysfunction or any other cause, band keratopathy is [traditionally] treated surgically with corneal debridement, says Heather Zutaut, O.D., center director for the Atlanta Eye Surgery Group in Atlanta. Besides debriding with a blade or spatula, applying a 1.5% neutral disodium ethylenediaminetetraacetic acid (EDTA) may allow for easier removal of the calcium deposits. However, calcium plaques may require additional solution and time to dissolve, Dr. Zutaut warns. The patient should then wear a bandage lens with prophylactic antibiotic and NSAID drops, and use an oral analgesic as needed until the epithelium heals.
After manual debridement, check the underlying stromal tissue for possible irregularities. If any are present, you can consider photo-therapeutic keratectomy (PTK) with an excimer laser to polish the surface. However, this is not Dr. Zutauts first choice because the cornea rather than the calcium is ablated. Significant irregular astigmatism is also a common complication of PTK.
In some cases, PTK is the first-line treatment for band keratopathy, Paul Karpecki, O.D., of Overland Park, Kan., says. In a French study, researchers performed PTK on 38 eyes with band keratopathy. Almost 90% of patients with smooth bands achieved visual improvement, and 85% of those with rough bands had improved ocular comfort.1 Dr. Karpecki says using EDTA as a removing agent before smoothing the surface with PTK allows for a regular corneal surface after the procedure because the laser will ablate through any remaining calcium.
An amniotic membrane transplant is the newest option for band keratopathy.
Doctors have also found success in removing band keratopathy with EDTA [alone] but had problems with re-epithelialization due to the loss of stem cells displaced by the calcium deposits, Dr. Karpecki says. Other complications of cor-neal debridement and PTK include pain, recurrence of the band, cor-neal scarring, edema and infection.
An amniotic membrane transplant may help as well in some recalcitrant cases. In a multicenter study, 16 eyes underwent amniotic membrane transplantation (AMT) as a graft after calcific deposits were surgically removed.2 Epithelialization was achieved by 93.7% of participants. The only eye that did not heal was later diagnosed with total limbal stem cell deficiency.
Also, researchers in Bangkok investigating AMT as a first-line treatment for ocular surface reconstruction have had a 75.7% success rate.3 They concluded that AMT can solve some difficult ocular surface problems, and can promote epithelial healing while reducing inflammation and scarring.
An amniotic membrane transplant has been shown to aid in re-epithelialization and to relieve the pain and foreign-body sensation associated with band keratopathy, even in eyes where the calcium returned, Dr. Karpecki says.
Whatever treatment you choose, the recurrence rate is high unless the underlying conditions are addressed, Dr. Zutaut says.
1. Dighiero P, Boudraa R, Ellies P, et al. Therapeutic photokeratectomy for the treatment of band keratopathy. J Fr Ophthlmol 2000;23(4):345-9.
2. Anderson, DF, Prabhasawat P, Alfonso E, et al. Amniotic membrane transplantation after the primary surgical management of band keratopathy. Cornea 2001;20(4):354-61.
3. Prabhasawat P, Kosrirukvongs P, Booranapong W, Vaja-radul Y. Amniotic membrane transplantation for ocular surface reconstruction. J Med Assoc Thai 2001;84(5):705-18.

