 |
One of the most unique features of an ophthalmologic exam is the ability to observe ocular vasculature in real time. This differs from the rest of the body in which advanced ultrasonographic or imaging techniques are necessary to observe this feature. As such, the examination of ocular vasculature—particularly in the retina—is often what feeds us information regarding the health of the entire body. The retina is also unique in that it has a dual blood supply, which is often impacted in vascular disease. Moreover, the retina can exhibit congenital anomalies of its vasculature, differentiating one person’s retinal vasculature from another. The most common of these congenital anomalies is the cilioretinal artery.
Vascular Divisions
A cilioretinal artery can be readily observed upon ophthalmic examination and is present in a significant proportion of healthy eyes. Besides making note of this anomalous vessel or vessels upon examination, it is important to understand its significance and how it may or may not impact retinal disease. To do this, reviewing the normal retinal vascular supply and branches is essential.
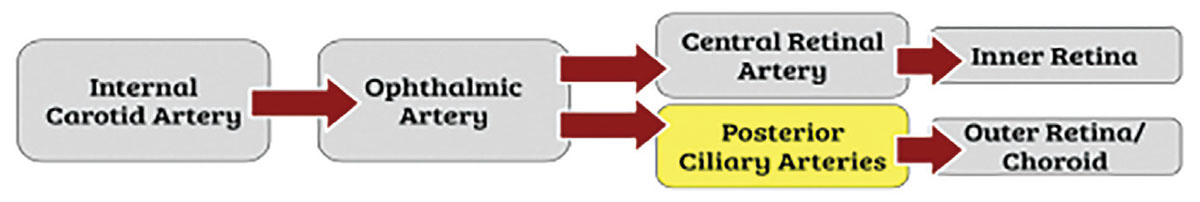
The retina and surrounding ocular structures are supplied by branches from the ophthalmic artery (OA), which is the first branch of the internal carotid artery. The internal carotid artery first leaves the cavernous sinus and almost immediately branches into the OA intracranially until it enters the both the dura and optic canal. The OA then branches into several divisions that supply various areas around the eyes and face. Two unique branches of the OA are responsible for nourishing the outer retina and choroid (posterior ciliary arteries) and the inner retina (central retinal artery; CRA).1
Usually, the first of these branches is the CRA, which is responsible for supplying the inner retina and is critical for vision. A different branch of the OA, known as the posterior ciliary arteries, supplies the outer retina and choroid. Unlike the CRA, though, these posterior ciliary arteries are not terminal—they instead divide into multiple, shorter branches to supply the proximal choroid and optic nerve head. It then pierces the sclera and continues as long posterior ciliary arteries, which supply the distal choroid. When these branches anastomose behind the lamina cribrosa, they form the circle of Zinn. The congenital anomaly known as the cilioretinal artery belongs to the posterior ciliary artery system, deriving directly from the choroid rather than the CRA and its branches.2
 |
|
A summary of the retinal vascular supply and origin of cilioretinal artery (highlighted). Click image to enlarge. |
Presentation
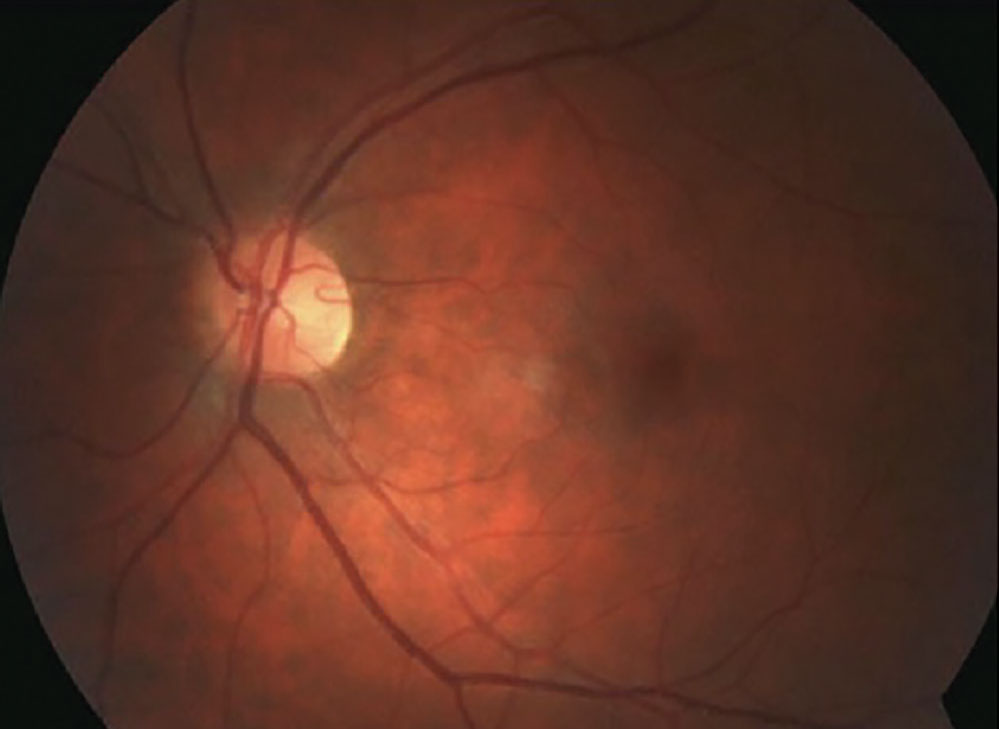
When performing a retinal examination using a condensing lens or via indirect or direct ophthalmoscopy, it is the CRA and its branches that are readily visible. The choroidal vasculature is not as easily delineated, being much deeper. However, the cilioretinal artery can also be viewed in this manner despite its derivation from the posterior ciliary artery system or choroid. It appears as a hook-like vessel coming from the edge of the optic disc resembling a “walking stick.” Although in gross appearance it can look like the rest of the CRA’s branches, it would best be distinguished using fluorescein angiography. Since the basis of fluorescein angiography is in the timing of vascular filling, with the choroidal flush occurring first, the cilioretinal artery would fill right along with it and significantly earlier than the arterial phase.2
 |
|
A temporal cilioretinal artery with classic “walking stick” appearance stemming from optic disc. Click image to enlarge. |
Clinical Implications
Cilioretinal arteries are rather prevalent and are documented in up to 49.5% of the population—arguably, not an “anomaly” at all. They are often found as solitary vessels that appear unilaterally. Most commonly, cilioretinal arteries are located on the temporal edge of the optic disc. Because of its location, it has a significant role in the circulation of the macula and, very rarely, the entire retina.2
The greatest significance of the cilioretinal artery has been documented in CRA occlusions. These are visually devastating, irreversible and, for the most part, untreatable. However, in eyes with a patent cilioretinal artery supplying the macula, vision can be spared and even return completely back to baseline following this occlusive event. The reason for this goes back to the dual vascular supply—the CRA and its branches are impacted but the posterior ciliary and choroid are not, allowing for continued perfusion from the cilioretinal artery to the area of the macula.3 Conversely, having a cilioretinal artery can also mean having an additional vessel that is at risk for an occlusive event in vascular disease, which would then impact the macula and visual acuity if present.2
One study also documented the significance of cilioretinal arteries in pathologic myopia, concluding that the presence of one in highly myopic eyes was associated with higher axial lengths and worse glaucomatous optic neuropathy. This correlation is not fully understood but is likely a result of blood flow dynamics affecting the optic nerve.4
Another area of research is the impact of cilioretinal arteries in age-related macular degeneration (AMD). The outer retina and choroid are often implicated in the pathogenesis of AMD. It has been theorized that the additional circulation provided by a cilioretinal artery could enhance oxygen tension in the macular area and be protective against the development of choroidal neovascular membranes. It has been documented that the presence of a cilioretinal artery reduced the risk of developing late-stage AMD and resulted in lower rates of neovascular membranes.5
This vascular anomaly we come across routinely on retinal examination bears a great deal of significance. Understanding the intricacies of retinal vascular supply and identifying these unique features can potentially aid in the prediction of retinal disease and progression.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Michalinos A, Zogana S, Kotsiomitis E, Mazarakis A, Troupis T. Anatomy of the ophthalmic artery: a review concerning its modern surgical and clinical applications. Anat Res Int. 2015;2015:591961. 2. Schneider M, Molnar A, Angeli O, et al. Prevalence of cilioretinal arteries: a systematic review and a prospective cross-sectional observational study. Acta Ophthalmol. 2021;99(3):e310-8. 3. Hayreh SS. Central retinal artery occlusion. Indian J Ophthalmol. 2018;66(12):1684-94. 4. Watanabe T, Kasahara K, Futagami S, et al. Cilioretinal arteries and cilioretinal veins in eyes with pathologic myopia. Sci Rep. 2019;9(1):2451. 5. Snyder K, Yazdanyar A, Mahajan A, Yiu G. Association between the cilioretinal artery and choroidal neovascularization in age-related macular degeneration: a secondary analysis from the Age-Related Eye Disease Study. JAMA Ophthalmol. 2018;136(9):1008-14. |

