 |
As eyecare practitioners, we are always in search of new tools that help elucidate a diagnosis, particularly in the case of retinal diseases. As many conditions present with overlapping clinical features, it is often necessary to distinguish between them to provide the most optimal management. One important area of assessment is in electrophysiology.
Electrophysiological testing can be a valuable tool in ophthalmic practice because it provides information about the electrical activity of the eye that cannot be obtained from a standard eye exam. First, it can provide objective, quantifiable data about retinal function that can be used to help diagnose retinal diseases, monitor disease progression and assess the effectiveness of treatment. These tests may also help in diagnosing retinal diseases in infants and young children who may not be able to cooperate with other diagnostic methods. Electrophysiological testing is also frequently used in research to identify new therapeutic targets.
Electrophysiological Tests
The most common of these tools used in the ophthalmic setting are visual evoked potentials (VEPs), electro-oculography (EOG) and electroretinography (ERG). Generally, the VEP measures the electrical activity of the brain in response to a visual stimulus. EOG measures the electrical activity of the eye muscles in response to eye movements, and the ERG, which will be our main focus, measures the electrical activity of the retina in response to light.1-8
ERG is an important tool in eye care because it provides objective and quantifiable data about retinal function while also being a noninvasive and painless procedure. Its use in the diagnosis of retinal conditions is becoming increasingly important, as it offers a great degree of information regarding the neuroretinal response to disease, treatment, genetics, age and environmental exposures.
The assessment involves placing electrodes on the surface of the eye, followed by flashing a series of bright lights in front of the eye. These electrodes measure the electrical activity of the retina in response to the light flashes.
To understand how the ERG works, a refresher about the electric potential of the eye and the intricate neuronal network of the retina is due.1,2
Retinal Electrical Activity
The electric potential of the human eye ranges from 0.4mV to 1.0mV. The cornea is electrically positive in relation to the retina; this potential difference is not generated by excitable tissue but rather is attributed to the higher metabolic rate of the retina. This electric potential changes rapidly when the eye is exposed to light, which is the basis of the ERG. An ERG is a waveform consisting of data from two processes: the receptor potential, or a-wave, which is the early negative phase arising from the retinal photoreceptors, and the positive b-wave arising from the inner nuclear layer.3
The retina is the only photosensitive tissue in the eye and is composed of over 50 neurons, including photoreceptors, bipolar cells, ganglion cells, horizontal cells and amacrine cells. For a phototransduction to occur, this precise neural network throughout the outer and inner retinal layers must be maintained. The process begins when the photoreceptors synapse with bipolar cells and transmit signals to the ganglion cells. Ultimately, the signal travels through the optic nerve to the brain for vision.4 This function of retinal neuronal and non-neuronal cells is assessed through ERG testing, which measures ion transport and the change in membrane potential using the eye’s response to a light stimulus.4-6
Types of ERGs
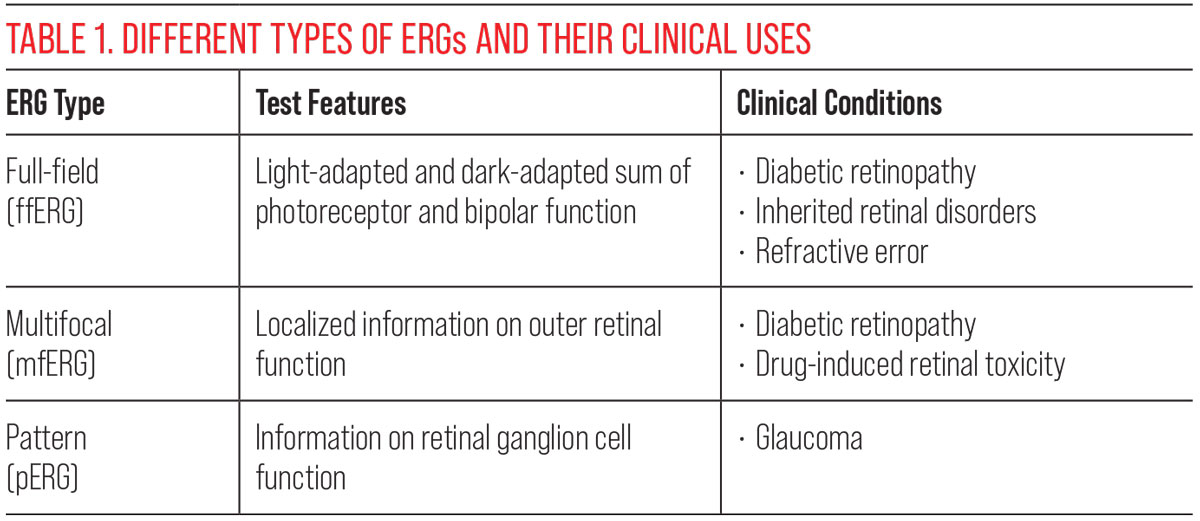
Each kind of ERG test provides unique information. A full-field ERG (ffERG) measures the total electrical activity in the retina in response to diffuse light stimulus. Typically, this is performed and recorded twice under light conditions and twice under dark conditions. The light-adapted ffERG is performed under lighting conditions that suppress rod photoreceptor function. The initial a-wave is a result of primarily cone photoreceptors and, to a lesser degree, OFF bipolar cells. The light-adapted b-wave is a function of both ON and OFF bipolar cells as well as retinal ganglion cells.
In contrast to the light-adapted procedure, the dark-adapted ffERG is performed under dark-adapted conditions in response to a brief low and moderate luminance flash. The b-wave is generated by ON bipolar cells in this case, and the moderate flash produces an a-wave consisting of a mixed rod and cone response. Overall, this type of ERG provides general information about the retina’s light response under light and dark conditions.4 A limitation to this form is that it does not localize loss of function and instead averages it over the entirety of the retina and macula.6
In contrast to the full-field, the multifocal ERG (mfERG) allows recordings from various points of the retina, including the macula and periphery under photopic conditions. Given this ability, it is useful in assessing localized areas of neural dysfunction in retinal disease. Finally, the pattern ERG (pERG) evaluates macular ganglion cell activity, which is otherwise difficult to assess with the other types.5
 |
| Click image to enlarge. |
Clinical Role
The use of ERG testing has long been recognized in the differentiation of inherited retinal disorders, as many have overlapping signs and symptoms. Testing can determine photoreceptor function for cone-rod or rod-cone dystrophies, since the principal use of ERG is in the assessment of neurons. In addition to aiding in diagnosis, the ffERG is used specifically to measure progression of disease. An example is with retinitis pigmentosa, where measuring cone degeneration is a way to elucidate the disease’s progression.6
More recently, ERG testing has found use in other retinal conditions. Although diabetic retinopathy is readily visible through clinical examination and is a known vascular disorder, evidence suggests there is a component of neural damage associated with the condition that can be uncovered using ERG testing. Light-adapted ffERG with high luminance has been able to detect cone sensitivity loss even before the clinical manifestation of retinopathy. This is likely a result of retinal hypoxia associated with diabetes. Additionally, mfERG can be helpful in measuring the extent of neurodegenerative disease in diabetes due to its ability to localize abnormalities, which may predict the progression of vascular abnormalities.5
 |
|
An example of moderately severe non-proliferative diabetic retinopathy. Using ERG testing in such a patient, neural damage may be detectable. Photo: Julie Torbit, OD. Click image to enlarge. |
Emerging studies about the role of ERG in glaucoma suggest the potential of using pERG to stratify risk of disease, since this is ERG type most sensitive to the retinal ganglion cells affected by glaucoma.7
Another area for ERG testing is drug-induced retinopathy. mfERG specifically is of great benefit due to its ability to evaluate toxicity limited to the central retina. This objective assessment can help aid the clinician in assessing the location and degree of retinal toxicity in response to chloroquine, hydroxychloroquine, VGB, interferon-alpha, ethambutol and sildenafil therapy. Moreover, it can monitor the return of function following drug cessation.8
Beyond diseases and drug toxicities, ERG has been studied in refractive errors such as myopia. For example, studies have shown that for every 1mm increase in axial length, dark-adapted ERG responses subsequently decrease, even in the absence of myopic retinal degeneration.3
These conditions are just some examples of how ERG testing has become more useful over time. Further studies are certainly needed, as this overview does not begin to cover the extent of its use. Overall, electrophysiological testing is an important tool in eye care that provides valuable information about retinal function. It is a versatile, noninvasive and objective test that has a wide range of applications in diagnosis, monitoring and research of retinal diseases.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Charles S, ed. RE Records. Electrical signals of the retinal microcircuitry. In Physiology of the Human Eye and Visual System. Harper & Row, Hagerstown. 1979:319-27. 2. Clark JW, ed. JG Webster. The electroretinogram. In Medical Instrumentation. Houghton Mifflin, Boston. 1978:177-84. 3. Kelsey JH. Clinical electroretinography. I. Br J Ophthalmol. 1967;51(5):356-7. 4. Gupta SK, Chakraborty R, Verkicharla PK. Electroretinogram responses in myopia: a review. Doc Ophthalmol. 2022;145(2):77-95. 5. McAnany JJ, Persidina OS, Park JC. Clinical electroretinography in diabetic retinopathy: a review. Surv Ophthalmol. 2022;67(3):712-22. 6. Cornish EE, Vaze A, Jamieson RV, Grigg JR. The electroretinogram in the genomics era: outer retinal disorders. Eye (Lond). 2021;35(9):2406-18. 7. Wilsey LJ, Fortune B. Electroretinography in glaucoma diagnosis. Curr Opin Ophthalmol. 2016;27(2):118-24. 8. Dettoraki M, Moschos MM. The role of multifocal electroretinography in the assessment of drug-induced retinopathy: a review of the literature. Ophthalmic Res. 2016;56(4):169-77. |

