 |
A 74-year-old woman presented to the office with a chief complaint of a troublesome bump on her eyelid OD that had been present “for years.” She said the issue has gradually become worse, making her right eye unsightly.
She did not report any pain. She denied trauma, systemic disease or allergies of any kind.
Diagnostic Data
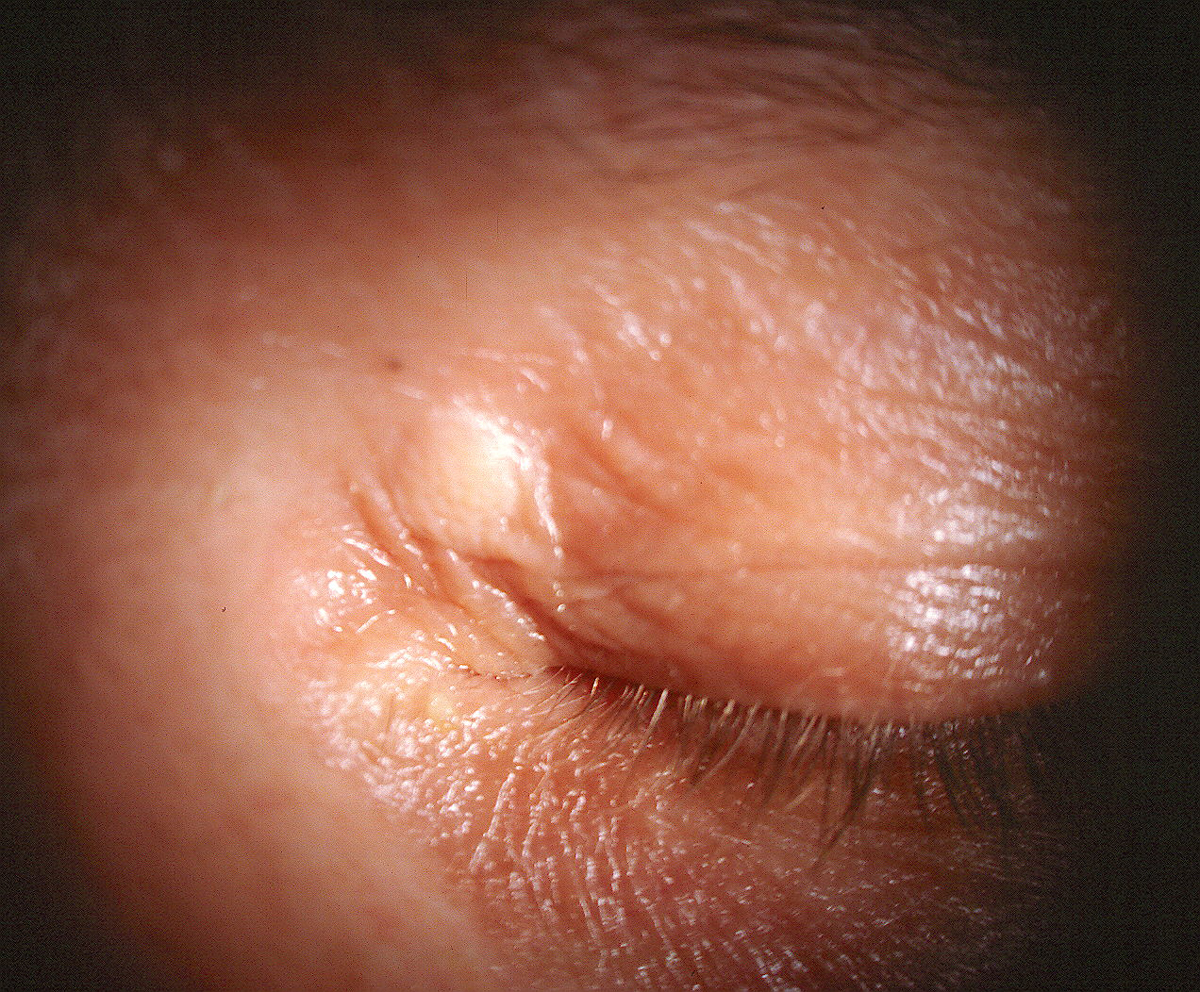
Her best-corrected entering visual acuities were 20/30 OD and 20/30 OS. Her external examination was unremarkable, with no evidence of afferent pupillary defect. Images comparable to the blemish in question are shown below. Her anterior segment findings were normal and Goldmann tonometry measured 17mm Hg OU.
Additional Testing
To learn more, other exam techniques included palpation and inspection of the lesion for tissue firmness, intact margins and any evidence of bleeding or oozing. Health history questions were also asked to rule out conditions of the skin related to undiagnosed systemic disease.
 |
| An example of periocular skin findings similar to those of the patient in question. Click image to enlarge. |
Diagnosis
The diagnosis in this issue is xanthelasma. The term is derived from the Greek xanthos (meaning yellow) and elasma (meaning plate).
Xanthelasma lesions are seen clinically as oval or elongated yellowish plaques that arise just beneath the skin of the periorbital region. Most commonly, they are located near the inner canthus of the upper eyelid (70% of cases), although they may be seen on the lower lid as well.1 In rare instances, the lesions can involve both upper and lower aspects of the lids and adnexa, encircling the eye in a mask-like fashion.2 Inspection and palpation may reveal a soft, semisolid or calcified texture.
Individuals with xanthelasma may present because of a cosmetic concern, or the condition may be detected upon routine ocular examination. Symptoms, such as pain or tenderness, are uncommon. In very rare instances, abnormally large lesions can interfere with lid function, causing ptosis or lagophthalmos. There is no tendency toward malignancy, although the lesions may enlarge and/or coalesce over time.
Most patients with xanthelasma are over 50 years of age.1 Prospective data seems to indicate no predilection difference between the genders.3 Additionally, there is no recognized racial predilection. The overall prevalence of xanthelasma is estimated at 4.4% in the general population.3 A slightly higher incidence of hypertension, ischemic heart disease, familial hypercholesterolemia, familial xanthomatosis and diabetes has also been observed in these patients.4-6
The term xanthoma describes a cutaneous deposit of fatty material, appearing as a well-circumscribed lesion in the connective tissue of the skin, tendons or fasciae.1 Xanthelasma (or more precisely, xanthelasma palpebrarum) refers specifically to any xanthoma that affects the periocular area. These account for >95% of such lesions.4
Histological evaluation of xanthelasma reveals an aggregation of foamy histiocytes (macrophages), laden with intracellular fat deposits located primarily within the upper reticular dermis.5 The main lipid component in xanthelasma is esterified cholesterol.6 A variety of factors is believed to contribute to the etiopathogenesis of xanthoma formation, including local and systemic lipid abnormalities, hormonal influences, accumulation of macrophages and leakage of plasma lipids into the dermis due to mechanical vascular trauma.4
Xanthelasma is associated with increased serum lipid fractions in about half of patients manifesting the disorder.1 In a recent study, subjects with xanthelasma were found to display elevated mean serum cholesterol, low-density lipoprotein (LDL) and very low-density lipoprotein (VLDL) levels in a statistically significant fashion as compared to their age-matched counterparts.6
In most cases, the diagnosis of xanthelasma is straightforward and can be made based upon the clinical appearance alone. If the presentation is atypical or if the personal history suggests a possibility of malignancy, incisional biopsy may be indicated. Given the significant potential for dyslipidemia and related comorbidities, laboratory evaluation of total serum cholesterol, high-density lipoprotein (HDL), LDL, VLDL, triglycerides, plasma glucose levels and liver function testing are recommended for all patients who are newly diagnosed with this condition.3,5-7
While xanthelasma is considered a benign lesion, the cosmetically unappealing nature of the condition often motivates patients to seek treatment. While dietary modifications and the use of statin drugs (e.g., atorvastatin, pravastatin) may be advantageous in managing hypercholesterolemia and other forms of dyslipidemia, there is little evidence that they have a direct impact on formed xanthelasma lesions. Still, one published case from 2005 illustrated a striking disappearance of eyelid xanthelasma in a patient after starting a course of simvastatin.15
 |
| Another example of periocular skin findings similar to those of the patient in question. Click image to enlarge. |
Intervention
Several techniques can be employed to remove these lesions successfully. Perhaps the least invasive modality involves the use of chemocautery agents, such as dichloracetic acid. This colorless, mildly pungent smelling liquid agent has both keratolytic and cauterant properties and may be obtained from a compounding pharmacy or purchased as part of a complete treatment kit (Derma-Cauter-All, North Pine Enterprises).8
The use of gentle liquid nitrogen cryotherapy has also been advocated as a potentially effective therapy but this modality has some associated discomfort and post-treatment eyelid swelling.9 Numerous anecdotal remedies for xanthelasma may be found online and may be encountered by patients. Some of these include: topical application of crushed garlic, castor oil or lemon rind; a “cleansing diet” consisting of only fresh papaya or pineapple and water for three consecutive days; niacin supplements; and exercise and stress reduction techniques. There are also a variety of cosmetic products with names like XanthRemover and Naturalis.
These xanthelasma treatments claim to be as effective and less expensive than surgical treatment. Unfortunately, none offer any scientific evidence regarding their efficacy.
Additionally, cryotherapy carries a risk of depigmentation in individuals with darker skin tones.10 More invasive therapies include low-voltage radiofrequency ablation, laser photoablation and surgical excision.11-14
Xanthelasma is extremely uncommon in patients under the age of 30. If noted, these individuals should be evaluated thoroughly for dyslipidemia and associated vascular, metabolic or cardiovascular disorders.
Our patient underwent laboratory testing following correspondence with the general internist and was found to have treatable hypercholesterolemia. Patients should be aware that, despite effective local treatment, recurrences can and often do occur. Likewise, patients must understand that all surgical treatment modalities have the potential for complications such as persistent erythema, hypo- or hyperpigmentation, scarring and ectropion.16,17
Dr. Gurwood thanks Al Kabat, OD and Alice Lim, OD, for their contributions to this case.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Zak A, Zeman M, Slaby A, Vecka M. Xanthomas: Clinical and pathophysiological relations. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(2):181-8. 2. Kim J, Kim YJ, Lim H, Lee SI. Bilateral circular xanthelasma palpebrarum. Arch Plast Surg 2012;39(4):435-7. 3. Christoffersen M, Frikke-Schmidt R, Schnohr P, et al. Xanthelasmata, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study. Brit Med J 2011;343:d5497. 4. Wang H, Shi Y, Guan H, et al. Treatment of xanthelasma palpebrarum with intralesional pingyangmycin. Dermatol Surg. 2016;42(3):368-76. 5. Dey A, Aggarwal R, Dwivedi S. Cardiovascular profile of xanthelasma palpebrarum. Biomed Res Int. 2013;2013:932863. 6. Nair PA, Patel CR, Ganjiwale JD, et al. Xanthelasma palpebrarum with arcus cornea: A clinical and biochemical study. Indian J Dermatol. 2016;61(3):295-300. 7. Esmat S, Abdel-Halim MR, Fawzy MM, et al. Are normolipidaemic patients with xanthelasma prone to atherosclerosis? Clin Exp Dermatol. 2015;40(4):373-8. 8. Napper G, Douglas I, Albietz J. Ocular therapeutics. Clin Exp Optom. 2007;90(3):212-3. 9. Labandeira J, Vázquez-Osorio I, Figueroa-Silva O, et al. Tolerability and effectiveness of liquid nitrogen spray cryotherapy with very short freeze times in the treatment of xanthelasma palpebrarum. Dermatol Ther. 2015;28(6):346-50. 10. Plensdorf S, Martinez J. Common pigmentation disorders. Am Fam Physician. 2009;79(2):109-16. 11. Sansalone K, Beer K, Pavlis J. Effective treatment of xanthelasma. J Drugs Dermatol. 2016;15(7):891-2. 12. Dincer D, Koc E, Erbil AH, Kose O. Effectiveness of low-voltage radiofrequency in the treatment of xanthelasma palpebrarum: a pilot study of 15 cases. Dermatol Surg. 2010;36(12):1973-8. 13. Corradino B, Di Lorenzo S, Triolo A, Moschella F. Laser treatment of giant xanthelasma palpebrarum. Lasers Med Sci. 2015;30(8):2205-7. 14. Pathania V, Chatterjee M. Ultrapulse carbon dioxide laser ablation of xanthelasma palpebrarum: a case series. J Cutan Aesthet Surg. 2015;8(1):46-9. 15. Shields CL, Mashayekhi A, Shields JA, Racciato P. Disappearance of eyelid xanthelasma following oral simvastatin (Zocor). Br J Ophthalmol. 2005;89(5):639-40. 16. Lee HY, Jin US, Minn KW, Park YO. Outcomes of surgical management of xanthelasma palpebrarum. Arch Plast Surg. 2013;40(4):380-6. 17. Park EJ, Youn SH, Cho EB, et al. Xanthelasma palpebrarum treatment with a 1,450-nm-diode laser. Dermatol Surg. 2011;37(6):791-6. |

