In April 2016, optometry lost a giant when the author of the seminal work Primary Care of the Posterior Segment, Larry Alexander, OD, died. In addition to being an optometric physician, author and educator at the University of Alabama Birmingham School of Optometry, Dr. Alexander was a past president of the Optometric Retina Society (ORS). That group chose to honor his legacy by accepting case reports from optometric residents across the country relating to vitreoretinal disease.
This case, selected by the ORS Awards Committee, was co-winner of the eighth annual Larry Alexander Resident Case Report Contest. The contest is sponsored by Topcon, Visionix (Optovue) and Heidelberg.
Poppers maculopathy is a condition characterized by bilateral sub-foveal ellipsoid zone disruption, yellow foveal spot, and reduced visual acuity. Maculopathy occurs after use of “poppers”, volatile liquid substances containing alkyl nitrites that are recreationally inhaled. Patients experience symptoms of blurred vision, central scotoma, metamorphopsia, or other central visual disturbances in the days to weeks after using poppers. Poppers use is more prevalent in men who have sex with men (MSM) and individuals with substance use. The condition is hypothesized to occur due to chronic foveal cone activation and cone apoptosis from excessive nitric oxide, causing excessive phototransduction of light. Poppers maculopathy often spontaneously resolves in the months after onset, and discontinuation of poppers may improve the prognosis. Poppers maculopathy is a rare, often subclinical manifestation of recreational drug use that is best diagnosed with OCT and a careful case history. Eyecare providers play an important role in identifying patients at risk for poppers maculopathy, counseling patients regarding drug cessation, and monitoring their prognosis over time.
Case Presentation
A 41-year-old White male presented to the Veteran Affairs Hospital optometry clinic for a comprehensive eye exam with a chief complaint of faded vision. The patient reported that letters appeared partially faded when reading for the last three months. He stated that he was able to see the letters better with slight eccentric viewing, looking adjacent to the written text. The symptom was constant since its onset three months ago. The patient denied eye pain and photopsia. His previous ocular history included dry eyes. His medical history was notable for erectile dysfunction and multiple mood disorders including depression, anxiety, panic disorder, and insomnia. He had a long history of polysubstance use for which he was currently in remission. Past substances used were stimulants, alcohol, cannabis, benzodiazepines, and opioids. His medications included bupropion, trazadone, gabapentin, and paroxetine for mood disorders and sildenafil for erectile dysfunction. His occupation was a radiology technician. The patient’s social history included a history of driving under the influence (DUI). The patient had no known drug allergies and an unremarkable family ocular history.
Upon examination, the patient’s best corrected distance visual acuity was 20/40 OD and 20/30 OS, which was reduced compared to the previous visual acuity of 20/20 OU one year ago. Refractive error was +3.00+0.75x175 OD and +2.50+0.50x160 OS. Distance cover test with spectacles showed orthophoria. Extraocular muscle motility was full and smooth OU. Pupils were equal and round without relative afferent pupillary defect OU. Confrontation visual fields were full to finger counting OD and OS. Amsler grid was performed, which revealed “murky, partially faded, or shadowy” areas surrounding central fixation in each eye. The patient denied metamorphopsia or scotoma.
Slit lamp examination was unremarkable. Intraocular pressures were normotensive OU. There was suspicion for macular disease given the reduced central visual acuity, so spectral-domain optical coherence tomography (SD-OCT) was ordered. The OCT of the maculae revealed abnormal findings (Figure 1). The Macula OCT showed subfoveal focal disruption of the ellipsoid zone (EZ) and, to letter extent, disruption of the interdigitation zone (IZ). The maculae were flat, and there was no macular edema or atrophy.
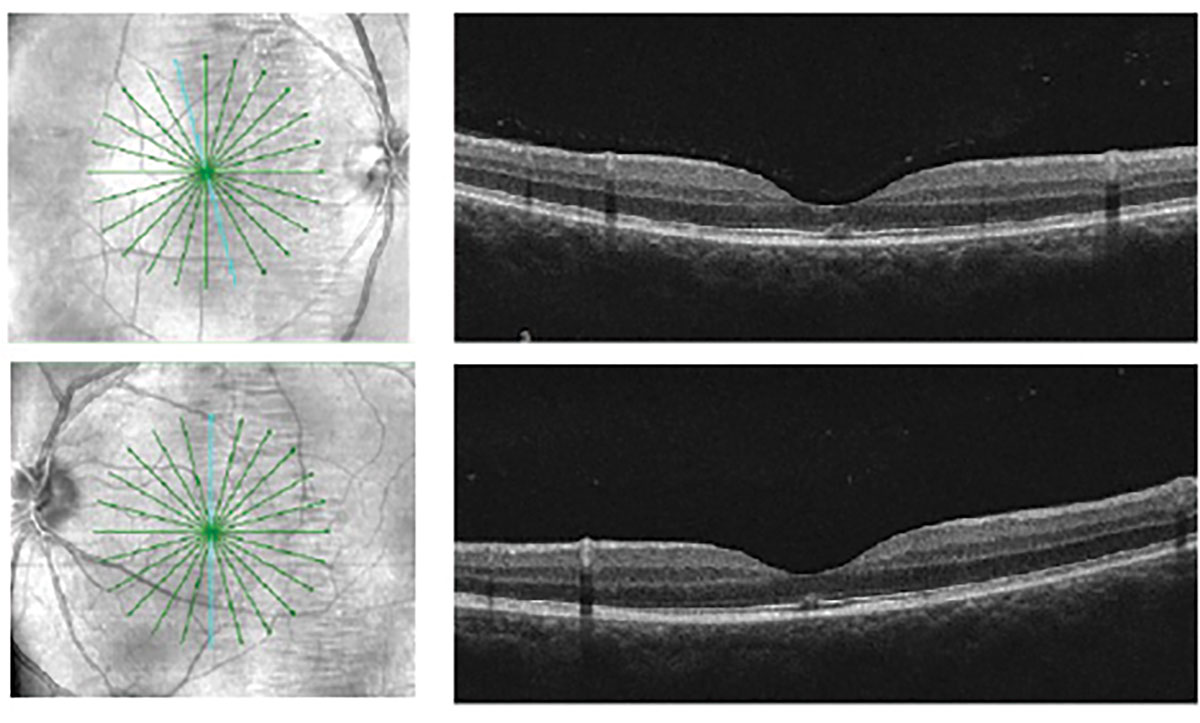 |
| Fig. 1. Cirrus HD Radial SD-OCT of the bilateral maculae revealed focal disruption of the ellipsoid zone and interdigitation zone at the fovea. Click image to enlarge. |
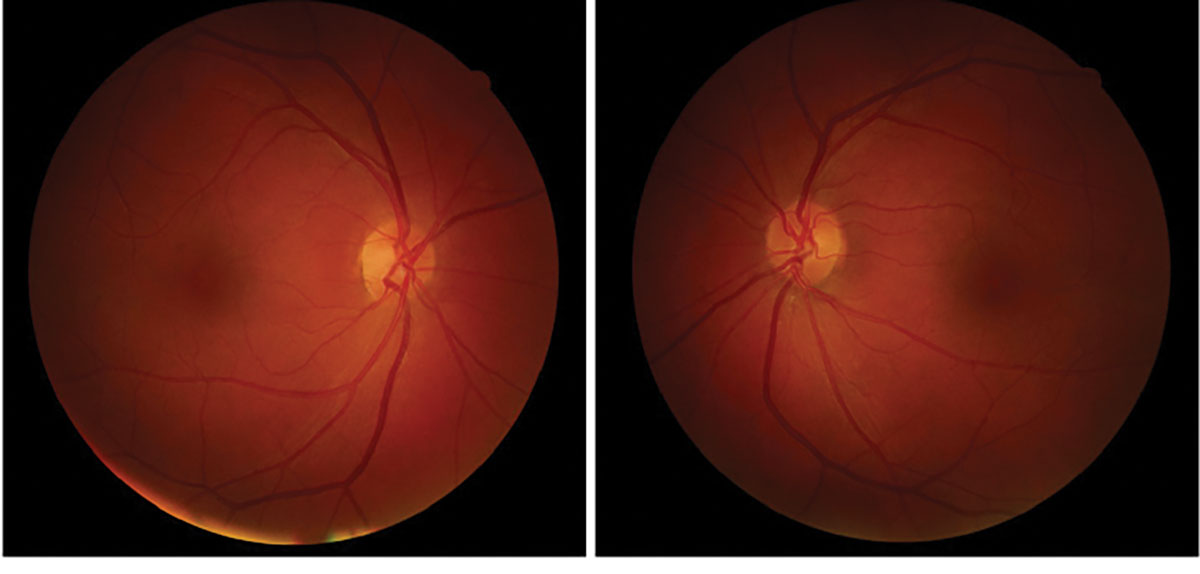
At three month follow up, ganglion cell count (GCC) OCT was unremarkable in both eyes (Figure 2). Posterior segment fundoscopy was also unremarkable at both visits with intact retina and optic nerves (Figure 3). Red-green color vision tested with Ishihara was normal in both eyes. The patient’s visual acuity had improved to 20/25 OU, and he reported improved subjective Amsler grid appearance OU. The OCT findings at three month follow up were relatively unchanged compared to the initial visit.
 |
|
Fig. 2. Fundus photography of the retinas were unremarkable. There was no macular mottling or yellow foveal spot in either eye. Click image to enlarge. |
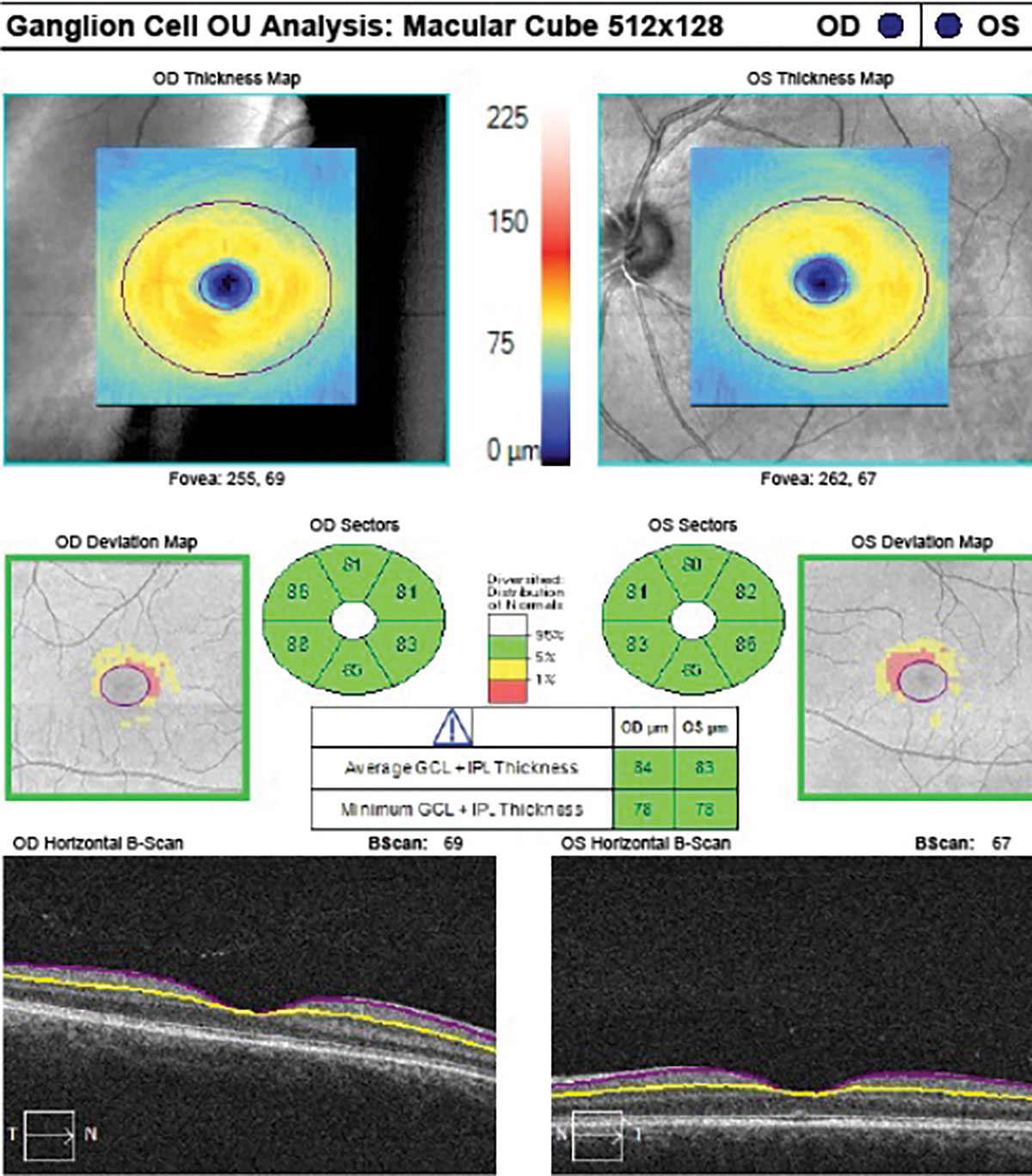 |
|
Fig. 3. Cirrus GCC OCT was unremarkable. There was no macular GCC loss in either eye. Click image to enlarge. |
Differential diagnoses based on Macula OCT
- Macular hole
- Whiplash maculopathy
- Photic maculopathy
- Tamoxifen maculopathy
- Poppers maculopathy
Macular hole occurs due to anteroposterior traction applied to the macula. Vitreomacular traction often results from posterior vitreous detachment (PVD) or epiretinal membrane (ERM). According to current OCT-based classification system, International Vitreomacular Traction Study, a full-thickness macular hole is defined as interrupted internal limiting membrane (ILM) to retinal pigment epithelium (RPE) at the fovea.1 Full thickness macular hole may resolve and leave behind residual focal EZ/IZ disruption after the vitreomacular traction regresses.2 The patient seen at Veterans Affairs Hospital did not have PVD or ERM, and the presentation was not consistent with resolved macular hole.
Whiplash maculopathy occurs from anteroposterior traction to the macula after whiplash. Whiplash refers to neck injury after sudden acceleration or deceleration, often secondary to motor vehicular accident. Whiplash maculopathy may display OCT findings of diffuse outer retinal layer disorganization, foveal neurosensory detachment, or EZ/IZ fragmentation.3 Though the diagnosis of ‘Berlin’s edema’ has similar OCT findings, Berlin’s edema also has concurrent transient opacification of the posterior pole on funduscopic exam.4 The patient denied recent trauma or whiplash.
Photic maculopathy is retinal injury due to light exposure. Photic maculopathy can result from direct or indirect exposure of the eyes to sunlight, solar eclipse, laser, arc welding, lighning, or other forms of light. Retinal changes that occur with photic maculopathy include yellow foveal lesion on fundoscopy and subfoveal EZ/RPE disruption on OCT.5 Clinical findings of photic maculopathy are nearly identical to poppers maculopathy due to the similar pathophysiologic mechanisms of both conditions.6 The patient denied photic exposure.
Tamoxifen maculopathy occurs from tamoxifen medication use. Tamoxifen is a selective estrogen receptor modulator medication used to treat some types of breast cancer in women and men. The most frequent ocular side effect of tamoxifen is retinopathy, followed by keratopathy and rarely optic neuritis.7 Retinopathy may present as crystalline deposits in the inner retina, cystoid macular edema, macular hole, or ruptured EZ at the fovea.8
A diagnosis of poppers maculopathy was made based on the patient’s reported history of poppers use. The patient admitted to first using poppers a few years ago. He used poppers at variable frequency that ranged from a few hours of daily to once monthly. He reported that he last used poppers four months prior to the onset of his visual symptoms. Given the illicit nature of poppers and the stigma associated with drug use, it is possible that the patient’s reported timeline of using poppers was inaccurate or under-reported.
Discussion
Poppers maculopathy is characterized by foveal degeneration and symptoms of central visual dysfunction secondary to nitrite inhalants. ‘Poppers’ are the colloquial term for colorless liquid chemicals made of volatile organic alkyl nitrite compounds. The nitrites were initially used in the late 1800s as prescription medication for management of angina pectoris. They were called ‘poppers’ because the nitrites were originally sold in glass vials that were popped with the fingers and inhaled.9 In 1960, the United States Food and Drug Administration (FDA) waived prescription requirements for the medication so poppers became widely used at discotheques and electronic dance music festivals. The use of all alkyl nitrites for human consumption became illegal in the United States again in 1990.9 However, poppers are now marketed as nail polish removers, leather cleaners, or liquid incense. They can be easily purchased at smoke shops, adult novelty stores, or gas stations.
Poppers are used for their vasodilatory effects. Inhaling the chemical vapors produces instant aphrodisiac effects with a rush of euphoria, arousal, and relaxation that lasts for a few minutes.10 Poppers are popular amongst the MSM community due to their effects of relaxing the anal sphincter for sexual intercourse.9 Poppers are also more used by individuals with polysubstance abuse and risky sexual behaviors.11 The inhaled chemicals travel from the lungs to the blood, brain, and other organs. Systemic side effects of poppers can include headache, dizziness, syncope, methemoglobinemia, or cardiorespiratory arrest. When poppers are used in conjunction with sildenafil, the combined vasodilatory effects of both drugs can be fatal. The patient examined at Veterans Affairs Hospital used sildenafil for erectile dysfunction in addition to poppers, though it was not inquired if he used both concurrently.
Poppers maculopathy can occur soon after inhalation of the alkyl nitrite compounds. A systematic review of 113 participants found that poppers maculopathy is most common in men (95%), with average onset of visual symptoms at forty years old.10 Participants had variable frequency of using poppers ranging from a single inhalation to over twenty years of use. Most cases of poppers maculopathy are bilateral (97%). The most common symptomatic presentation of poppers maculopathy was bilateral blurred vision, followed by central scotoma or visual field loss. Participants also reported symptoms such as phosphenes, photopsia, or metamorphopsia. The mean visual acuity at initial presentation was 20/30. Upon clinical exam, a bilateral yellow foveal spot was found in 73% of participants, and fundus autofluorescence (FAF) may show subtle foveal hyper-fluorescence (Figure 4).12 Approximately 15% of patients presented with a normal fundus like the patient seen at VA Hospital. On SD-OCT, majority of patients had subfoveal EZ disturbance (80%). Visual fields were predominantly normal. At three-month follow up, the OCT findings and mean visual acuity had improved or resolved in majority of patients. Another review of literature found that poppers maculopathy was more prevalent in Europe, likely because poppers are legal in many European countries.13 Additionally, the study found that 60% of participants who developed maculopathy were frequent poppers users.
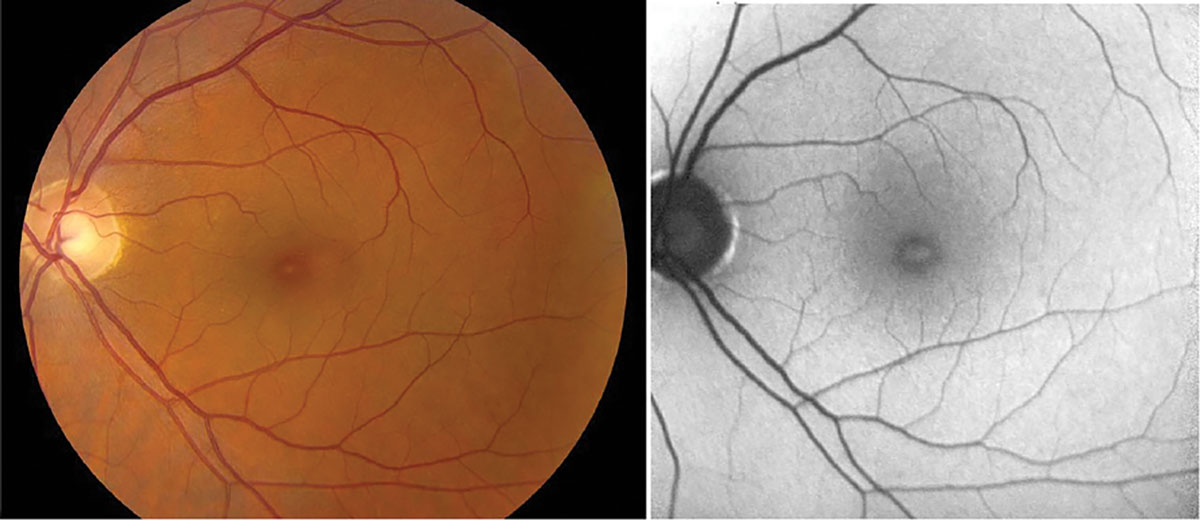 |
| Fig. 4. Fundus photo and FAF of a 45-year-old HIV-positive male with visual acuity of 20/30 OU. He reported using poppers regularly for years, with symptomatic onset of central scotoma within 24 hours of last poppers use, and duration of scotoma for seven months. Fundus photo shows yellow spot at the fovea. FAF shows corresponding foveal hyper-autofluorescence. Click image to enlarge. |
The pathophysiology of poppers maculopathy is hypothesized to be due to chronic cone activation. Poppers contain alkyl nitrites that induce an upregulation of nitric oxide synthase, which produces excessive nitric oxide (NO).13 At physiologic levels, nitric oxide modulates phototransduction, as NO becomes cyclic guanosine monophosphate (cGMP). There are cGMP-gated sodium channels present in photoreceptor outer segments which mediate phototransduction and light response of cones. At high doses, NO may induce light toxicity.
High amounts of radical NO can increase light response of cones, causing chronic activation of and apoptosis of foveal cones. This theory explains why excessive cone activation in poppers maculopathy can resemble photic maculopathy. It has been purported that middle-aged people in their forties are more likely to get poppers maculopathy due to chronic damage to foveal cones over their lifetime if they are longtime poppers users.
Management of poppers maculopathy typically involves counseling patients on poppers cessation. Anecdotal treatments in the literature include lutein, topical non-steroidal anti-inflammatory (NSAID) medication, vitamin C, and hyperbaric oxygen therapy. There is little evidence of the benefit of these anecdotal treatments. Most patients have spontaneous resolution of maculopathy in three to six months following onset of symptoms. Case reports have shown that maculopathy can improve even in patients who are chronic poppers users. Patients should additionally be provided referral to rehabilitation programs for substance use. Patients are typically monitored at three to four month intervals to monitor status of the maculopathy until resolution. Multimodal imaging such as OCT, FAF, and visual field can be helpful in monitoring the prognosis of poppers maculopathy. Color vision should be tested with HRR to monitor for acquired color vision defects. Patients can be dispensed an Amsler grid to self-monitor for changes in scotoma or metamorphopsia.
Conclusion
Poppers maculopathy is a rare bilateral retinal condition associated with use of nitrite alkyl inhalants. The condition is most common in middle-aged men with high-risk sexual behaviors who are chronic poppers users. Symptoms of poppers maculopathy that patients may report include blurred vision, central scotoma, and metamorphopsia. Common clinical features are foveal photoreceptor disruption on OCT and yellow foveal discoloration on fundoscopy. Poppers maculopathy is reversible. Foveal EZ-RPE OCT disruption and visual acuity often improves or resolves over time. Poppers cessation may improve visual and functional outcomes for patients with poppers maculopathy.
1. Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, Sadda SR, Sebag J, Spaide RF, Stalmans P. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013 Dec;120(12):2611-2619. 2. Yıldırım Ş et al. Vitreomacular Traction and Outer Retinal Structural Changes. Turk J Ophthalmol. 2019 Apr 30;49(2):109-113. doi: 10.4274/tjo.galenos.2018.79577. PMID: 31055898; PMCID: PMC6517856. 3. Cappello, Ezio et al. Spectral Domain Optical Coherence Tomography Findings In a Case of Whiplash Maculopathy With Incomplete Resolution. Retinal Cases & Brief Reports 15(4):p 421-425, July 2021. 4. Liem, Albert et al. Reversible cone photoreceptor injury in commotio retinae of the macula. Retina 15(1):p 58-61. 5. Venkatesh R et al. Multicolour imaging features in photic maculopathy. Clin Exp Optom. 2021 Mar;104(2):243-246. 6. Fajgenbaum, M. Is the mechanism of ‘poppers maculopathy’ photic injury?. Eye 27, 1420–1421 (2013). 7. Noureddin BN et al. Ocular toxicity in low-dose tamoxifen: a prospective study. Eye (Lond). 1999 Dec;13 ( Pt 6):729-33. 8. Hu Y et al. The optical imaging and clinical features of tamoxifen associated macular hole: A case report and review of the literatures. Photodiagnosis Photodyn Ther. 2017 Mar;17:35-38. 9. Romanelli, F et al. (2004), Poppers: Epidemiology and Clinical Management of Inhaled Nitrite Abuse. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 24: 69-78. 10. Caleb Bartolo et al. ‘Poppers Maculopathy’ and the adverse ophthalmic outcomes from the recreational use of alkyl nitrate inhalants: a systematic review, Seminars in Ophthalmology, 38:4, 371-379. 11. Ostrow DG et al. Recreational drugs and sexual behavior in the Chicago MACS/CCS cohort of homosexually active men. Chicago Multicenter AIDS Cohort Study (MACS)/Coping and Change Study. J Subst Abuse. 1993;5(4):311-25. 12. Rewbury R, Hughes E, Purbrick R, et al. Poppers: legal highs with questionable contents? A case series of poppers maculopathy. British Journal of Ophthalmology 2017;101:1530-1534. 13. González-Martín-Moro J et al. Poppers maculopathy: A quantitative review of previous literature. Semin Ophthalmol. 2022 Apr 3;37(3):391-398. |

