 |
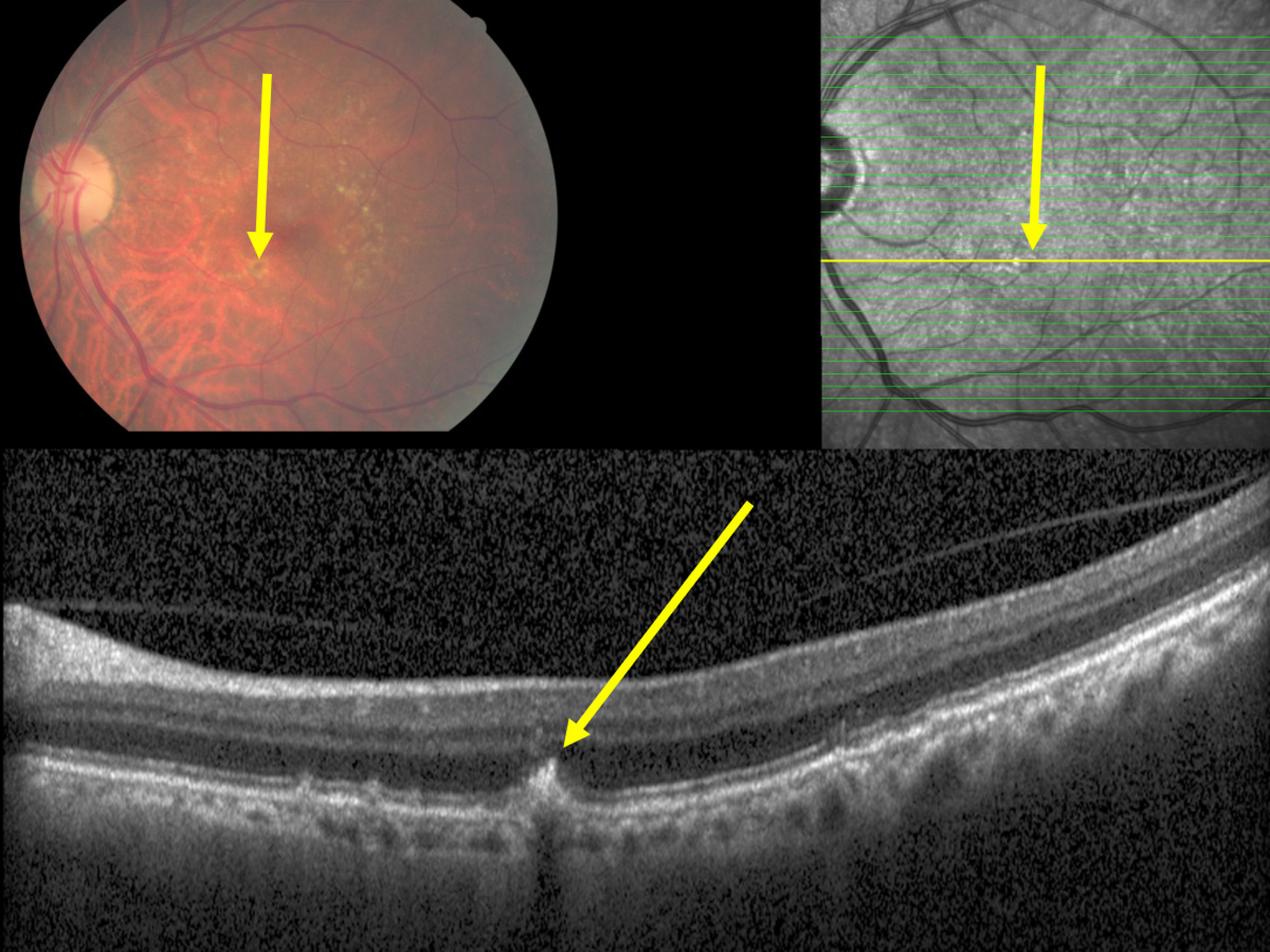
A correlation between intraretinal hyperreflective bodies and spatially correlated defects in the ellipsoid zone and ELM also corresponded to the finding obtained in the histologic part of the same study, in which intraretinally located RPE cells were spatially correlated with defects in the ELM. This image from the study shows macular hyperpigmentation (yellow arrow) corresponding to a plume-like intraretinal hyperreflective body in the outer nuclear layer (yellow arrow), apparently emerging out of the RPE line, with a corresponding localized defect in the inner segment/outer segment line and defect in the outer external limiting membrane. Photo: Panda-Jonas S, et al. Ophthalmol Sci. September 30, 2024. Click image to enlarge. |
Retinal pigment epithelium (RPE) changes are considered indicators of age-related macular degeneration (AMD). RPE cell loss signals the development of geographic atrophy in the late stage of AMD, and RPE cell proliferations in the subretinal space between the retina and Bruch’s membrane do the same for the neovascular or wet form of AMD. Increasing the available information about intraretinal hyperreflective bodies and intraretinally migrated retinal pigment epithelium cells may expand the knowledge about the pathogenesis of AMD in general and about the role of intraretinally migrated RPE cells in particular. Researchers in Germany examined the occurrence and spatial correlations of intraretinal hyperreflective bodies and macular hyperpigmentations as a potential surrogate of intraretinally located RPE cells on OCT images and fundus photographs obtained in a population-based study. Their study, published in Ophthamology Science, found that macular hyperpigmentations in eyes with intermediate and late AMD were usually associated with intraretinal hyperreflective bodies, which according to their shape and according to histological studies represent migrating/proliferating RPE cells. The hyperreflective bodies also correlated histologically with intraretinally located (migrated) RPE cells and corresponded spatially with localized defects of the ellipsoid zone and the external limiting membrane (ELM).
The study used OCT-based and fundus photography-based examination of the macula of the Beijing Eye Study participants, as well as light-microscopical histomorphometry of enucleated human eyes. In the Beijing Eye Study (6,551 eyes; 3,301 participants), prevalence of intermediate AMD and late AMD was 5.1% and 0.6%, respectively.
All 42 eyes with intermediate AMD and macular hyperpigmentation had intraretinal hyperreflective bodies at locations corresponding spatially with macular hyperpigmentations on the fundus photographs. Among all eyes with intermediate AMD (n=331), intraretinal hyperreflective bodies were detected in 262 (79.2%) eyes. The most internal location of the intraretinal hyperreflective bodies was at the ellipsoid zone in 46 (13.9%) eyes, at the external ELM in 45 (13.6%) eyes, and in the outer nuclear layer in 145 (43.8%) eyes. Out of the 262 eyes with intraretinal hyperreflective bodies, 186 (71.0%) eyes showed a corresponding defect in the ellipsoid zone, and 128 (48.9%) eyes showed a defect in the ELM. The eyes with an intraretinal hyperreflective body located beneath the ELM did not show an ELM defect. The intraretinal hyperreflective bodies were associated with a plume-like appearance and with a smoke-like appearance in 20 (7.6%) eyes and 137 (52.3%) eyes, respectively. All intraretinal hyperreflective bodies did not have a shadow on the OCT images. Similar findings were obtained in the eyes with late AMD.
Among 237 enucleated eyes examined histologically, 21 globes showed intraretinally migrated retinal pigment epithelium cells: eight eyes in parapapillary alpha zone/beta zone, five eyes with myopic patchy atrophies and three eyes with AMD. The intraretinally migrated retinal pigment epithelium cells were spatially associated with an ELM defect and were not surrounded by a basal membrane.
“The histological part of the study demonstrated the intraretinal location of RPE cells in eyes with AMD and other diseases, and all of these intraretinally migrated retinal pigment epithelium cells were spatially associated with defects in the ELM,” the researchers wrote in their paper. “The findings suggest that RPE cell migration into the retina is a hallmark of intermediate or late AMD, in particular in eyes with macular pigmentations.”
The study noted that these observations suggest that the ELM (and the ellipsoid zone) may act as a migration barrier for subretinal RPE cells.
“The finding of intraretinally located RPE cells in eyes with intermediate and late AMD also raises the question whether in the intermediate and late stages of AMD the disease affects not only the subretinal compartment and photoreceptor layer but also the middle retinal layers, including the inner nuclear layer,” the researchers proposed.
“The high prevalence of intraretinal hyperreflective bodies in eyes with intermediate AMD may imply that intraretinal hyperreflective bodies should be actively searched for in routinely taken OCT images of the macula in patients with AMD,” they concluded. “It holds true in particular since the risk of progression from intermediate AMD to late AMD has been shown to be associated with the distribution and extent of intraretinal hyperreflective bodies, especially in the outer retinal layer.”
| Click here for journal source. |
Panda-Jonas S, Jonas RA, Xu J, et al. Intraretinal retinal pigment epithelium cells in age-related macular degeneration. Ophthalmol Sci. September 30, 2024. [Epub ahead of print] |


