For those of us who specialize in contact lenses, our primary goal is improving our techniques to increase both patient satisfaction and our own success rate. But defining success in terms of a lens fit—especially considering that both you and the patient contribute different factors—can be challenging. How successful are we as practitioners when fitting our patients with soft multifocal contact lenses, and do we really give them what they are expecting?
 |
While a student at the Southern California College of Optometry, a mentor of mine, Harue Marsden, OD, taught me the importance of patient education and, more importantly, the value of patient understanding. This article discusses options for improving patient comprehension of how multifocal lenses work, which may ease the fitting and wearing experience as well as prevent patients from dropping out of contact lens wear entirely. As always, the primary goal is to reduce frustration, increase satisfaction and elevate the practice’s multifocal contact lens success rate.
Take a Step Back
At the heart of the matter is presbyopia. More patients than ever are dealing with loss of accommodation: approximately one-third of current patients are presbyopic, with 2.3 billion presbyopes worldwide expected to surface by the year 2020—135 million of whom will be in the United States.1,2
As such, many of us likely mention age in some way in our discussion of presbyopia with our patients. However, we should consider a different culprit. Although standard practice is to refract the patient to 20 feet away, this generation of presbyopes spends a large amount of time in front of monitors, laptops, tablets, e-readers and cell phones, which are less than two feet in front of them. A 2015 report by the Vision Council on digital eyestrain noted that more than 90% of American adults use digital devices for at least two hours per day, with close to 30% of individuals using digital devices for more than nine hours each day.3 Our visual world is much closer to us than in the past.
Fitting Step-by-StepThis step-by-step guide is designed to work with all lens designs: 1. Obtain an accurate refraction value. This is the foundation upon which much of the contact lens fitting process is based. Don’t over-minus and don’t over-plus the reading, as this can lead to inaccurate focusing later. Additionally, try to minimize the difference between distance and near viewing to reduce the add demand required, which will reduce the amount of adaptation required and likely increase your success rate. A patient with less than 1D of cylinder may be easier to fit than those with higher cylinder prescriptions. 2. Determine the patient’s dominant eye. This is necessary for choosing lenses and will help during troubleshooting. Sensory dominance testing in which you evaluate the binocular response to plus over each eye, in my opinion, is a better indicator of how the patient will likely respond to simultaneous vision compared with the sight dominance testing process that incorporates hand motions to form a triangle to evaluate for alignment. 3. Check the patient for any ocular surface issues such as dry eye prior to fitting them with contact lenses. Though comfort is less of an issue today due to new developments in technology, this will ensure other factors are not hindering contact lens success. 4. Select the lens modality you think will work best for the patient, regardless of price. Then, incorporate the vertexed spherical equivalent of the spectacle refraction, together with the corresponding lens manufacturer’s fitting guide, to choose the initial contact lenses for the patient. 5. Apply the lenses to the patient’s ocular surface and let them settle. Direct the patient to look at frames, read a magazine or survey the office. The more time patients have to do this, the better the contact lenses will settle and improve accuracy in your vision assessment. 6. Evaluate the fit once you feel enough time has passed. Look for indications that the lenses are centered, aligning the optics of the lens with the center of the pupil and line of sight. When evaluating the patient’s vision in their new lenses, keep the lights on and test binocular vision in both distance and near ranges. Additionally, use real-world test methods, such as cell phone screens, watches, magazines and pill bottles to further evaluate the lenses. Success is achieved only when all initial complaints have been satisfied. In the case of a chart, set 20/40 as the goal and express excitement if the patient is able to pass this line. A chart on the wall with no instructions to the patient has an automatic implied expectation that the bottom line is success. 7. Troubleshoot. If there are any problems, perform a binocular distance over-refraction, regardless of the complaint. Use loose lenses to push plus power in the distance, but do not change the add power. Changing the add power is a large shift in the design of the lens and should only be considered once small distance changes to the spherical component have been made. However, if changing the spherical component does not ultimately solve the patient’s problems, refer to the fitting guide for directions on making proper adjustments to the add power based on the patient’s complaints. If there are still issues remaining at this point, consider the possibility of an incorrect refraction, the need for a different lens or the lens is fit optically off-center. Evaluating monocular vision at this point may help in troubleshooting refractive errors. |
The human visual accommodative and convergence systems are relied on more than they ever have been before; thus, the rate of population entry into the presbyopic category, a condition in which the ability to focus up close declines over time, is increasing significantly. Anecdotally, patients seem to arrive at my clinic at a much earlier age than the previous decade, asking about asking about near assistance and support. The industry as a whole is catering to these pre-presbyopic patients with exercises, visual breaks and ophthalmic tools that push plus power up close. With all this in mind, we should consider digital devices to be a primary source of early-onset presbyopia, in addition to age and chance.
Use of multifocal contact lenses in children to help slow the rate of myopia progression continues to be investigated by researchers and applied in clinical practice—yet another opportunity to help patients in need.
The Right Approach to Education
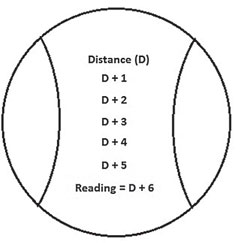
Generally, presbyopia occurs between the ages of 30 and 65 with the loss of the ability to accommodate by 2.5D, or a change of 10 units over the course of 35 years if broken into 0.25D steps. Using this unit system can be beneficial when explaining the process of loss of the focusing system to patients and can help you pinpoint where they are in the process—specifically, how much more change they have ahead of them. Doing so may eliminate concerns regarding the frequent lens prescription changes they may require.
For the most part, presbyopic patients are in denial and do not want to be informed that age is the reason for their visual changes. We can overcome this resistance by highlighting computer focusing trends, explaining the system of 10 units of change and initiating the conversation sooner with each patient. With this approach, many will be less frustrated or upset. For example, if a patient presents to the clinic with a +1.50D add, they have more than likely lost six units of their accommodate muscle energy and are running with only 40% of their initial ability. This patient would require six units of add/magnification support to return them to their full potential. This explanation helps patients understand where they are in the process and how much muscle they have lost, enabling them to track their own personal rate of change.
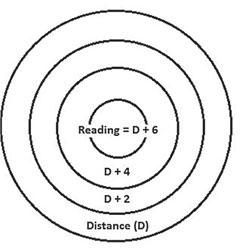
The system of 10 units can also be used to clarify how a pair of progressive lenses is a linear system while a soft multifocal contact lens is typically designed in a circular pattern. Explaining the differences in glasses and contact lens designs is key to clarifying how these products work and understanding which one is right for the patient.
Most importantly, beginning patient education early is key to achieving greater fitting success using either progressive ophthalmic lenses or soft multifocal contact lenses. Patients with a lower add amount typically have an easier time adapting to soft multifocal lenses as compared with more mature presbyopic patients.
Soft Multifocal Lens Designs
Broadly speaking, there are two multifocal lens designs: translating and simultaneous vision. Translating designs, which resemble traditional bifocal and trifocal ophthalmic lenses, are for the most part only found in gas permeable contact lenses. These provide crisp vision and are suitable for higher add demands. They are, however, more complex to fit and require greater patient adaptation as they must train themselves to use downgaze for the add power.
Simultaneous vision is the process through which multiple powers are presented to the eye at the same time. The patient’s visual system then chooses which prescription to focus through in order to see the image in question at the selected distance, while ignoring the other prescriptions. There are two forms of simultaneous vision—concentric and aspheric—although many lenses involve a combination of concentric and aspheric designs.
Explaining to patients the complexity of the visual system and how simultaneous vision lenses work can help them better understand the design and also the reasons why 100% crispness of vision is not always feasible, particularly in low-light conditions. It can also help patients understand why a certain lens may not be the right fit for them. Two patients with the same prescription and the same daily visual tasks might wear different multifocal lenses because they process certain lens designs in different ways. Ensuring thorough patient education also helps to alleviate any blame the patient may place on you or the lens design for perceived inadequacies.
Introducing Soft Multifocal Lenses to The Patient
There are several steps to consider when introducing patients to soft multifocal contact lenses. First and foremost, you can gauge patients’ awareness and level of interest with either paper or electronic signage in your reception room and dispensary, as well as questions on your intake form. For a more active approach, direct staff members to inform patients about the lenses during the registration process, pre-testing session or at checkout following the appointment. The most important discussion, however, comes directly from the practitioner via a recommendation, which can be as simple as a new product update or a more targeted presentation of the available options.
Regardless, when introducing the concept of multifocal contact lenses, it is key to first explain presbyopia and its effect on visual demands. From there, relay the available advancements in technology and multifocal options and, if they express interest, continue by describing the pros and cons of the lenses and their designs, the fitting process, follow-up timeline, issues or complications they may experience during adaptation to the lens and, lastly, the cost. Providing the patient with an understanding of the entire process helps the patient accept the fitting fee.
Fitting time. At my practice, we find that it can take about 2.5 visits on average to fit a soft multifocal lens properly; the exact timeframe will depend on the amount of add power needed and the patient’s adaptability. To avoid patient frustration, always make them aware of this fact so they can plan accordingly. Communicating clearly about the protracted nature of the fitting process also helps to justify the fitting fee in their minds.
During each visit, patients should expect to devote ample in-office time to trial lens wear so that perceptual adaptation can take place before assessing visual performance. Although there is no set length of time for this, we find 20 to 30 minutes may be adequate, during which patients can test their lenses using various viewing materials around the office. If patients object to the fitting delay, inform them that this time allows their visual system to adapt to the lens, after which their concerns are more easily addressed. A small change in power can alter the distribution of the pattern on the lens surface, changing how their eyes react to the design. Thus, it is important to give them time to adapt in the office so they do not walk away with improperly powered lenses.
Patient adaptation to multifocality continues following exposure to real-life visual demands beyond the office setting, and patients need to be prepped to anticipate this and advised to withhold judgment for several days after the initial fitting. We schedule a one-week follow-up appointment to reassess the fit and visual performance of the lens after patients have had time to neuroadapt.
Fitting limitations. When discussing limitations with the patient, mention the design of simultaneous vision lenses and the importance of adequate light. The human pupil is a dynamic system, while soft multifocal lenses are not; a simple explanation regarding how dilation works can prevent many patients from expressing frustration— when attempting to read a small menu in a poorly lit restaurant, for example. Under-promising and over-delivering is the best strategy, which can be done by being realistic, not necessarily negative.
 |
| Progressive lenses, above, usually have a linear design, while multifocal contact lenses use a circular design, below. |
 |
Fitting fees. When it comes to fees, you should feel confident appropriately charging for your education, years of experience, expertise and time. As experts, we deserve to be paid for both our knowledge and time. Arrange a mutually agreed-upon course of action prior to the contact lens fitting so both you and the patient understands what is expected of each other. Having a back-up plan in the event the lens fit does not work is also a good idea: this may include modified monovision, monovision or distance contact lenses with glasses placed over top for reading purposes.
Refining and Rethinking
If patients do not adapt well to multifocal wear, don’t give up just yet. The abundance of designs on the market today offers alternatives that are worth exploring with a properly motivated patient. The patient may fail in one multifocal design concept and yet do just fine with a different approach. Again, make sure the patient is prepped at the outset about this potential setback and your contingency plans.
Should the patient find the next lens also poorly suited to their needs, we consider modified monovision before abandoning multifocal wear entirely. This approach—when only one multifocal lens is used—has no exact guidelines; it is more of a trial-and-error approach to fitting lenses when the patient’s prescriptions do not follow the usual guidelines and principles. Examples include emmetropic patients who view even a plano lens as a distraction, early presbyopes who may not need two multifocal lenses initially, and astigmatic patients.
Fitting emmetropes with one multifocal lens in the non-dominant eye is an easy entry into presbyopia, but the latter two types of patients are slightly harder to manage. In the case of early presbyopes, even the presence of two low lenses may provide too much add power; instead, place a single vision lens in the dominant eye and a multifocal in the non-dominant eye. Patients who have astigmatism higher than 1D may have difficulties using spherical lenses. For these patients, place a toric lens in one eye and a multifocal lens in the other to provide distance clarity and near support. Those who have high levels of astigmatism in both eyes unable to be masked with a spherical lens should consider wearing soft toric multifocal, hybrid, gas permeable or scleral contact lenses.
If the monovision contact lens approach fails due to a lack of intermediate vision or if the range of vision between near and distance becomes too vast for adaptation, placing a multifocal in the non-dominant eye can assist with the patient’s intermediate vision. You must get creative to help these patients, and perhaps consider options such as using low add powers in the dominant eye and higher add powers in the non-dominant eye to prevent blur from two high aspheric lenses. Unfortunately, switching monovision patients to multifocal contact lenses is not an easy task, as they enjoy good distance and near clarity. The best strategy, when possible, is to avoid monovision as the initial choice entirely.
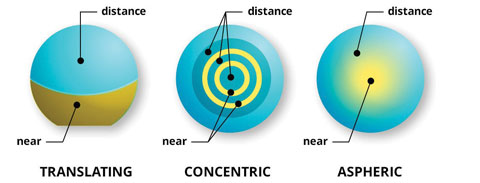 |
| Explaining how each lens works will help patients understand the difference and ensure successful contact lens wear. Image: All About Vision. |
The End of a Fit
With so many factors in play during a multifocal lens fitting, it can be challenging to know when the patient is fit in the best possible option. The end of a fitting comes when there are no other means to adjust the lenses. Patients who are content with their vision may continue to provide feedback until you ask them to stop; thus, it is acceptable to inform a patient that you have reached the best level of vision possible with the lenses they are in. Remember, you guide and control the process and can decide when to stop taking further action.
Above all, however, you can achieve higher rates of success with multifocal contact lens fittings when patients are properly educated on both the affected visual structures and the fitting process. Including them on the journey helps them remain involved with their eye care decisions, ensuring you are both on the same page with the same goals in mind. A comprehensive approach based on effective communication builds stronger relationships between you and your multifocal lens patients.
Dr. Pal runs a specialty contact lens and dry eye practice in Toronto. She is the vice chair of the AOA Contact Lens and Cornea Section Council, a member of the Women’s Advisory Board for Alcon and a speaker for Allergan’s dry eye faculty in Canada. She is consultant for Allergan, Alcon, Bausch + Lomb, CooperVision, Johnson & Johnson Vision Care and Menicon, as well as a facilitator of the STAPLE lens fitting workshops.
|
1. Silicone Hydrogels. Contact Lens Options for Presbyopia. Available at: www.siliconehydrogels.org/editorials/previous_editorial_jackie_tan.asp. Accessed July 18, 2016. 2. National Eye Institute. Myopia Defined. Available at: www.nei.nih.gov/eyedata/myopia#4. Accessed July 18, 2016. 3. The Vision Council, 20154 Digital Eye Strain Report. Available at: www.thevisioncouncil.org/blog/2014-digital-eye-strain-report. Accessed July 18, 2016. |

