 |
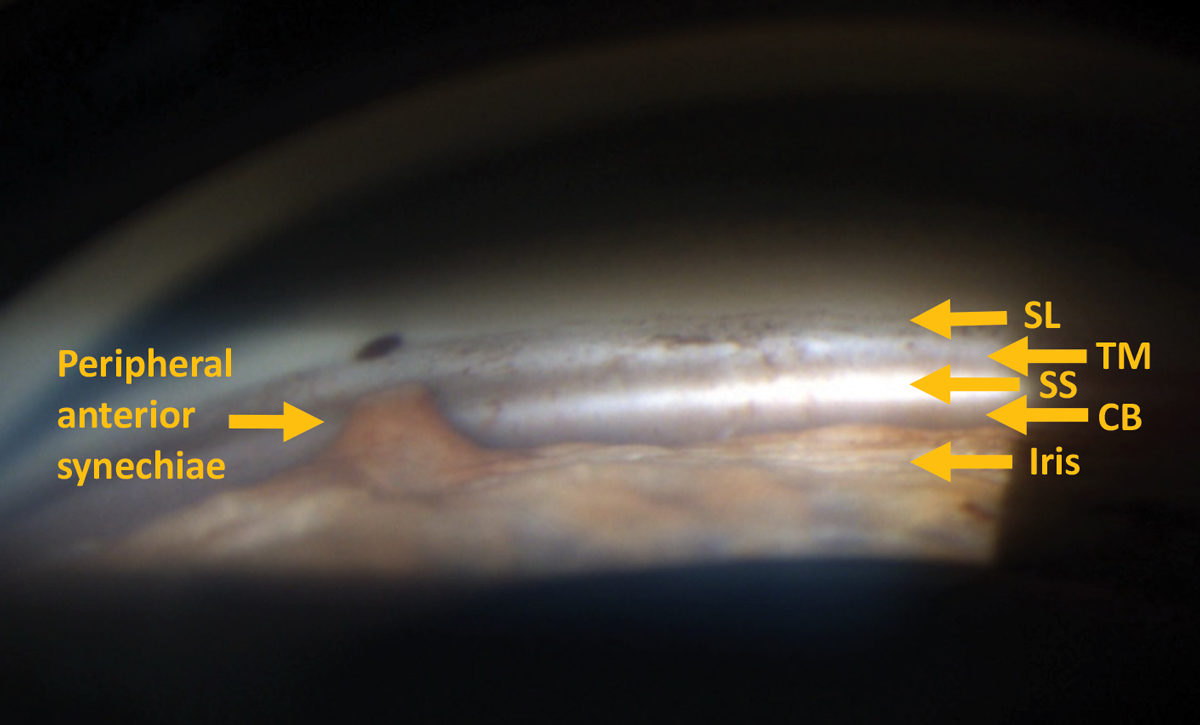
| In this study, 35.1% of patients with OAG or suspected OAG had received at least one medication associated with increased risk of acute angle-closure crisis before developing it. Photo: Amila Herbert, OD. Click image to enlarge. |
If an anatomic narrow angle is not appropriately diagnosed and treated, it can result in acute angle-closure crisis and lead to substantial vision loss. A recent retrospective study determined that in a group of Medicare patients, there appeared to have been multiple opportunities for interventions that may have averted the acute angle-closure crisis that ensued. In this cohort, only 67.5% consulted an optometrist or ophthalmologist at least once during the two-year lookback period. The research team believes that interventions targeted at addressing these risk factors and increasing eyecare access among high-risk groups may allow for better identification and treatment of these vulnerable patients.
A two-year lookback period from the date of initial presentation of acute angle-closure crisis was used to identify 1,179 patients who had at least one eyecare visit and received a diagnosis of open-angle glaucoma (OAG) or suspected OAG or took at least one medication associated with risk of acute angle-closure crisis. Of the patients who had at least one eyecare visit, those who underwent gonioscopy, received a diagnosis of an anatomic narrow angle before developing an acute crisis or both were identified. Characteristic clinical signs and symptoms of an acute attack include a mid-dilated pupil, elevated intraocular pressure, pressure-induced corneal edema, closed angles detected with gonioscopy, vascular congestion, eye pain, headache, nausea and/or vomiting.
|
For a refresher on how to perform gonioscopy, please review a recent article on the technique here. |
The researchers noted that 39.4% of patients had OAG or suspected OAG, and 35.1% had received at least one medication associated with increased risk of acute angle-closure crisis before developing it. Of the 796 patients who consulted an optometrist or ophthalmologist in the lookback period, less than one-third underwent gonioscopy in the two years before developing acute angle-closure crisis (33.2%), and less than one-half of all patients undergoing gonioscopy received a diagnosis of an anatomic narrow angle (42.8%). Most patients underwent gonioscopy in the one to four weeks preceding the acute angle-closure crisis.
The researchers suggested potential reasons for the suboptimal rates of gonioscopy include prioritization of other components of the ophthalmic examination, use of alternate methods to characterize anterior chamber angle depth, patient’s refusal to undergo the examination owing to need for topical anesthesia and potential for ocular discomfort or financial barriers. In this case, all patients were covered under the same insurance provider. Therefore, lack of insurance was not a barrier to care.
“Educational initiatives aimed at cultivating awareness among optometrists, ophthalmologists and trainees on the importance of gonioscopy as a diagnostic tool may help address the underuse of the technique,” the study authors wrote in their paper. “Reduction of financial barriers to gonioscopy, use of anterior segment imaging as adjunct testing and implementation of electronic health record reminders to flag patients at risk and facilitate timely and appropriate ophthalmic assessments may be associated with reduced incidence of acute angle-closure crisis.”
Wu AM, Stein JD, Shah M. Potentially missed opportunities in prevention of acute angle-closure crisis. JAMA Ophthalmol. May 12, 2022. [Epub ahead of print]. |

