 |
A 57-year-old Caucasian male presented with a complaint of gradually decreasing vision in his left eye for the past eight to nine months. He denied any ocular pain, headaches, tinnitus or transient visual obscuration associated with his vision loss. His ocular history is positive for a cataract surgery performed three years earlier in both eyes. His medical history is positive for hypertension, diabetes and sleep apnea, which are medically controlled with lisinopril, metformin and a continuous positive airway pressure machine, respectively. He denied smoking, alcohol or illicit drug use.
On examination, his best-corrected visual acuities were 20/20 OD and counting fingers at three feet in his left eye with a prescription of -1.25 +0.75 x 035 OD, -2.50 +1.00 x 005 OS. Confrontation visual fields were full for the right eye, but revealed a generalized constriction for the left eye. Threshold visual field testing was performed and showed an enlarged blind spot in the right eye and severe depression in the left eye. Extraocular motility was full for both eyes and pupils were equal, round and minimally reactive to light with a trace afferent pupillary defect in the left eye. Color vision, measured with Ishihara plates, was full for the right eye and completely diminished for the left eye (10/10 OD, 0/10 OS).
Intraocular pressures were measured at 15mm Hg and 17mm Hg for the right and left eye, respectively. Anterior segment health was unremarkable for both eyes. The dilated fundus exam for both eyes shows a clear vitreous. Images of the optic nerve of each eye are available for review (Figure 1). The macula and periphery were unremarkable. Magnetic resonance imaging (MRI) was performed and is available for review (Figure 2).
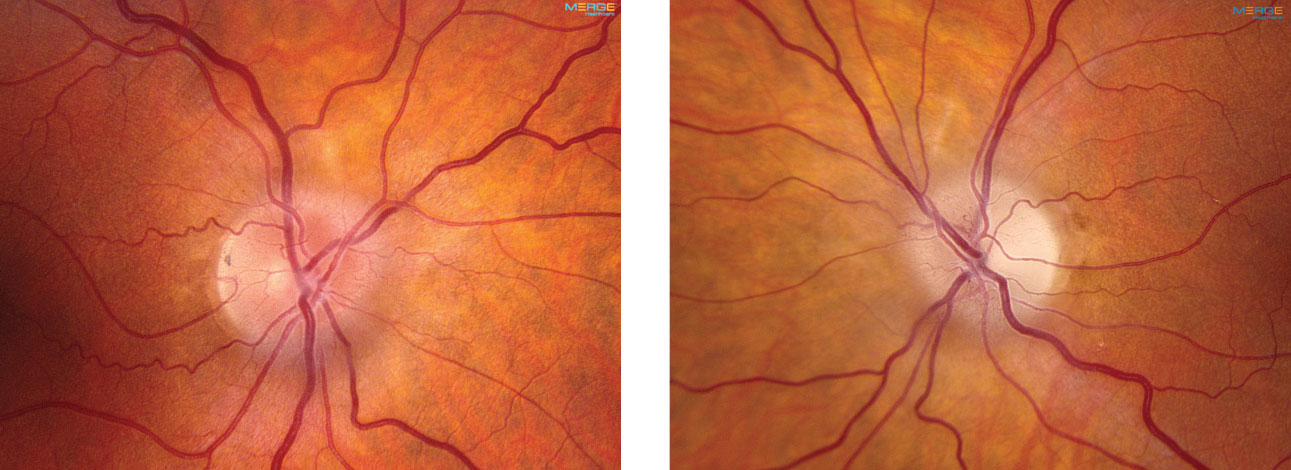 |
| Fig. 1. These are the fundus images of the right and left eyes of our patient. What can they tell you about the cause of the patient’s symptoms? |
Take the Retina Quiz
1. How would you describe the optic nerve appearance in our patient?
a. Normal, distinct margins OU.
b. Optic disc pallor in the left eye.
c. Optic disc edema in the right eye and optic disc pallor in the left.
d. Grade 1 disc edema in both eyes with temporal pallor in the left.
2. What does the MRI reveal?
a. A mass in the frontal lobe.
b. A mass in the parietal lobe.
c. An infarct in the occipital lobe.
d. A chiasmal lesion.
3. Based on the testing and images, which is the correct diagnosis?
a. Guillain-Barré syndrome.
b. Anterior ischemic optic neuropathy.
c. Foster Kennedy syndrome.
d. Pseudo-Foster Kennedy syndrome.
4. How should this patient be managed?
a. Observation.
b. IV steroids.
c. Neurosurgical consult.
d. Optic nerve sheath decompression.
Diagnosis
Our patient has subtle grade 1 disc edema in both eyes. What’s more, the left eye also has as obvious temporal pallor. This is evident when you compare the coloration of the neuroretinal rim in each eye.
This presentation alone should raise a red flag for possible Foster Kennedy syndrome, which presents as disc edema in one eye and optic nerve pallor in the other.
Foster Kennedy syndrome is characterized by a sub-frontal meningioma, resulting in compressive optic neuropathy and increased intracranial pressure (ICP).1 This, in turn, causes optic nerve atrophy and pallor ipsilateral to the tumor and optic disc edema contralateral to the tumor as a result of increased ICP.2
Researchers believe Foster Kennedy syndrome represents 1% to 2.5% of all intracranial masses.4 The conditions three clinical presentations include:
- Type 1: Optic atrophy on one side with contralateral disc edema.
- Type 2: Papilledema with unilateral optic atrophy.
- Type 3: Papilledema with bilateral optic atrophy.
Each presentation is dependent upon the location of the tumor and when symptoms are detected. Symptoms include progressive vision loss, ipsilateral anosmia (loss of smell), diplopia, headaches, nausea and vomiting.1 While its primary location is in the sub-frontal region, it can also present in the olfactory groove, falx cerebri and sphenoid wing, all of which result in a different constellation of signs and symptoms.4 An optimal way of diagnosing this condition is through funduscopic examination coupled with MRI.
One key differential is pseudo-Foster Kennedy syndrome, which is defined as optic nerve pallor in one eye and disc edema in the contralateral eye in the absence of an intracranial mass.5 The two most common causes of this condition include, but are not limited to, a bilateral sequential ischemic optic neuropathy or optic neuritis.3 Other, less common causes include a prior papillitis or a secondary optic atrophy from trauma, infectious, inflammatory or infiltrative origins.3 Interestingly, pseudo-Foster Kennedy syndrome is another clinical possibility to consider in our patient. This rare occurrence is defined as the presence of both an intracranial mass and an ischemic event that results in the same clinical picture as Foster Kennedy syndrome.3 Apart from visual field testing and OCT a brain and orbital MRI must be performed to correctly differentiate between these syndromes and make an accurate diagnosis.
The MRI of the brain in our patient revealed a large left-sided meningioma of the anterior cranial fossa measuring 7x7x6mm with diffuse enhancement. There is an extension of this mass to the left optic canal as well as to the superior portions of the left cavernous sinus with no effect on the left extraocular muscles of the orbit. In contrast, the right optic nerve and the right optic canal appears to be intact with no mass effect. These findings confirmed our suspicion of Foster Kennedy syndrome.
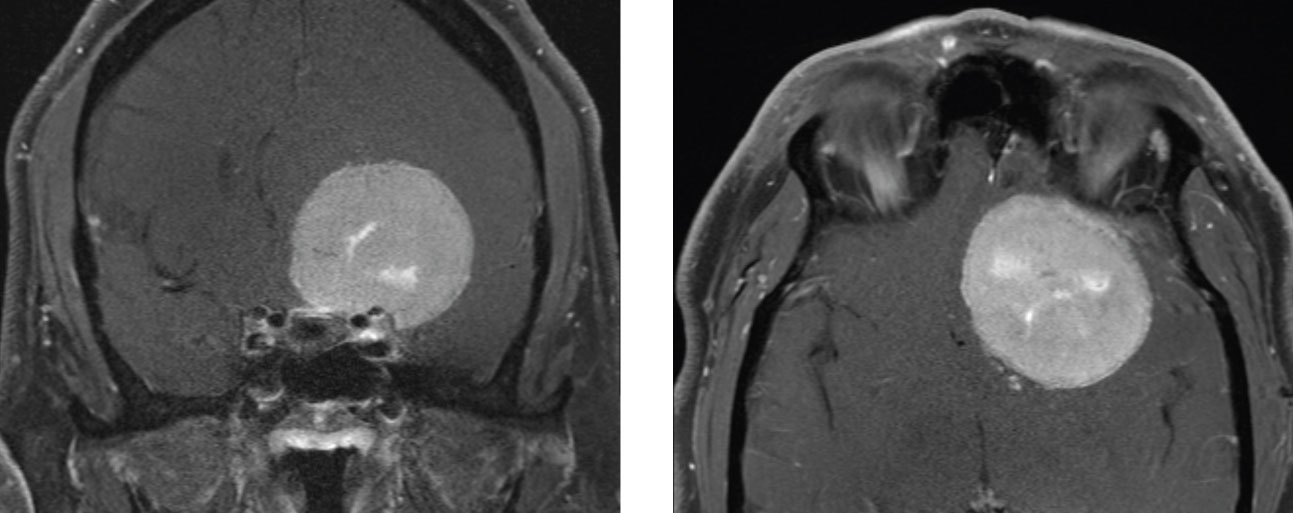 |
| Fig. 2. At left, the coronal view of the MRI. At right, the axial view of the MRI. |
Management
Treatment for patients with Foster Kennedy syndrome can be divided into medical and surgical management. Initial medical management for symptomatic brain tumors includes oral corticosteroids, which may help to reduce edema surrounding the tumor as well as decrease ICP.5 Radiotherapy or radiosurgery is also a non-surgical way to shrink the tumor and prevent further growth and expansion.1,5
The most effective and primary course of treatment is surgical resection to reduce the mass effect and relieve the elevated ICP.5 In cases where tumors are not resectable or do not benefit from radiotherapy, hydroxyurea chemotherapy may be modestly beneficial.5 However, further studies are required to establish its clinical significance.5
The prognosis for these types of cases is variable, depending on factors such as the chronicity of the condition, the size of the tumor and the age of the patient. Nevertheless, early recognition of the signs and symptoms along with an accurate diagnosis of Foster Kennedy syndrome is critical to a patient’s quality of life and final visual prognosis.
Our patient was immediately referred to a neurosurgeon and he had emergent surgery. He continues to be followed closely.
Dr. Jayasimha is an optometric resident at Bascom Palmer Eye Institute in Miami.
Retina Quiz Answers:
1) d; 2) a; 3) c; 4) c.
1. Lai A, Chiu S, Lin I, Sanders M. Foster Kennedy syndrome. J Neuro-Ophthalmol. 2014;34(1):92-4. 2. Sadun A. Foster-Kennedy syndrome. Science Direct. www.sciencedirect.com/topics/medicine-and-dentistry/foster-kennedy-syndrome. July 03, 2008. Accessed January 16, 2019. 3. Vickers L, Bhatti T, El-Dairi M. Diagnose and manage pseudo–Foster Kennedy syndrome. www.aao.org/eyenet/article/diagnose-manage-pseudofoster-kennedy-syndrome-2. January 2014. Accessed January 16, 2019. 4. Walia H, Grumbine F, Sawhney G, et al. An aggressive sphenoid wing meningioma causing Foster Kennedy syndrome. Hindawi. www.hindawi.com/journals/criopm/2012/102365. May 17, 2012. Accessed January 16, 2019. 5. Zhou Y, Vickers A, Ponce C, et al. Foster Kennedy vs pseudo-Foster Kennedy. eyewiki.aao.org/Foster-Kennedy_vs_Pseudo-Foster-Kennedy. January 14, 2018. Accessed January 16, 2019. |

