 |
A 77-year-old white male presented for an eye examination in November 2004. He complained of watering at times and blurred vision in both eyes. His medications included Bextra (valdecoxib, Pfizer), Lipitor (atorvastatin, Pfizer) and Cardura (doxazosin mesylate, Pfizer). He reported no allergies to medications.
The patient had been to the office previously, and a review of his record yielded some interesting moments.
The patient had been to the office previously, and a review of his record yielded some interesting moments.
Diagnostic Data
This patient initially presented to my office in January 2001, at age 74, after two different refractive surgeons rejected him for LASIK due to cataracts. He had been to several other eye doctors in the area in previous years. The patient was still interested in refractive surgery. At that time, his medications included Lipitor, Cardura and Celebrex (celecoxib, Pfizer).
Best-corrected visual acuity was 20/20- O.D. and 20/25- O.S. through hyperopic, astigmatic and presbyopic correction. Pupils were equal, round and reactive to light and accommodation with no afferent pupillary defect. A slit lamp examination of his anterior segments was unremarkable.
Intraocular pressure measured 24mm Hg O.D. and 18mm Hg O.S. Through dilated pupils, his lenses were characterized by early nuclear sclerosis with cortical spoking, consistent with his BCVA. His cup-to-disc ratios were 0.45 x 0.55 O.D. and 0.45 x 0.45 O.S. A moderate amount of peripapillary atrophy surrounded both discs; the atrophy was greater O.D. than O.S. The neuro-retinal rim in the right eye did not adhere to the ISNT (inferior-superior-nasal-temporal) rule. The neuroretinal rim in the left eye did conform to the ISNT rule, with the thickest neuroretinal rim located inferiorly, followed by superiorly, then nasally and finally temporally. His macular and peripheral retinal examinations were unremarkable.
I explained to the patient that he was at risk for glaucoma, especially in the right eye, and that further testing was warranted. He said that none of the other doctors that he had recently seen had told him anything about his risk for glaucoma, but that he only had cataracts.
He returned six weeks later for visual field testing, which was essentially normal O.U. Applanation tensions at that visit were similar to the first visit. We again discussed at length his risk for glaucoma. I asked him to return for follow up in four months, although I didnt walk him to the desk to get him scheduled.
When called four months later (June 2001) to confirm the follow-up visit, he rescheduled for two weeks further. When called to confirm that appointment, he cancelled and said he would call back at a later date to reschedule.
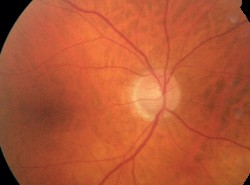 |
| Although he didnt seem to believe it, the patient had thinning of the neuroretinal rim. |
Diagnosis and Treatment
The patient presented again in November 2003 with complaints of decreased distance vision O.U. The decreased vision was ultimately found to be refractive in nature. IOP measured 24mm Hg O.D. and 19mm Hg O.S. Cupping had increased to 0.55 x 0.75 O.D. and 0.50 x 0.55 O.S. Laser polarimetry and stereo digital imaging of the optic nerves confirmed loss of neuroretinal rim tissue.
He was scheduled for field testing, which was completed in late November 2003. Field studies at this time clearly demonstrated paracentral scotomata in the arcuate regions above and below O.U.
We engaged in a lengthy discussion about the progressive nature of glaucoma, and I told him that intervention was necessary at this time. I prescribed Lumigan (bimatoprost, Allergan) 1 drop O.U. h.s. and asked him to return in two weeks to assess his clinical response.
When he returned two weeks later (December 2003), he had discontinued the Lumigan three days after initiation of therapy because it caused a foreign-body sensation. Again, we discussed the situation, and I stressed that the situation needed to be brought under control. I switched him to Xalatan (latanoprost, Pfizer) 1 drop O.U. and asked him to return in two weeks. When called to confirm that appointment (mid-December 2003), he canceled, stating that he was too busy and that he would call to reschedule.
He finally returned in November 2004 with complaints of blurred vision. He reported that he had discontinued the Xalatan a year earlier, about a week after beginning therapy. IOP at this visit measured 26mm Hg O.D. and 21mm Hg O.S. The cataracts remained the same, but the neuroretinal rims had further thinned.
The patient presented again in November 2003 with complaints of decreased distance vision O.U. The decreased vision was ultimately found to be refractive in nature. IOP measured 24mm Hg O.D. and 19mm Hg O.S. Cupping had increased to 0.55 x 0.75 O.D. and 0.50 x 0.55 O.S. Laser polarimetry and stereo digital imaging of the optic nerves confirmed loss of neuroretinal rim tissue.
He was scheduled for field testing, which was completed in late November 2003. Field studies at this time clearly demonstrated paracentral scotomata in the arcuate regions above and below O.U.
We engaged in a lengthy discussion about the progressive nature of glaucoma, and I told him that intervention was necessary at this time. I prescribed Lumigan (bimatoprost, Allergan) 1 drop O.U. h.s. and asked him to return in two weeks to assess his clinical response.
When he returned two weeks later (December 2003), he had discontinued the Lumigan three days after initiation of therapy because it caused a foreign-body sensation. Again, we discussed the situation, and I stressed that the situation needed to be brought under control. I switched him to Xalatan (latanoprost, Pfizer) 1 drop O.U. and asked him to return in two weeks. When called to confirm that appointment (mid-December 2003), he canceled, stating that he was too busy and that he would call to reschedule.
He finally returned in November 2004 with complaints of blurred vision. He reported that he had discontinued the Xalatan a year earlier, about a week after beginning therapy. IOP at this visit measured 26mm Hg O.D. and 21mm Hg O.S. The cataracts remained the same, but the neuroretinal rims had further thinned.
 |
| Of the services we provide, glaucoma tops the list. Dont be reticent to point out your specialty areas to patients. |
Discussion
Have you ever had a patient like this? Undoubtedly. So, how would you proceed?
Perhaps I had not done a sufficient job of explaining the severity of the visual outcome if he continued along the same path. So, I changed my usual discussion and essentially went directly to the point: He would become blind if not treated. When I said this to him, he rather abruptly said that he planned to get a second opinion. I wish he had done that two years earlier.
When I asked him whom he planned to see for the second opinion, he did not have any particular provider in mind, but he mentioned the two refractive surgeons he had seen prior to our first visit.
In some respects with this patient, I felt as though I was banging my head against the wall, and that maybe I should just let him seek help from whomever he chose. Still, I felt I had an obligation to direct him in his choice of a second opinion. I then simply asked him: Can I make a recommendation? I won-dered whether this recommendation would have any more effect on this patient than any other recommendation I had made in the past. I suggested he see the only ophthalmologist that is a fellowship-trained glaucoma specialist in the area, instead of a general ophthalmologist. He agreed to do so.
Whats my responsibility for this patient? Was he even my patient anymore? I dont know; time will tell. There certainly is a much higher likelihood that he will return to my practice after prodding by the fellowship trained glaucoma-tologist, with whom I have a great relationship.
I called the glaucoma specialist prior to the patients visit with her to let her know what she would be dealing with, and I explained the history with this patient. I hope the patient will follow her recommendations for his sake. But the reality is that patients have to assume a certain amount of responsibility for their own care. And with this patient, you cannot tell.
If you find yourself in a similar situation, I suggest you avoid the desire to dismiss the patient (even when it seems as though you and your practice may be better off without some patients). Take care of your patients, even those who wont take care of themselves. By keeping the patients well-being first, you will sleep better at night, and do better for your patient. Maybe.
Vol. No: 142:1Issue:
1/15/05

