 |
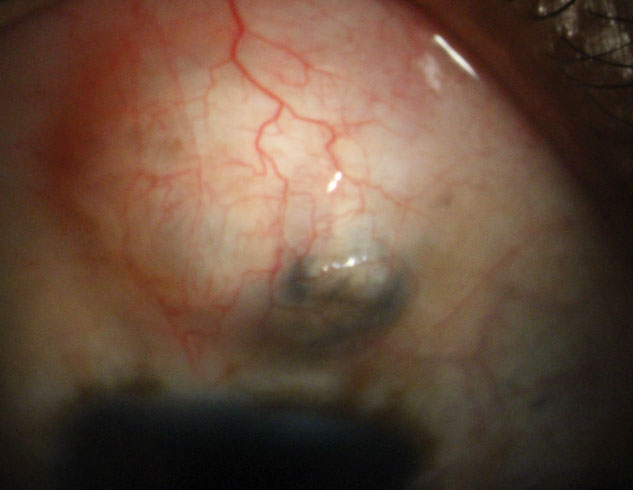
Trabeculectomy may require additional surgery and cause further complications for patients of African ancestry. In this study, 18 eyes required further intervention within one year of surgery, which included bleb revision, glaucoma drainage tube implant and scleral interventions. Photo: Justin Schweitzer, OD. Click image to enlarge. |
For glaucoma patients who cannot be adequately managed with medications and/or SLT, trabeculectomy is a likely next step. Despite the highly invasive nature of the procedure, it has been shown to have a high long-term success rate.1 Unfortunately, not every patient experiences optimal results. For instance, Black patients are more likely to undergo glaucoma surgery and progress to severe stages of their disease compared to white patients.2 This results in further complications after surgery for Black patients, especially after trabeculectomy surgery.
Researchers from the University of Pennsylvania recently published findings in the Journal of Glaucoma on the outcomes of trabeculectomy in primary open-angle glaucoma patients of African descent. They enrolled a total of 63 eyes and performed the surgery in 55 POAG cases. Each patients’ intraocular pressure, visual acuity, visual field and medication usage were all recorded pre- and postoperatively. Additionally, the researchers observed all complications that arose within one year after surgery.
Trabeculectomy was successful for a proportion of the study’s population. Less than half—just 46%—of patients had a successful treatment without need for medication intervention, and approximately 22% of patients had the “qualified” success that entailed continuance of a drug regimen postoperatively.3 The remainder of patients’ surgeries failed (32%) and their cases needed further surgical intervention.
“Complications were observed in 58.7% of patients, with additional surgery, bleb leak and hypotony being the most common issues,” wrote the researchers in their paper on the study. “In contrast to the successful and qualified successful groups, younger age at surgery and a positive family history of glaucoma were associated with surgical failure.” They noticed a significant worsening of visual field parameters coupled with a decline to patients’ visual acuity. They noted that their findings were similar to those reported in previous studies. However, they had no clear explanation for why most of these eyes lost vision.
Although complications arose and patients’ vision worsened, other measurements observed in the study were positive. Overall, intraocular pressure was reduced by 46%, and the use of daily glaucoma medications and eye drops dropped as well (73% and 67% reduction).
“While trabeculectomy demonstrates positive outcomes, including substantial reductions in IOP and medication, these findings underscore the complexities of trabeculectomy outcomes in African ancestry populations and highlight the need for precision-based approaches to glaucoma management,” concluded the researchers in the paper on this study.
| Click here for journal source. |
1. Wagner FM, Schuster AK, Kianusch K, et al. Long-term success after trabeculectomy in open-angle glaucoma: results of a retrospective cohort study. BMJ Open. 2023;13:2:e068403. 2. Lee RH, Lee RK, Pasquale LR. Burden of Trabeculectomy and Glaucoma Drainage Implantation after Laser Trabeculoplasty: A Two-Year Follow-up Study. Ophthalmol Glaucoma. 2022;5(1):58-66. 3. Mamidipaka A, Shi A, Addis V, et al. Outcomes of trabeculectomy and predictors of success in patients of African ancestry with primary open angle glaucoma. Journal of Glaucoma. October 2, 2024. [Epub ahead of print]. |


