Obstructive sleep apnea syndrome (OSAS) is both prevalent and underdiagnosed in the global population. Not only is it associated with an increased risk of cardiovascular events and diabetes, studies have connected OSAS with ophthalmologic conditions, such as non-arteritic anterior ischemic optic neuropathy, retinal vein occlusion, glaucoma and diabetic macular edema. Current evidence is inconsistent regarding the impact of OSAS on the retinal vascular network, and a new study sought to create a clearer picture of these pathophysiological changes.
 |
|
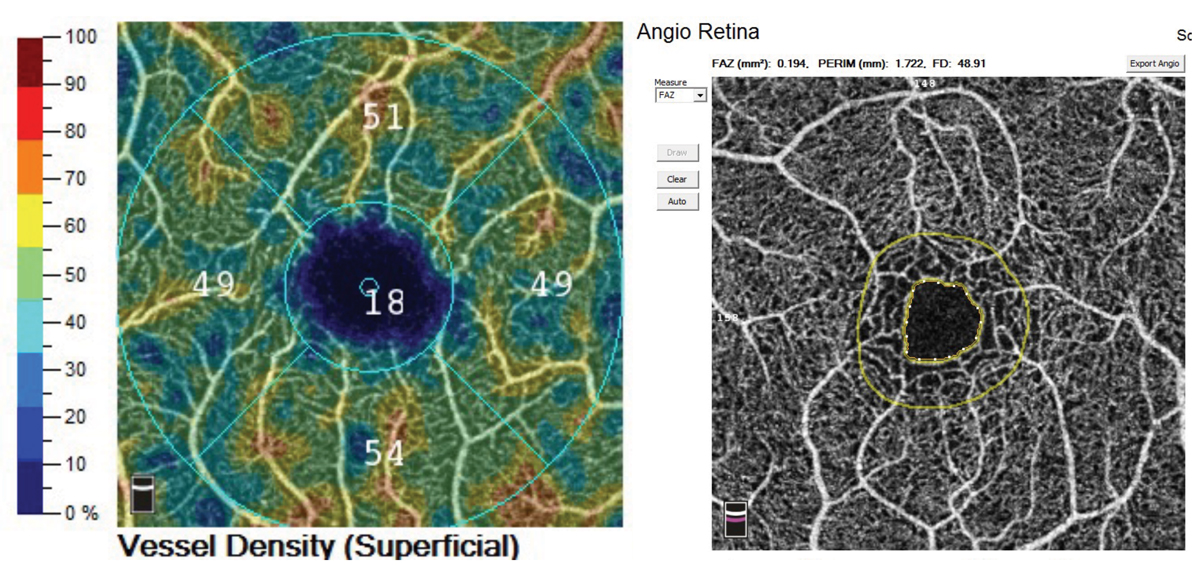
Using OCT-A, researchers captured images of the fovea and evaluated the macular vascular density and perfusion density of patients with obstructive sleep apnea syndrome, as well as those in the control group. The sleep apnea group demonstrated a significantly increased vascular density in the parafoveal and perifoveal deep capillary plexus and perfusion density in the perifoveal deep capillary plexus. Photo: Jessica Haynes, OD. Click image to enlarge. |
Using OCT-A, researchers conducted a single-center prospective observational clinical study on patients from the Sleep Laboratory of Erasme Hospital in Brussels. A total of 61 patients were divided into study and control groups, whose vascular density (VD) and perfusion density (PD) of the superficial and deep capillary plexuses were measured by OCT-A. In the OSAS groups, researchers observed significant increases in both the VD of the deep capillary plexus in the parafoveal and perifoveal areas and increased PD of the deep capillary plexus in the perifoveal area compared with those in the control. No significant differences were noted in either the VD or PD of the superficial capillary plexus.
In their recently published paper on the work, the researchers said their results are consistent with some previous studies that reported an increase in the PD in the parafoveal and perifoveal deep capillary plexus, however they also show discrepancies with other studies that observed a decrease in the PD of the deep capillary plexus. “This discrepancy in results could be explained by differences in ethnicity, age, and duration of OSAS symptoms between the study populations,” wrote the authors.
“The decrease in the retinal PD described in previous studies could be explained by endothelial dysfunction and atherosclerosis, which may be associated with long-term OSAS. In the long term, these mechanisms could be responsible for capillary occlusion or destruction at the origin of a PD-related decrease. Therefore, it would be interesting to continue the current study to investigate the VD and PD in the included patients for several years to observe whether a two-step reaction in the retinal vasculature exists in patients with OSAS,” they continued.
“It is speculated that an increase in the VD in terms of vessel length occurs secondary to hypoxia; however, the exact nature of the vessels (i.e., whether they are neovessels or collateral vessels) is unknown,” the authors stated. “The non-anarchic organization of the vessels observed in OCT-A images supports the hypothesis that they are collateral vessels that develop in response to hypoxia.”
They concluded that their results suggest that collateral vessel formation and possible retinal vasodilation occur in the deep capillary plexus for patients with OSAS, which opens new perspectives on the pathophysiology of ophthalmological complications associated with it.
“In addition, the identification of these alterations in macular VD and PD related to OSAS could allow the future development of new strategies for the prevention and treatment of ophthalmological complications in patients with OSAS,” they wrote. “Finally, studies with long-term follow-up seem to be necessary to explore and confirm the hypothesis of a two-phase pathophysiological mechanism that could explain our results and those of previous studies on older patients with OSAS.”
Abdessater L, Hein M, Rasquin F. Analysis of macular vascularization using optical coherence tomography angiography in patients with obstructive sleep apnea syndrome: A prospective clinical study. Medicina (Kaunas). 2024;2:60:5:757. |

