 |
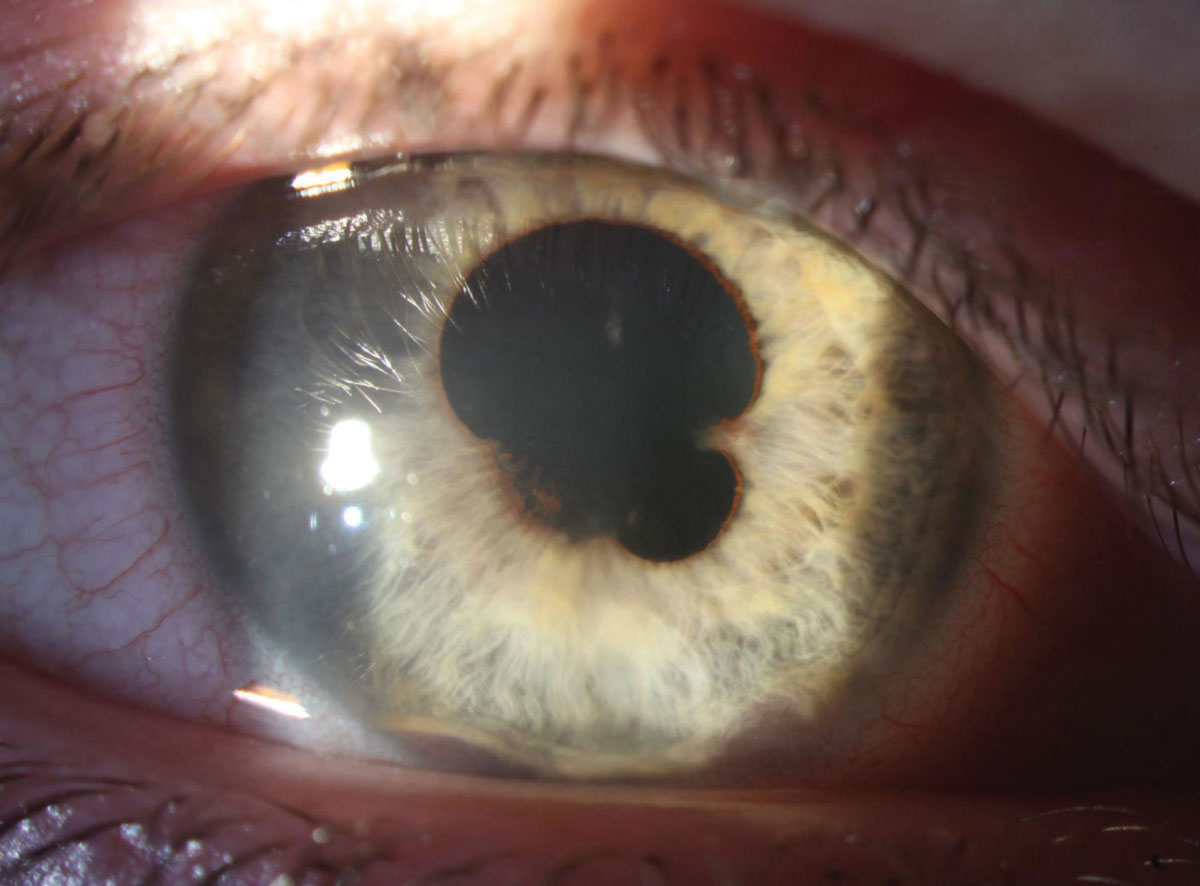
| Recurrence in the ipsilateral eye was most prevalent in the viral anterior uveitis group, with relapse in 13.4% by one year, 22.7% by five years and 44.9% by 10 years. Photo: Aaron Bronner, OD, and Alison Bozung, OD. Click image to enlarge. |
Although anterior uveitis carries a generally better visual prognosis compared to intermediate, posterior or panuveitis, it consists of up to 92% of cases and therefore contributes considerably to the overall burden of uveitis-related vision loss. Researchers based in Auckland, New Zealand, evaluated the risk of recurrence of anterior uveitis amongst a large cohort of patients to identify whether any risk factors were associated with an increased likelihood of recurrence and to evaluate the long-term visual outcomes in these patients. They determined that approximately half of patients with acute anterior uveitis will develop recurrence in the ipsilateral eye and a quarter will have recurrence in the contralateral eye.
This study, published in Ophthalmology, included 2,763 eyes of 2,092 patients followed up for a median of 8.9 years, equating to a total follow-up of 19,794.9 eye-years. The researchers believed that their method of data collection through direct chart review, rather than relying on diagnostic coding, also conferred a higher degree of accuracy.
Across the cohort, recurrence occurred in the ipsilateral eye in 1,258 eyes (45.5%) and in the contralateral eye in 522 eyes (27.3%). The overall risk of recurrence in either eye was 49.5% during the study period, with 411 eyes (14.8%) experiencing both ipsilateral and contralateral recurrence. Patients with viral uveitis experienced the greatest risk of ipsilateral recurrence and the lowest risk of contralateral recurrence. Rates of ipsilateral recurrence over 10 years were 38.1% for idiopathic disease, 43.2% for HLAB27/inflammatory arthritis and 44.9% for viral uveitis. Contralateral recurrence at ten years was 15.2% in idiopathic uveitis, 37.6% in HLAB27/inflammatory arthritis and 2.0% in viral uveitis.
On multivariate analysis, the following were associated with increased risk of ipsilateral recurrence: older age; Māori ethnicity; Asian ethnicity; HLA-B27/inflammatory arthritis; viral uveitis. There was no association with gender, smoking, bilateral disease or hypertensive uveitis. Risk factors identified for contralateral eye involvement were Māori ethnicity, Pasifika (Pacific Islander) ethnicity and HLAB27/inflammatory arthritis. Moderate vision loss (≤20/50) was present in 411 eyes (14.9%) at final follow-up and was more common if the time to first recurrence were shorter.
The study authors noted that they found a longer median time to recurrence than in previously published studies. Because this study examined all causes of vision loss, not purely permanent vision loss, they also anticipate that cataracts will have a larger influence on rates. “We know that, if we only examine permanent visual loss, then uveitic glaucoma would be responsible for over one-third of cases of anterior uveitis,” they added.
“A clearer understanding of the risk of recurrence and precipitants for relapse in anterior uveitis will allow clinicians to engage in a more informed discussion of the prognosis and disease course with patients,” they wrote.
Brodie JT, Thotahil AZ, Jordan CA, et al. Risk of recurrence in acute anterior uveitis. Ophthalmology. June 7, 2024. [Epub ahead of print]. |

