A large study recently published in the journal Retina offers new insights into visual outcomes and the development of neovascular AMD (nAMD) among eyes with geographic atrophy (GA). The findings revealed a general decline in the mean visual acuity (VA) by two to three lines over the three-year study period, with poorer outcomes observed in patients older than 86 and/or with moderate visual impairment. Patients whose fellow eye was affected by nAMD also showed more rapid progression.
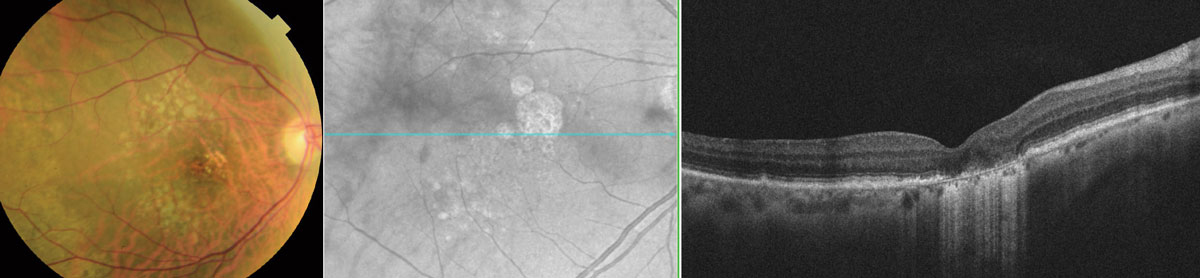 |
| Patients with geographic atrophy in this study lost, on average, two to three lines of visual acuity over the three-year follow-up period. Photo: Wendy Harrison, OD, PhD. Click image to enlarge. |
The retrospective study reviewed medical records from 18,712 eyes with dry AMD and newly diagnosed GA who had at least three years of follow-up data on file. The mean patient age at baseline was 79 years, and 66% of the cohort was female. Data was assessed at initial GA presentation and roughly six, 12, 24 and 36 months of follow-up.
The initial mean VA was 20/45. Over three years, 18.9% of the eyes studied developed nAMD. The rate of developing neovascularization was more than double in eyes where the fellow-eye had nAMD compared to those with fellow-eye GA, with a relative risk of 2.34. For eyes that did not develop nAMD, there was a decline in VA by an average of 12.4 letters within 36 months.
By the end of the three-year study period, 70% of eyes had vision below the threshold required for driving (VA of 20/40 or worse), 42% had low vision (VA of 20/70 or worse) and 23% were classified as legally blind (VA of 20/200 or worse).
Two factors independently linked to a faster decline in VA and poorer outcomes among GA patients were older age and a moderate baseline visual impairment (VA between under 20/40 and 20/100). The eyes with both factors—belonging to the oldest age group (≥86 years) and with moderate visual impairment—experienced notably poor outcomes, losing an average of 19.7 letters within three years.
The youngest age group (≤74 years) fared better than older patients with GA in terms of visual outcomes, with 54% maintaining driving vision at 36 months of follow-up, and only 14% progressing to legal blindness. Conversely, in the oldest age group, only 17% of eyes maintained VA ≥20/40 throughout follow-up, and 55% had low vision.
In their paper, the researchers note how it’s interesting that patients with moderate visual impairment lost more lines of acuity on average than those with severe, or minimal, visual impairment. “These findings may reflect progression from juxtafoveal to subfoveal GA in eyes with moderate visual impairment at index, as well as a floor effect among patients with severe visual impairment,” they proposed.
This data emphasizes the significant burden and lack of independence many patients with GA face, even as soon as months or a year after diagnosis. The researchers point out that older patients and those with moderate visual impairment “may especially benefit from early interventions to slow disease progression and preserve visual acuity.” Additionally, given that nearly 19% of eyes with GA progressed to nAMD within three years, and nAMD in the fellow eye increased this risk two-fold, they suggested that “patients diagnosed with GA ought to receive long-term surveillance for vision-threatening exudation, particularly those with a history of nAMD in the fellow eye.”
Looking forward, the study authors concluded, “Further research into early therapeutic interventions may enhance our ability to prevent blinding outcomes in GA and preserve quality of life in this vulnerable patient population.”
| Click here for journal source. |
Shughoury A, Boucher N, Aggarwal N, Ciulla TA. Three-Year Clinical Outcomes in Geographic Atrophy: An Analysis of 18,712 Patient Eyes. Retina. October 1, 2024. [Epub ahead of print]. |


