Whether you are a clinician assessing your patients’ risk for myopia or a researcher studying myopia etiology and epidemiology, patient questionnaires can provide insightful data to inform treatment and management decisions, as well as save precious chair time. One recently developed myopia survey called UH NEAR—University of Houston Near work, Environment, Activity and Refraction—can be a valuable tool to systematically collect information about children’s demographics, ocular history and visual activity.1 The survey was designed for parents of children ages five to 17 years to answer on behalf of their child to collect myopia risk factor data. It takes into account the numerous aspects of heredity, demographics and visual environment to aid clinicians and researchers in compiling relevant information that has been linked to myopia in the recent literature.
As myopia increases in prevalence and options to control the condition become more widely available, it is nearing the standard of care to discuss myopia risk, progression and management with young patients and their parents. Studies have shown that any degree of myopia increases the risk for associated potentially blinding ocular pathologies, including myopic macular degeneration, choroidal neovascularization, posterior subcapsular and nuclear cataracts and primary open-angle glaucoma.2
Family history and genetics play a significant role in the pathogenesis of myopia. One of the strongest predictors is a child’s number of myopic parents.3 However, the prevalence of myopia is increasing faster than genetics alone can account for, suggesting that generational changes in the social and visual environment may also play a role.4
While numerous environmental and behavioral factors have been studied with respect to myopia, including time outdoors, light exposure, near work, physical activity, education, urbanization and electronic device use, the three that most consistently emerge as contributing factors include time outdoors, education and near work.5-8 Unfortunately, two of these—time outdoors and near work—are notoriously difficult to quantify. While new technology takes advantage of wearable sensors to continuously and objectively measure ambient illumination and viewing distance, there are numerous limitations that prevent the widespread use of these instruments in the context of myopia, including high cost, limited availability and complex user interfaces. Therefore, subjective estimates of environmental and behavioral factors remain relevant and informative for collecting data both from clinical patients and from large populations as part of epidemiological studies.
The issue with traditional myopia risk factor surveys is that they are often long, use surrogate measures to quantify near work—such as number of books read or grades in school—include ambiguous questions, do not consider recent advances in digital media or have not been validated or widely used.5,910 Additionally, there is no single questionnaire that is standard across clinics or studies. To help address some of these limitations, the UH NEAR survey was developed to comprehensively addresses demographic, environmental and behavioral factors that can be widely used in research and clinical settings to assess risk factors for myopia.
 |
|
Given that screen time is an established risk factor for myopia, UH NEAR asks parents to estimate how long their children spend on electronic device on weekdays and weekends each during the school year and summer break. Photo: Getty Images. |
How the Survey was Developed
The UH NEAR survey was developed in several phases, as follows:
- Phase 1: The most sensitive and specific method of parental reporting for the presence of children’s myopia was determined.
- Phase 2: Questions regarding demographic factors and visual behavior were compiled, assessed and refined by the research team based on a thorough review of the literature.
- Phase 3: The developed survey was administered to focus groups to collect feedback for further refinement.
- Phase 4: A scoring system was developed.
UH NEAR Survey PDFClick here to download a PDF of the survey.
|
The study was approved by the institutional review board at the University of Houston. Procedures followed the tenets of the Declaration of Helsinki, and informed consent was obtained from participants after explaining the nature of the study.
From phase 1, it was determined that the most sensitive method for parents to correctly classify their child as myopic was the indirect method, as derived and adapted from the Orinda Longitudinal Study of Myopia.11 The indirect method uses a series of three questions, including, “Does your child wear glasses?” and if so, “What age did they receive glasses?” and, thirdly, “What is the purpose for wear (distance vision, near vision or both)?” This method has a sensitivity of 0.84 and specificity of 0.53 in correctly classifying the child as myopic or non-myopic. Therefore, with only parent input, some children will be incorrectly classified as myopic or non-myopic. This limitation is eliminated if the child is seen by a clinician or a member of a research team.
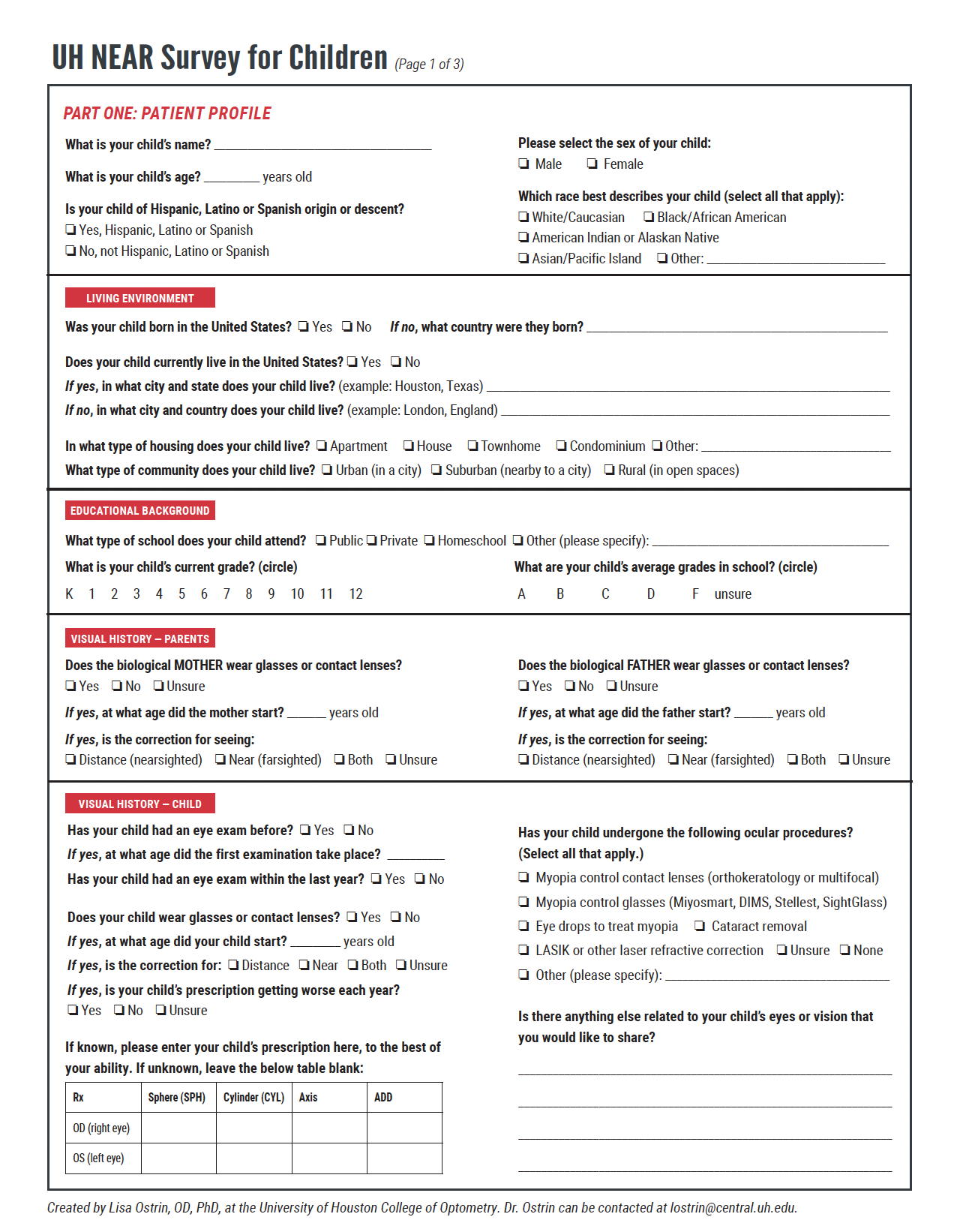
The final survey includes the following demographic information: age, sex, race and ethnicity, place and type of residence, type of school setting and average grades. The ocular history section asks about the refractive status of the biological mother and father, as well as the child, using the indirect method. Parents are asked to note the child’s prescription, if it is known. The parent should indicate if the child has had any of the following: myopia control contact lenses (orthokeratology or multifocal), myopia control spectacle lenses (i.e., MiyoSmart, DIMS, Stellest, SightGlass), eye drops to treat myopia, cataract removal, LASIK or other laser refractive correction. Parents also have the opportunity to answer an open-ended question to indicate any further information about their child’s eyes that they feel might be relevant.
Once parents complete the demographic and ocular history sections, they answer a series of visual activity questions. Here, parents are asked to estimate the time their children spend on various tasks on a weekday and a weekend day during school time as well as during summer break. The same 11 questions are asked for these four different times of the year, as the literature shows that children’s visual activity is significantly different for weekdays and weekend days, and for school sessions and summer break.12,13
These 11 items were carefully curated to include the minimum number of questions that fully encompass myopia risk factors relating to time outdoors (any time the child is exposed to sunlight, including physical or leisure activity and riding in a car), near work (whether printed or electronic) and electronic device use, including handheld devices and computers. Additionally, parents are asked to estimate their child’s sleep duration per night for the time periods mentioned previously. For each question, the parent marks the hours on a continuous rating scale from zero to 12 hours, with 15-minute increments indicated on the scale.
 |
|
Parents filling out the survey must estimate how much time children spends doing outdoor physical or leisure activities and riding in a car to determine their approximate sunlight exposure, a known myopia risk factor. Photo: Getty Images. |
Scoring the Survey
A scoresheet is provided to aid clinicians and researchers in calculating relevant metrics. The demographics and ocular history do not require any calculations and allow clinicians and researchers to easily compile important myopia-related factors, including age, parental myopia, refractive error group (myopic or non-myopic) and refraction (when available).
For visual activity, given that parents estimate children’s time spent in various activities separately for weekdays and weekend days, the overall time spent in each activity across an entire week is calculated using a weighted equation:
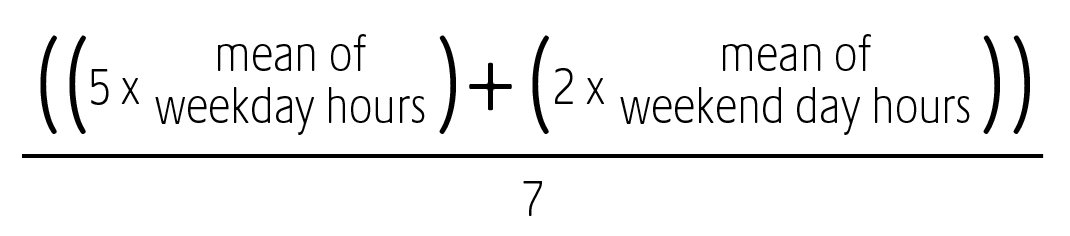 |
This calculation is performed for each of the 11 questions for school time and then for summer break. From these values, further calculations will sum time outdoors, physical activity, near work and electronic device use.
In this survey, time outdoors represents all of the time during the day that the child is exposed to sunlight, traditionally considered >1000 lux, and is calculated by adding the amount of time the child spends engaged in physical activity outdoors, leisure activity outdoors and riding in a vehicle (during the daytime).14 Physical activity encompasses any sports or vigorous activity that the child may engage in and is calculated by adding the amount of time spent on both outdoor and indoor physical activity.
In order to quantify near viewing, activities known to be performed at 10cm to 50cm are considered “near” and include reading and writing on printed material and handheld device use.15,16 Time spent using all screens is calculated by adding the amount of time the child spends using handheld devices, computers and gaming consoles and watching television.
An additional calculation provided on the score sheet is diopter hours: a weighted variable that takes into account the accommodative demand of each activity. Here, activities performed at certain distances were grouped together and multiplied by the dioptric demand.
Survey Applications
Since the UH NEAR has distinctive uses in clinical vs. research settings, below are some of its potential applications for both types of professionals.
Clinicians: Eyecare providers may find this survey useful when considering management plans for myopia patients and to collect myopia risk factor data across their patient populations. The survey can be sent to parents or guardians prior to the eye exam, filled out in-clinic while in the waiting room or administered to the parent during the child’s exam. Older children can help parents estimate time in various activities to improve accuracy, and clinicians should perform cycloplegic refractions when possible.
During focus group administration, the full 44-item survey took approximately 10 minutes for parents to answer. For a simple snapshot of the child’s activity, or to further reduce the time for completion, clinicians may decide to shorten the survey.
Factors from the survey that may indicate faster myopia progression are as follows:
- Younger age
- More myopic refraction
- Two myopia parents
- Less than 90 to 120 minutes of outdoor time per day
- High educational demands
- Extensive use of digital devices
The presence (or absence) of some or all of these factors can help clinicians identify the level of myopia risk each child potentially faces, and thus, may help to create a management plan tailored to each case.
Researchers: Myopia researchers can administer the UH NEAR survey to collect epidemiological data in clinical trials, from large populations or in laboratory-based research studies. Consistent use across labs will allow data to be pooled for diverse populations and varied geographic locations. The survey can be easily converted to an online format to facilitate wider administration and data compilation.
The greatest strength of the UH NEAR survey will come from its use in longitudinal studies, where it can be paired with objective wearable sensors to precisely quantify light exposure, near work, physical activity and sleep, along with a comprehensive eye exam including cycloplegic refractive measurement.
How to Access
Clinicians or researchers interested in using the UH NEAR survey can find a downloadable version of the full questionnaire and scoring sheet here. It can also be obtained through direct contact with the author of this article and one of the survey developers, Lisa Ostrin, OD.
Because this survey was produced based on the current understanding of myopiagenesis, it is expected to evolve and improve as potential new, previously unidentified risk factors become relevant. For use in countries other than the United States, clinicians and researchers can tailor demographic questions to the specific education system to make it most relevant to the population in question.
Whether you are a clinician or researcher, the UH NEAR survey offers a comprehensive and practical method of myopia risk assessment to encourage data-driven management of this growing patient population.
1. Gajjar S, Ostrin LA. Development of the University of Houston near work, environment, activity, and refraction (UH NEAR) survey for myopia. Clin Exp Optom. 2023:1-14. 2. Haarman AEG, Enthoven CA, Tideman JWL, et al. The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci. 2020;61(4):49. 3. Jones-Jordan LA, Sinnott LT, Manny RE, et al. Early childhood refractive error and parental history of myopia as predictors of myopia. Invest Ophthalmol Vis Sci. 2010;51(1):115-21. 4. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 5. Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279-85. 6. Li SM, Li SY, Kang MT, et al. Near work related parameters and myopia in chinese children: the anyang childhood eye study. PloS one. 2015;10(8):e0134514. 7. Guo Y, Liu LJ, Xu L, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120(2):277-83. 8. Choi KY, Chan SS, Chan HH. The effect of spatially-related environmental risk factors in visual scenes on myopia. Clin Exp Optom. 2022;105(4):353-61. 9. Rosner M, Belkin M. Intelligence, education, and myopia in males. Arch Ophthalmol. 1987;105(11):1508-11. 10. Simensen B, Thorud LO. Adult-onset myopia and occupation. Acta Ophthalmol (Copenh). 1994;72(4):469-71. 11. Zadnik K, Satariano WA, Mutti DO, Sholtz RI, Adams AJ. The effect of parental history of myopia on children’s eye size. JAMA Ophthalmol. 1994;271(17):1323-7. 12. Ostrin LA, Sajjadi A, Benoit JS. Objectively measured light exposure during school and summer in children. Optom Vis Sci. 2018;95(4):332-42. 13. Gwiazda J, Deng L, Manny R, Norton TT, Group CS. Seasonal variations in the progression of myopia in children enrolled in the correction of myopia evaluation trial. Invest Ophthalmol Vis Sci. 2014;55(2):752-8. 14. Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci. 2014;91(3):330-41. 15. Williams R, Bakshi S, Ostrin EJ, Ostrin LA. Continuous objective assessment of near work. Sci Rep. 2019;9(1):6901. 16. Bhandari KR, Shukla D, Mirhajianmoghadam H, Ostrin LA. Objective measures of near viewing and light exposure in schoolchildren during COVID-19. Optom Vis Sci. 2022;99(3):241-52. |