Practical Matters in Myopia Management - 3rd EditionWith an expanding arsenal of information, myopia can be a puzzling area of care. In this third annual Review of Optometry supplement, experts offer solutions backed by science to help you manage this growing patient population. Click here to download a PDF or here to read the digital edition. Check out the other articles featured in this supplement: |
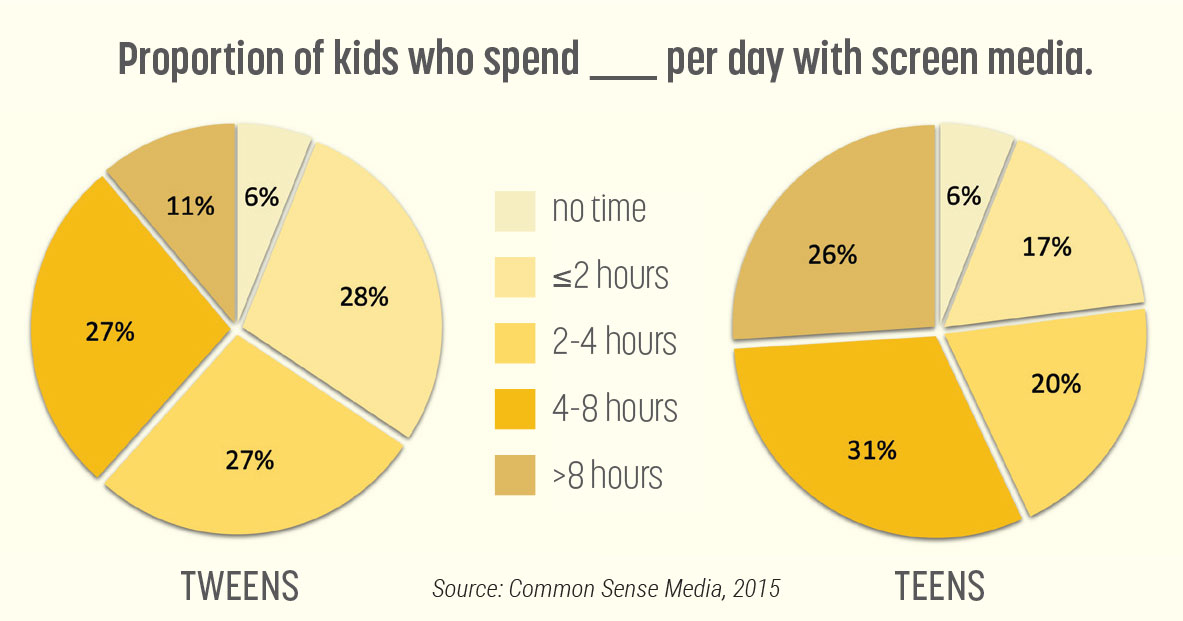
The time we spend on screens of all kinds is increasing, for all ages of the population. Electronics are integral to our educational, career and social lives. According to the 2015 Common Sense Census about media use by tweens and teens, children between the ages of eight and 12 use almost five hours a day of screen media while those 13 to 18 years old average a little over six and a half hours of screen media a day.1 There is also a shift away from viewing media on a television to more time on mobile devices—with their closer viewing distances.1
It’s up to us, as primary eyecare providers, to know about and discuss the risks of these devices as well as their proper use.
Hazards of Screen Use
There has been a lot of discussion about the potential dangers of blue light. Why blue light specifically? If we think back to the way energy and wavelength relate, they have an inverse relationship: the lower the wavelength, the higher the energy.2 The spectral profiles of sunlight and electronic screens are very similar, both emitting a high amount of short-wavelength light.3 When this high energy light hits the photoreceptors and retinal pigment epithelium (RPE), the ensuing reaction leads to photochemical damage and deformation of proteins and DNA in the retina.4,5 Studies have shown that 400nm to 435nm blue light destroys the mitochondria of cultured human RPE cells.6
However, we have to recall that we have protective elements in the retina such as macular pigment and melanin, both of which absorb high-energy light and act as antioxidants.7,8 While we have research like the Beaver Dam Eye Study showing a correlation between sun exposure from your teens to your 30s leading to development of macular degeneration, other studies (e.g., the Eye Disease Case-Control Study Group) show a lack of correlation.9-12 A 2016 study noted that “comparing natural exposures with the reasonably foreseeable exposure to optical radiation from lamps, computer screens and mobile devices, such as smartphones, shows that the actual spectrally weighted irradiance is lower than the natural exposures.” The researchers went on to say that “under even extreme long-term viewing conditions, none of the assessed sources suggested cause for concern for public health.”13
So, where is the bigger concern with electronics? It is twofold: (1) visual stress and (2) disruption of circadian rhythms and sleep. Habitual performance of screen-viewing behavior can lead to computer vision syndrome (CVS), disrupt accommodative and binocular function, and be a catalyst for myopia progression.
Digital eyestrain. CVS is a group of ocular- and vision-related problems that result from prolonged digital device use. Female sex, improper body posturing and ergonomics, long duration of use without proper breaks and short working distance are associated with increased odds of CVS.14 The most common symptoms, experienced by 64% to 90%, are headache, neck and back pain, eye strain, eye pain, eye irritation, vision blur, diplopia, dry eye, burning and tearing.15
Sleep disruption. Smartphone use in the dark suppresses melatonin production. Melatonin, produced in the pineal gland in response to darkness, helps with timing of your circadian rhythm sleep-wake cycle. It naturally rises in the evening, putting you into a state of quiet wakefulness that helps promote both falling and staying asleep. The closer the working distance, the brighter the screen and the brighter the general room illumination, the higher the suppression of melatonin production will be.16 Electronic book use before bed has been shown to suppress melatonin production, delay the onset of sleep and cause sleepiness the following day compared to reading a paper book.17
Myopia. Development and progression of myopia stems from the interplay of genetics, peripheral retinal defocus, accommodative demands, binocularity, higher-order aberrations, circadian rhythms, light intensity, spectral composition and overstimulation of retinal OFF pathways.18 The relationship between accommodative demand, binocularity and myopia is complex and not fully understood.
Fifteen cross-sectional studies have investigated the relationship between near work activities and prevalence of myopia.19 Ten of them showed that more near-work activities increase prevalence of myopia in children aged six to 18 years. Eight longitudinal studies demonstrated a relationship between near-work activities and progression of myopia. They concluded that near-work activities were a risk factor for myopic progression.19
 |
| Click image to enlarge. |
Juvenile myopia may result from a breakdown in the emmetropization process in susceptible children.18 Axial growth is influenced by visual experience (retinal image quality and optical defocus). Myopes display unusually high levels of aberration and larger accommodative lags relative to those who remain emmetropic. Chronic retinal defocus at near (due to accommodative lag) possibly triggers a series of biochemical events that result in scleral remodeling and axial elongation in an attempt to improve image clarity.20 The peripheral retina in myopes is more sensitive to hyperopic defocus than emmetropes. Any peripheral retinal blur over ±1.00D is likely to be perceived as defocused and could disrupt the emmetropization process in a child.21
In outdoor environments, objects are typically further away and there is less dioptric variation across the visual stimuli, reducing accommodative demand. We typically also have higher illumination, causing more miosis and leading to greater depth of focus. The pupil acts as an aperture stop—when enlarged, optical image properties (retinal image blur, higher-order aberrations, depth of focus, accommodative lag) could contribute to myopia progression in susceptible individuals.20,21
Myopes show reduced stereopsis and greater binocular imbalance vs. emmetropes.22,23 Myopic children have a higher AC/A ratio vs. emmetropes and the ratio can be elevated as far as four years before myopia onset.24 AC/A reaches its peak at myopia onset and remains raised through at least five years after myopia onset.25 Children with higher AC/A ratios have a 20-fold increased risk of myopia development within one year.26,27
A study done by Goss evaluated initially emmetropic children who had eye and vision examinations at six-month intervals for a period of three years.28 Distance phorias were not significantly different between emerging myopes and those who remained emmetropic. Near phorias, however, were found to be more convergent (eso) in the became-myopic group, associating the onset of myopia with an eso shift in the near phoria. The children in the remaining-emmetropic group did not show eso shifts in near phoria. In the became-myopic group, near phoria showed an eso shift beginning before and continuing after the onset of myopia.
How to Help
So, what can we recommend to help our patients? There have been a lot of ads for blue-blocking tints and antireflective coating to help fight against the “dangers of blue light.” In reality, these tints and coatings theoretically reduce the calculated phototoxicity by just 10.6% to 23.6%, decrease melatonin suppression by 5.8% to 15.0% and show no change in circadian rhythms or contrast sensitivity vs. clear lenses.29,30 In a double-masked study evaluating blue-blocking lenses’ impact on CVS, the intervention was “found not to alleviate symptoms or signs of eye strain associated with computer use, compared to non-blue blocking (clear) lenses.”31 A meta-analysis of the effect of blue-light blocking spectacle coatings and tints on visual performance, macular health and the sleep-wake cycle found that they did not improve computer eye strain or fatigue, did not improve sleep quality, did not enhance contrast sensitivity and showed no evidence of preserving macular health.32
“Warm” filters that attach on top of a computer screen, on the other hand, block more blue light than blue-blocking spectacles, reduce overall illuminance and do a better job preventing electronic screens from suppressing melatonin production. Night-mode functions in smartphones also have value, with one study showing reduced melatonin suppression values by up to 93%.33 A simple alternative is turning down the brightness of the device itself, and in fact may be needed for optimal effect. A study looking at placing the iPad into night shift mode and the effect on melatonin suppression found that “adjusting a self-luminous display’s spectral composition without adjusting its brightness setting may be insufficient for avoiding adverse impacts on melatonin secretion and circadian system.”34
A recent study upheld the belief that evening exposure to light affects the circadian clock, sleep and alertness.35 The team investigated whether mechanisms of color vision, specifically on the blue-yellow axis, affect the human circadian system and sleep differently. Participants were exposed to three different light scenarios for one hour starting 30 minutes after habitual bedtime: baseline control lighting (93.5 photopic lux), intermittently flickering (1 Hz, 30s on–off) yellow-bright light (123.5 photopic lux) and intermittently flickering blue-dim light (67.0 photopic lux). All the light stimuli were calibrated to have equal melanopsin excitation. The researchers found no differences between the three lighting conditions (white, blue, yellow lighting) regarding circadian melatonin phase delays, melatonin suppression, subjective sleepiness, psychomotor vigilance or sleep.
We should be discussing proper device use with all our patients whether we are more concerned with myopia development and progression in the pediatric population or computer vision syndrome and circadian rhythm disruption in patients of all ages. Here are some of the points I discuss with my patients:
Evaluate for and manage vision dysfunction. A full comprehensive evaluation and management of dry eye, uncorrected refractive error and ocular motilities can be integral to a patient’s visual function and comfort. The OD should discuss and offer the full scope of treatments on a case by case basis including but not limited to: lubrication, medication, gland expression, intense pulse light, punctal plugs, trigeminal nerve stimulation, lenses, prisms, tints, coatings, binasal occlusion and vision therapy to ensure clear, comfortable, binocular vision and coordination of visual functional skills. If you do not offer a treatment in your office that a patient may benefit from, consider referring to an optometric colleague to help comanage the patient and return them to you for their annual evaluations.
 |
|
Testing binocular, accommodative and oculomotor function is always important but especially so in younger patients as we evaluate the potential of digital device use to be a catalyst for myopia development. Click image to enlarge. |
Increase screen size, text size and viewing distance. Small screens tend to render text at small point sizes, prompting the viewer to reduce the working distance. Inform the patient that they should use the largest screen possible and sit as far away as possible when viewing electronics. A large phone is better than small one, a tablet is better than a phone, a monitor is better than a tablet and a TV screen viewed from across the room is even better. This increase in diameter and, more importantly, viewing distance decreases the visual demand. If they like to watch videos on their phone, have them switch to casting it onto the TV. These small changes in habit can be easy to implement and can provide a significant benefit.
Take the work outside. Outdoor time has overwhelming health and vision benefits. It can be difficult to get time outdoors when you spend all day at school or work and then have homework or follow-up work to do. I recommend that, whenever possible, the patient take their homework or work outside. Even though it would be ideal for them to be out and about engaging in play and physical activity, at least this way they reap the benefits of the sun before it sets for the day. Across multiple studies, it has been shown that spending about 13 hours/week (two hours/day) outdoors decreases the likelihood of myopia development.36
 |
|
Children should spend at least two hours per day outside to help decrease the likelihood of myopia development. Click image to enlarge. |
Ergonomic setup of the computer monitor. The chair and desk should be set up so that the patient’s feet are both flat on the floor, knees are bent in a 90° to 110° angle, the chair backrest supports the lower back and the forearms are parallel to the floor.36 It is more comfortable to view a computer screen when the eyes look downward because we usually converge when we look down, not straight ahead. A computer monitor should sit about 24 to 33 inches from the eye (depending on size) and the top of the computer screen should be at eye level with the center of the computer about 15 to 20 degrees below eye level.37
Ideally, there should be no head movement needed to view any portion of the screen. Position the screen to avoid glare, particularly from overhead lighting or windows. Blinds, drapes and lower-wattage lights can be used or a screen filter can be used to both decrease the glare as well as brightness of the screen.
Peripheral screen stickers. Placing a bright sticker on all four corners of the monitor can help keep a patient from over-converging or over-accommodating. Having the patient be mindful and aware of the four stickers as they are doing their work can help them be more aware of their periphery and not lock in centrally.
 |
|
Teach patients about the proper ergonomic positioning needed during extended computer use. In this photo, you can also see the placement of stickers at each corner of the screen to help promote peripheral awareness and prevent over-accommodation. Click image to enlarge. |
Hydration and blinking. Whenever we are doing something visually stimulating or cognitively challenging, whether on electronics or paper, our blink rate decreases. This can lead to dryness, eye irritation and contact lens intolerance.38 Hydration as well as intentional blinking, just like purposefully being aware of the four corner stickers in the periphery, can help decrease the sensation of dry eyes.
Rest breaks with an alarm. Visual and postural breaks are critical. It can be hard to remember to take a break, so I have my patients set a repeating timer on their phone. If they can’t agree to every 20 minutes, we make a deal for every 30 minutes. While getting them to look out a window for 20 seconds is beneficial, I prefer to have them actually get up and out of the chair to relax their body as well as their eyes. For the adults, I have them do neck, shoulder and back stretches while looking at a distance, for the little kids I give them fun activities such as jump like a frog or walk like a duck, and for the teenagers I have them agree on some quick and simple chores like pick up three pieces of clothing off your floor and throw them in the hamper or put two things away that are sitting on the kitchen counter. Giving each individual an activity to do during the break and setting a reminder alarm helps give their eyes, body and mind a break.
Tech-free bedroom. Bedrooms should be an electronics-free zone.39 Ideally, there should be no TV and charging station in the bedroom. If your patients charge their phone or tablet in the bedroom, they are much more likely to sneak a peek or just use it wholesale. It’s best to set up a nighttime charging station somewhere in the house outside of the bedrooms, so that all electronics get charged there overnight, starting one hour before bedtime. If there is a computer in the child’s bedroom, it may be warranted to ask the parents to remove the power cable from the room so there is no temptation to turn it on. If electronics must be used within one hour before bedtime, make sure the patient turns on night mode and, more importantly, reduces the brightness on the screen.
Peaceful Coexistence
Electronic use is not going away. It is tied into our everyday lives, whether we want it or not, starting from a very young age. Much of childhood education is shifting to digital formats in the classroom and for homework, more and more socializing happens online and, as a society, we are becoming increasingly interlinked through the digital world. It may not be feasible to fully restrict electronics but we can set reasonable limitations that minimize the detrimental effects while allowing our patients to reap the benefits of the digital world.
Dr. Petrosyan is an associate clinical professor at SUNY College of Optometry and East New York Diagnostic and Treatment Center. She is on the board of the Optometric Extension Program Foundation, is a vision therapy and rehabilitation workbook creator through Bernell, and is helping introduce optometry and comprehensive pediatric eye care to Armenia through the Armenian EyeCare Project.
1. The Common Sense Census: Media use by tweens and teens: common sense media, 2015. eMarketer. 2. Schwartz S. Visual Perception: A Clinical Orientation. Fourth Edition. McGraw Hill Professional. 2009. 3. Gringras P, Middleton B, Skene DJ, Revell VL. Bigger, brighter, bluer-better? Current light-emitting devices – adverse sleep properties and preventative strategies. Front Public Health. 2015;2:233. 4. Wiegand RD, Giusto NM, Rapp LM, Anderson RE. Evidence for rod outer segment lipid peroxidation following constant illumination of the rat retina. Invest Ophthalmol Vis Sci. 1983;24(10):1433-5. 5. Beatty S, Koh H, Phil M, Henson D, Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2000;45(2):115-34. 6. Youn HY, Chou BR, Cullen AP, Sivak JG. Effects of 400 nm, 420nm, and 435.8nm radiations on cultured human retinal pigment epithelial cells. J Photochem Photobiol B Biol. 2009;95(1):64-70. 7. Suárez-Barrio C, del Olmo-Aguado S, García-Pérez E, et al. Antioxidant role of PRGF on RPE cells after blue light insult as a therapy for neurodegenerative diseases. Int J Mol Sci. 2020; 21(3):1021. 8. Zareba M, Skumatz CM, Sarna TJ, Burke JM. Photic injury to cultured RPE varies among individual cells in proportion to their endogenous lipofuscin content as modulated by their melanosome content. Invest Ophthalmol Vis Sci. 2014;55(8):4982-90. 9. Tomany SC, Cruickshanks KJ, Klein R, Klein BE, Knudtson MD. Sunlight and the 10-year incidence of age-related maculopathy: the Beaver Dam Eye Study. Arch Ophthalmol. 2004;122(5):750-7. 10. McCarty CA, Mukesh BN, Fu CL, Mitchell P, Wang JJ, Taylor HR. Risk factors for age-related maculopathy: the visual impairment project. Arch Ophthalmol. 2001;119(10):1455-62. 11. Delcourt C, Carrière I, Ponton-Sanchez A, et al. Light exposure and the risk of age-related macular degeneration: the Pathologies Oculaires Liées à L’age (POLA) Study. Arch Ophthalmol. 2001;119(10):1463–1468. 12. Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL 3rd; Age-Related Eye Disease Study Research Group. Risk factors for the incidence of advanced age-related macular degeneration in the age-related eye disease study (AREDS) AREDS report no. 19. Ophthalmology. 2005;112(4):533-9. 13. O’Hagan JB, Khazova M, Price LL. Low-energy light bulbs, computers, tablets, and the blue light hazard. Eye (Lond). 2016;30(2):230-3. 14. Lema AK, Anbesu EW. Computer vision syndrome and its determinants: a systematic review and meta-analysis. SAGE Open Med. 2022;10:20503121221142402. 15. Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31(5):502-15. 16. Oh JH, Yoo H, Park HK, Do YR, et al. Analysis of circadian properties and healthy levels of blue light from smartphones at night. Sci Rep. 2015;5:11325. 17. Chang AM, Aeschbach D, Duffy JF, Czeisler CA, et al. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci USA. 2015;112(4):1232-7. 18. Németh J, Tapasztó B, Aclimandos WA, et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur J Ophthalmol.. 2021;31(3), 853-83. 19. Huang H-M, Chang DS-T, Wu P-C (2015) The association between near work activities and myopia in children—a systematic review and meta-analysis. PLoS One 10(10): e0140419. 20. Nicola S. et al. IMI Accommodation and binocular vision in myopia development and progression. Invest. Ophthalmol. Vis. Sci. 2021;62(5):4. 21. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-60. 22. Maiello G, Walker L, Bex PJ, Vera-Diaz FA. Blur perception throughout the visual field in myopia and emmetropia. J Vis. 2017;17(5):3. 23. Vera-Diaz FA, Bex PJ, Ferreira A, Kosovicheva A. Binocular temporal visual processing in myopia. J Vis. 2018;18(11):17. 24. Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A ratio, age, and refractive error in children. Invest Ophthalmol Vis Sci. 2000;41(9):2469-78. 25. Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom Vis Sci. 2005;82(4):273-8. 26. Mutti DO, Mitchell GL, Jones-Jordan LA, et al; CLEERE Study Group.. The response AC/A ratio before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2017;58(3):1594-1602. 27. Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A ratio, age, and refractive error in children. Invest Ophthalmol Vis Sci. 2000;41(9):2469-78. 28. Goss DA, Jackson TW. Clinical findings before the onset of myopia in youth: 3. Heterophoria. Optom Vis Sci. 1996;73(4):269-78. 29. Leung TW, Li RW, Kee CS. Blue-light filtering spectacle lenses: optical and clinical performances. PloS One. 2017;12(1):e0169114. 30. Mainster MA. Violet and blue light blocking intraocular lenses: photoprotection versus photoreception. Br J Ophthalmol. 2006 Jun;90(6):784-92. 31. Singh S, Downie LE, Anderson AJ. Do blue-blocking lenses reduce eye strain from extended screen time? A double-masked randomized controlled trial. Am J Ophthalmol. 2021;226:243-51. 32. Lawrenson JG, Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: a systematic review of the literature. Ophthalmic Physiol Opt. 2017;37(6):644-54. 33. Teran E, Yee-Rendon CM, Ortega-Salazar J, et al. Evaluation of two strategies for alleviating the impact on the circadian cycle of smartphone screens. Optom Vis Sci. 2020;97(3):207-217. 34. Nagare R, Plitnick B, Figueiro MG. Does the iPad night shift mode reduce melatonin suppression? Light Res Technol. 2019;51(3):373-383. 35. Blume C, Cajochen C, Schöllhorn I, Slawik HC, Spitschan M. et al. Effects of calibrated blue–yellow changes in light on the human circadian clock. Nat Hum Behav. 2024;8(3):590-605. 36. Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95(6):551-566. 37. Emerson S, Emerson K, Fedorczyk J. Computer workstation ergonomics: Current evidence for evaluation, corrections, and recommendations for remote evaluation. J Hand Ther. 2021;34(2):166-78. 38. Chu CA, Rosenfield M, Portello JK. Blink patterns: reading from a computer screen versus hard copy. Optom Vis Sci. 2014;91(3):297-302. 39. Fuller C, Lehman E, Hicks S, Novick MB. Bedtime use of technology and associated sleep problems in children. Glob Pediatr Health. 2017;4:2333794X17736972. |

