In March 2004, a 60-year-old black male was referred to the office for glaucoma evaluation. His primary care O.D. noted significant cupping with IOPs of 18mm Hg O.D. and 19mm Hg O.S.

He denied a family history of glaucoma, but he did admit that at an exam about three years earlier, the pressure in his eyes was high. On his history form, he did not disclose any medications he was taking. On questioning, he acknowledged that he was on two blood pressure medications, a fluid pill, and a cholesterol medication. He reported that his overall health was good except for the hypertension and hypercholesterolemia.
Diagnostic Data
On initial examination in our office, entering acuities were 20/40 O.D. and 20/30 O.S. Pupils were equal, round, and reactive to light and accommodation with no afferent pupillary defect. Confrontation fields were normal O.U. A slit lamp exam was remarkable only for corneal arcus O.U.
Applanation tensions were 14mm Hg O.D. and O.S. Central corneal thicknesses were 531m O.D. and 535m O.S. Gonioscopic examination demonstrated grade III-IV angles O.U. with a moderate amount of trabecular pigmentation; there were no angle anomalies.
Threshold fields demonstrated a superior arcuate scotoma O.D. involving fixation; the left field was unremarkable. Reliability indices were high.
Through dilated pupils, his crystalline lenses were characterized by early, minimal lenticular changes. Both maculae showed dry retinal pigment epithelial (RPE) mottling; there was no clinical evidence of subretinal neovascular membrane formation or leakage. His peripheral retinas appeared normal O.U.
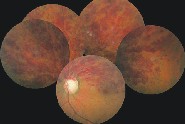
The left eye shows hemispheric vein occlusion with extension of the hemorrhage into the foveal avascular zone.
Stereoscopic exam revealed cup-to-disc ratios of 0.90 x 0.90 O.D. and 0.85 x 0.85 O.S. The neuroretinal rims were thin, with excavation beneath the lips. A significant amount of laminar remodeling was present in both nerves. The discs and cups appeared to be naturally large in size, but clearly showed advanced glaucomatous damage.
The perioptic vasculature was characterized by mild arteriolar attenuation O.U., and the posterior pole vasculature was characterized by grade II hypertensive retinopathy and grade II atherosclerotic (AS) retinopathy.
Management
I diagnosed the patient with advanced normotensive glaucoma, with preperimetric findings O.S. I prescribed Travatan (travoprost, Alcon), 1 drop O.U. h.s., and asked him to return in three weeks.
At that visit, IOPs were 10mm Hg O.D. and 9mm Hg O.S., and he tolerated the medication well. Repeat field studies demonstrated the same findings as the primary fields. I asked him to continue the medication and return in four months.
But before his next scheduled follow-up visit, he presented with a somewhat urgent complaint of decreased vision in his left eye. He said that his vision in that eye had been blurry for about one week, and that he had discontinued the Travatan in both eyes because of it. Visual acuities in the left eye at this visit were reduced to 20/80.
Dilated examination showed a hemispheric vein occlusion O.S. with extension of hemorrhage into the foveal avascular zone (FAZ), with significant macular edema.
I had a lengthy discussion with the patient about the systemic risk factors for the development of hemiretinal vein occlusions. I told him that we may need to consider anticoagulant therapy to help perfusion of the retina. In preparing the order form for blood workincluding a lipid profile, CRP, ESR, and homocysteinethe patient admitted that he was actually on more medications than he initially disclosed, and that one of them was Plavix (clopidogrel, Bristol-Myers Squibb). He explained that he had previously been found to have 50% stenosis of the right internal carotid and 100% stenosis of the left, and was subsequently medicated with the Plavix.
Needless to say, we had a chat about full disclosure of his entire systemic history, and the importance of the systemic diseases and how they relate to the eye. The patient subsequently faxed to us a list of his medications which included: Lotrel (amlodipine/benazepril, Novartis); hydrochlorothiazide (HCTZ); labetalol; K+ supplementation; 325mg enteric-coated aspirin q.d.; 75mg Plavix q.d.; Lipitor (atorvastatin, Pfizer); Neurontin (gabapentin, Parke-Davis); and Protonix (pantoprazole, Wyeth).
Discussion
Many patients fail to see the need to disclose medications and a thorough systemic history to their eye-care provider. In hindsight, this patients significant cardiovascular diseases were the basis of his advanced glaucomatous optic neuropathy with relatively low pretreatment IOPs.
As eye-care providers who manage glaucoma, we continually look for the many risk factors of the disease as we work-up our patients. But remember that glaucoma itself is a risk factor for other eye diseases, such as vein occlusions. The risk factors and associated systemic conditions that predispose a patient to retinal vein occlusions include hypertension, hypercholesterolemia, atherosclerotic cardiovascular disease, age (sixth and seventh decade), IOP that exceeds retinal vein perfusion pressure (pressure dependant or normotensive glaucoma), hyperviscosity syndromes, and periphlebitis.1
The role of elevated C-reactive protein levels and elevated homocysteine levels as markers for global cardiovascular risk and hypercoaguability are becoming more evident in management of patients with retinal vascular disease.
While a thorough systemic work up is essential in identifying the etiology of retinal vein occlusions, bear in mind that glaucoma is an isolated risk factor. Ultimately, this patients cardiovascular status is behind both the development of the normal tension glaucoma, as well as setting the stage for IOP to exceed retinal venous pressure. Accordingly, management of the vein occlusion includes adequate hypertensive control, tight glycemic control (his HgbA1c level was elevated in the initial work-up), and lipid control, which are being evaluated by his primary-care physician.
But an equally important component in the management of the vein occlusion is management of his IOP. Although the patient initially attributed the decreased vision to the Travatan and discontinued its use, the Travatan was re-started to manage both the normal tension glaucoma and the hemiretinal vein occlusion.
At this time, the vein occlusion has remained non-ischemic, and the clinical picture is improving. Meanwhile, I will stay the course in his glaucoma management.
1. Kanski JJ. Clinical OphthalmologyA Systematic Approach, 5th ed. Oxford: Butterworth-Heinemann, 2003.

