 |
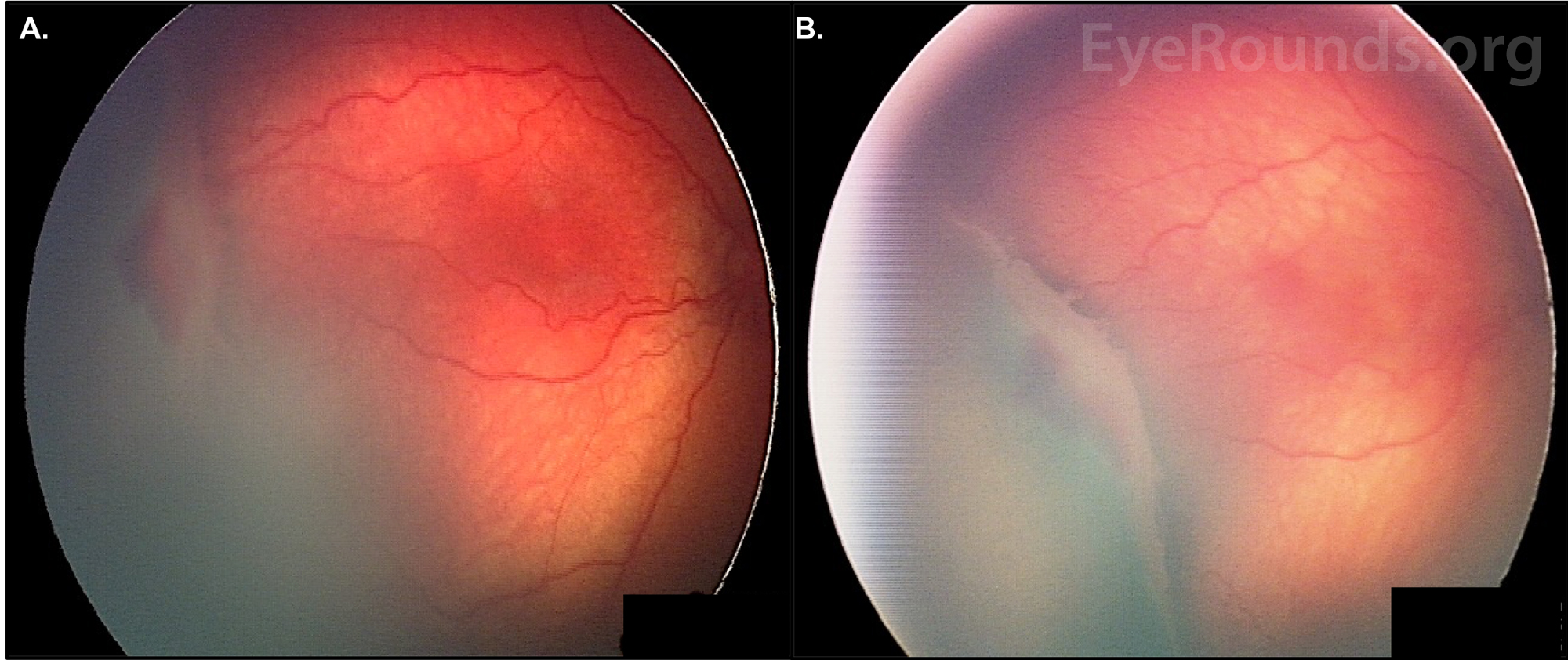
California statewide initiatives to improve oxygen management may have contributed to the decreasing ROP incidence. As well, while screening for ROP remained steady in California over this period, improved screening on a national level may have been a driver of the increasing trend for ROP incidence in the entire country. Photo: University of Iowa/www.eyerounds.org. Click image to enlarge. |
Using data from a large cohort of NICUs across the state, a newly published study in JAMA Ophthalmology updates current shifts in prevalence of retinopathy of prematurity (ROP) specific to California. Since 2003, ROP incidence has been increasing, and researchers from Stanford and the University of California believe that understanding the progression of and racial disparities within ROP incidence in their state may provide a useful perspective to guide practice in management and prevention of the condition.
Screening and incidence of ROP was observed for large-scale changes from the beginning of 2012 until the end of 2021, with inclusion of 39,269 very preterm infants (defined as less than 32 weeks’ gestational age or less than 1,500g) who were admitted to 60 neonatal intensive care units in the state.
Of the entire cohort, mean gestational age was 28.6 weeks, with a mean birth weight of 1,075g; 48.6% of all infants were female. The race of mothers who gave birth to these infants were 12.6% Asian, 13.3% Black, 44.9% Hispanic, 0.7% Native American/Alaskan, 24.7% non-Hispanic white and 1.0% Pacific Islander. In the 10-year span, ROP screening rates in California for eligible infants less than 30 weeks’ gestational age remained steady at 95% for all races and ethnicities. Among all infants included, ROP incidence decreased in the same time frame from 31% to 29%, and incidence rates among Asian and Hispanic patients decreased the most quickly compared with other racial and ethnic groups, narrowing disparities. This is a marginal but significant improvement, still indicating that more must be done to avoid the severe disease.
Upon further discussion, the authors of the study relay that by 2021, only 100 of 2,834 infants born under 30 weeks and eligible for screening were not, making it a low 3.5%. Also of note were the decreasing rates of ROP in Asian and Hispanic infants, who had the highest rates in 2012. The finding of these decreased rates was independent of preterm birth rates, which are contrary to what’s been found in a broader US study. This prior investigation reported that ROP rates and racial/ethnic disparities increased in prevalence during this period at the national level, with a 4.6% incidence in 2003 or a 6.8% incidence in 2019.
In the cohort of infants in the JAMA Ophthalmology study, ROP was more prevalent among Asian, Hispanic, Native American/Alaskan and Pacific Islander infants and other races compared with white, non-Hispanic infants. Interestingly, there was also an observed increase in ROP prevalence among infants born to parents with lower maternal ages; this was unexpected, since greater maternal age is linked with lower birth weight and gestational age. This may be explained by the fact that ROP has been linked to socioeconomic status, and lower maternal age may act as an indication of socioeconomic status.
Due to the disparity seen in California’s incidence rates vs. the rest of the US, the authors note that “the reasons for contrasting trends in the rest of the US should be further investigated,” but add that “lessons from California ROP management may help improve ROP trends across the rest of the US.”
| Click here for journal source. |
Quinn MK, Lee HC, Profit J, Chu A. Trends in retinopathy of prematurity among preterm infants in California, 2012 to 2021. JAMA Ophthalmol. October 3, 2024. [Epub ahead of print]. |


