Eye care professionals (ECPs) probably spend more time trying to make their progressive wearers satisfied than any other category of eyeglass wearer. But despite advances in lens design and manufacture over the last 25 years, ECPs still yearn to discover the perfect progressive—the one design that balances acuity, comfort and utility just right. And while balancing these elements is essential, frame fit, cosmetics and perceived value also remain important ingredients in a successful experience.
To help both sides of the dispensing desk arrive at the best solution, let’s start with a review of the fundamentals for dispensing progressive addition lenses (PALs). While challenging, these conditions can be comanaged successfully, and optometrists are in the perfect position to take a leadership role in the care of this sizable patient population.
The Juggling Act
 |
|
Fig. 1. Pupil size determines the effective cross section of the eye’s refractive optical train—cornea, crystalline lens and retina—that is contributing to the final refractive result. Click image to enlarge. |
One of human vision’s biggest advantages—that it’s inherently “squishy,” or adaptable—does hinder choosing the best lens for any individual PAL wearer. The eye/brain’s ability to adapt and function well in a matrix of less-than-optimal conditions, such as eyewear routinely made off-spec or with poor lens materials and centering, can hide what matters most for any individual patient. This squishiness also helps in defining the larger area of wearer satisfaction colloquially called “20/happy,” which can guide in determining the most efficient use of professional time and materials.
But even 20/happy can be elusive, and therefore ECPs should always remain open to novel information as they juggle prescription, progressive design and placement to deliver a superlative progressive experience.
Prescription
Perhaps nothing impacts a prescriber’s approach more than time spent performing eyeglass rechecks. By the time a wearer lands in the doctor’s chair for a recheck, usually the Rx is the top suspect behind their eyewear dissatisfaction. Although creating the best progressive begins with an accurate refraction, it sometimes goes awry when the well-intentioned prescriber’s discretion influences the final Rx in a way that works against progressive success. Below is a short list of suggestions that can improve progressive satisfaction:1. Don’t massage the astigmatism. Full correction of astigmatism delivers the best bang for the buck when chasing optimal acuity. But prescribing the full astigmatism can come with a price: an alteration of habitual perspective that negatively impacts comfort for some wearers. For this reason, prescribers often reduce or eliminate minor amounts of astigmatism up to 0.50D.
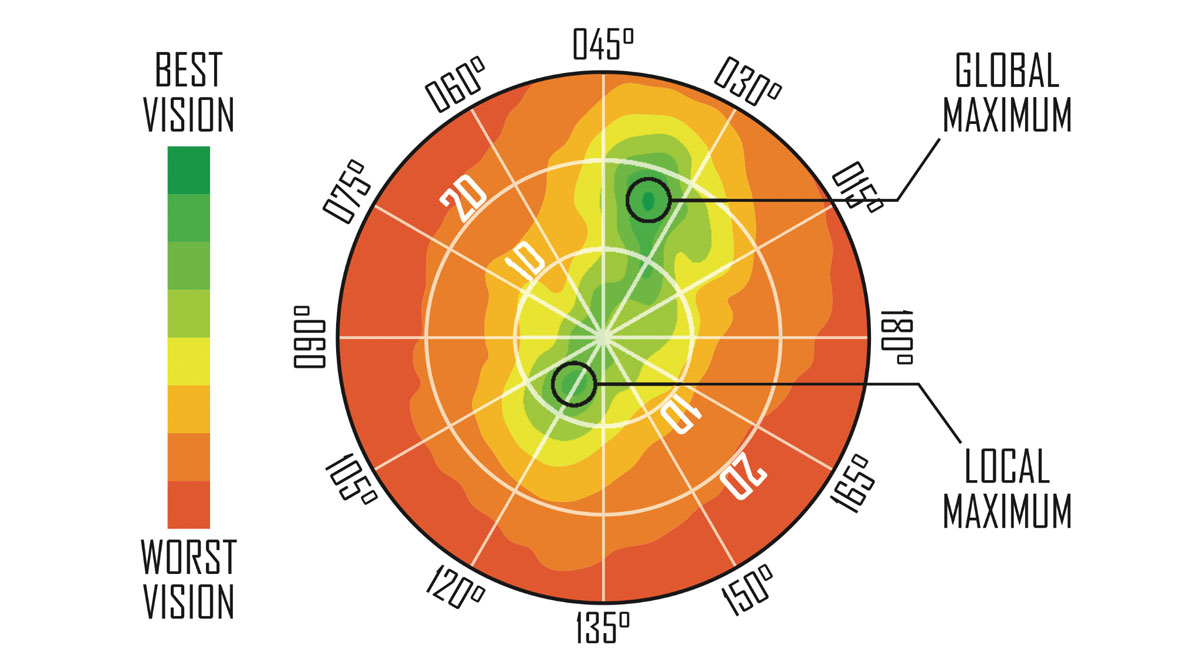
Additionally, orthogonalizing the axis—adjusting it closer to the prime meridians of 90º or 180º—is often used to further reduce perspective side effects. But all progressive lenses possess some residual astigmatism distributed across the lens surface.1 This residual astigmatism can interact with any leftover refractive astigmatic error in a progressive lens and decrease acuity and utility.
Recommendation: Prescribe the full cylinder found and avoid orthogonalizing the axis. Although satisfaction here is not guaranteed, the prospects for progressive success almost always improve when the eye’s astigmatism is properly and optimally corrected. If the wearer experiences perceptual discomfort tracked to their astigmatism correction, try switching to a softer-design progressive.
2. Consider maximum plus and acuity. Approach this timeless recommendation with caution. With the standard exam distance set at 20 feet, which equals a vergence of +0.16D, the final subjective lens choices could easily flip into an undesirable over-plus situation for driving distance. Further, anything that compromises axial acuity will further degrade peripheral acuity by compounding the inherent peripheral blur of progressive lenses.
Recommendation: Trial frame the Rx outdoors to discover the optimal flip point for achieving best acuity while driving. There are exceptions—see “Troubleshooting Mature Presbyopes” on p. 39.
3. Be aware of pupil sampling. Pupil size controls more than luminous flux and near vision depth of field: the eye’s pupil size determines the effective cross section of the eye’s refractive optical train—cornea, crystalline lens and retina—that is contributing to the final refractive result. Sphere, cylinder power and axis can vary in value between a daytime pupil of 2.5mm diameter and a nighttime pupil of 5.5mm or greater diameter.
Recommendation: Again, trial frame the Rx outside the exam room, particularly at night if possible. The best correction for night use might be different enough to recommend two different prescriptions (Figure 1).
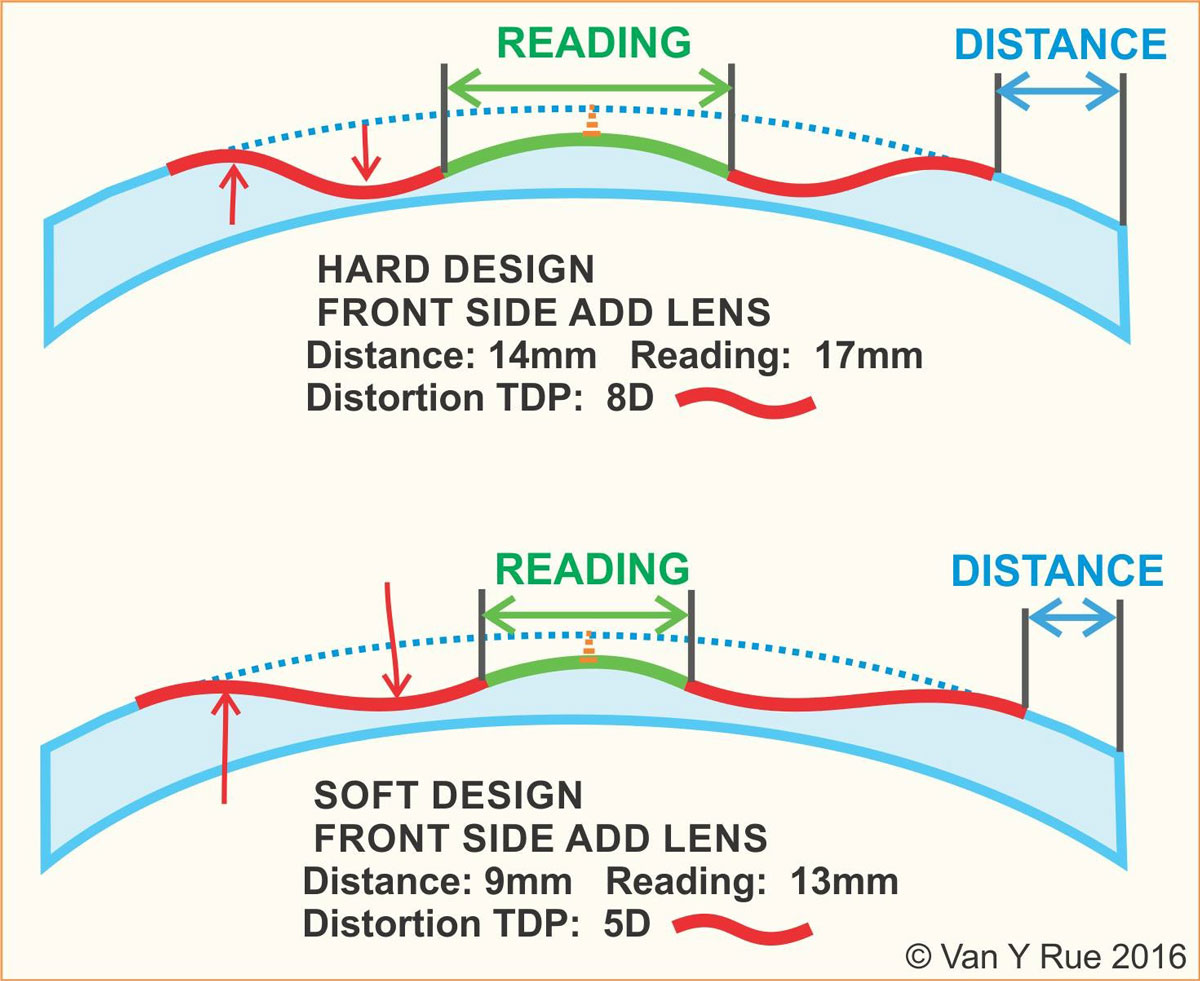
MATCHING PROGRESSIVE DESIGN TO THE WEARERYour assortment of 10 to 20 odd-sized and multi-colored contact lens trial sets says a lot more about your curated wisdom than you may realize. You carefully choose a contact lens because each fulfills a unique Rx or lifestyle need among your patient base. Every modality, base curve and diameter earns its place in your lens toolbox because it enables you to better serve patients or solve a problem. Progressive lenses are no different. Older, cast-front progressives have an inescapable physics problem because about half of the surface area was rendered useless by an inability to optimally manage the greater surface astigmatism of these designs. The areas near the intermediate corridor and peripheral distance zones have been politely termed “soft-focus areas.” To maintain a stable umbilic, traditional progressives defaulted to using a profile shaped like an hourglass. But this profile is problematic, as surface astigmatism of these older designs narrows the visual areas adjacent to the pupil while placing the widest and clearest areas at the very top and bottom of the lens.1 It’s widely agreed that free-form progressive technology has delivered wider usable zones and reduced but never fully eliminated unwanted surface astigmatism. Not well discussed is that free-form technology gives designers enormous control over where that remaining distortion is placed, and as a consequence, what zones will benefit the most. Today, free-form lens designers can literally move distortion anywhere on the lens, thereby optimizing the zones they choose. As a result, free-form progressives—just like contact lenses—have become a vastly more specialized family of lenses and far more fit-specific in their application.1 During the early 2000s, progressive lens technology exploded. The “T-shape” design—only possible in free-form—appeared first in the Rodenstock Multigressiv (Free Form Technologies), followed by the Shamir Autograph. A T-shape could offer almost edge-to-edge distance clarity at the pupil height compared to the average 5mm to 12mm of usable distance width offered by traditional molded progressive designs of the time. Astute ECPs immediately found that patient complaints about driving at night utterly plummeted. As a trade-off, T-shape designs often suffer in intermediate width. And, in many cases, the reading zones of T-shape designs were found to be narrower than popular traditional lenses of the time, such as Varlilux Comfort. Even free-form technology has limitations. At the same time, Johnson & Johnson’s Definity (now an Essilor lens) greatly improved on the original Owen Aves 1907 design, with its bi-surface design allowing advanced surface astigmatism management to push distortion away from areas nearest the pupil out to the upper and lower corners. The first advantage was increased intermediate width near the center—just below the pupil—not at the top or bottom lens edge. As a general purpose lens design, Definity became a computer user’s dream. The second advantage was that the feeling of swim and sway, especially while walking, was greatly reduced, in part because distortion was pushed more outside the foveal cone. But a disadvantage was that usable distance width was sometimes perceived to be narrower than other traditional lenses.1 Matching a lens’s inherent strengths to a patient’s unique needs, lifestyle and Rx can tremendously improve patient satisfaction and reduce non-adapts. Most free-form lenses today are distance, intermediate or reading prioritized, and knowing which designs best match a wearer’s needs is critical to improving satisfaction and creating viral patient referrals.
|
Design
Early progressives, such as the original Varilux (now Essilor) of 1959, came with substantial unwanted astigmatism in the transition zones near the progressive umbilic. As PALs evolved in the 1970s and 1980s, front-surface designs tried to reduce this in two ways: one approach—exemplified by the multi-add design of Varilux Infinity—favored adjusting corridor length to optimize the astigmatism gradient for increasing add powers, thereby optimizing corridor width and reducing swim-related effects.2
The other, exemplified by American Optical’s Omni, dispensed with retaining areas of stable power almost altogether, and spread surface astigmatism throughout the entire lens through a bipolar design.3 Nether design ultimately garnered sustained success for two reasons: Infinity required uncomfortable eye rotation in higher add powers, while unhappy Omni wearers found the bipolar design possessed insufficient areas of clear, stabilized prescription power.
But Omni did become the choice of wearers sensitive to swim effects—and provided insight on how residual astigmatism and magnification effects might be better managed. Eventually, progressive design evolved from just optimizing optics to full consideration of binocular needs. Zeiss’s horizontal symmetry—which debuted in the Gradal HS lens—was among the first progressive lenses to address the importance of binocularity.4 Gradal HS has since been discontinued.
Today, outcome-based visual satisfaction has become the target goal of PAL design. To this end, optimizing dynamic prism and dynamic magnification—the differing prismatic and magnifying effects encountered between the eyes as they gaze across the lens—becomes particularly important in any anisometropic and/or oblique cylinder axis prescription.
Optimization of these prescriptions can be achieved by using steeper or dissimilar base curves and differential lens thickness to help improve fusion and reduce swim. But the resulting cosmetics of these lenses are often less well-received by both practitioner and patient. However, wearers of lenses optimized in this way realize improved binocular function, with many reporting they are enjoying progressive comfort for the very first time. Shaw progressives are an example of this specialty approach, using an advanced, global iseikonic analysis to achieve binocular optimization.5
Today, the latest design process analyzes a wearer’s head and neck posture over time, combined with comprehensive tracking data that reveals how we actually aim our eyes and tilt our heads in everyday tasks. This data is then used to optimize corridor length, width and specific distribution of residual astigmatism in creating the best balance between acuity, comfort and utility. A sampling of today’s premium progressives that employ this comprehensive approach is found here:
- Hoya ID Mystyle 2 and ID Lifestyle 3
- Independent Owners Network (ION) Love Our Lens
- IOT Camber Steady and Camber Mobile
- Shamir Autograph Intelligence
- Varilux X and Comfort Max
- Zeiss Individual Smart Life and DriveSafe
There are further personalization frontiers to consider, such as the differences in axial length and center of rotation found between hyperopes and myopes. Finally, there’s the dark arts of trying to match the best lens for any individual wearer (see “Matching Progressive Design to the Wearer”).
|
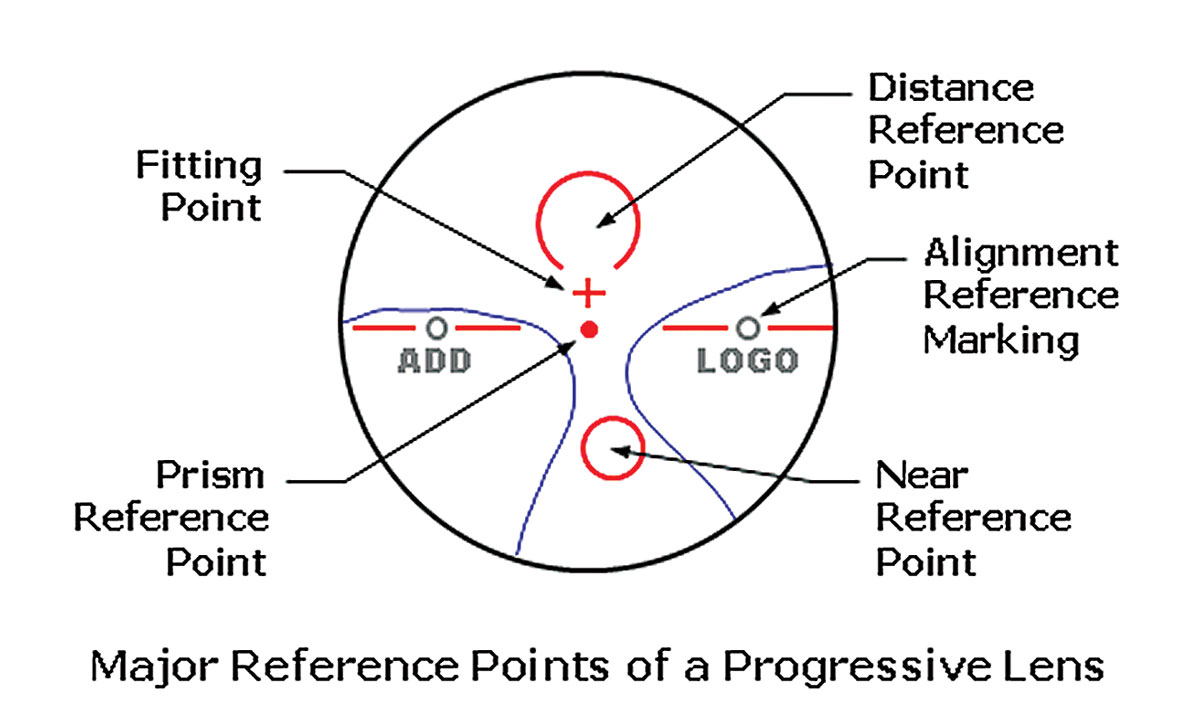
Fig. 2. The fitting cross is an important marker that designates the point of the lens that should be placed along the center of the patient’s pupil. Click image to enlarge. |
Placement
PAL designers expect their lenses will be fit according to a stated protocol, where the fitting cross of the lens is placed over the center of the pupil with the facial plane vertical—meaning perpendicular to the floor (Figure 2). This is also the proper head alignment for measuring the pantoscopic tilt of the frame chosen.
Here are three interrelated factors to always keep in mind when placing a progressive:
1. Posture. A patient’s habitual head posture often must be taken into account when specifying a fitting height. Habitual head posture reflects the routine manner in which an individual carries their head, i.e., facial plane tilted forward or back—with tilt-back posing more significance in progressive fitting. The normal approach has been to adjust the fitting height to compensate for these postural deviations.
Alternately, the corridor length may be adjusted as well—longer corridors for the head-back tilt or shorter for head-forward postures. An example of a combined approach might lower placement of the fitting cross by 1mm to 1.5mm and compensate the reading area by specifying a 1mm to 2mm shorter corridor.
2. Corridor length. Today, issues arising from cell phone usage have required revising normal eye depression angles from 26º to 28º to a less demanding 22º to 25º.1 But as the effective corridor value is often defined differently between manufacturers, comparing corridors between different PALs remains a challenge. For example, manufacturers may use either a varying metric of 85%, 95% or 100% of add power to define their corridor length.6
3. Frame fit. To further complicate achieving the best placement for a progressive, factors such as patient preference for a loose frame fit, eyelash clearance and sinus or skin sensitivity may require modifying the fitting cross placement from its position in front of the pupil.
 |
Fig. 3. Expand your knowledge and skill with progressive lenses to create a personalized experience that keeps patients coming back. Click image to enlarge. |
Troubleshoot Dissatisfaction
Despite the best laid plans of prescriber, fitter and lens designer, wearers will inevitably return dissatisfied with their progressive lenses. When rechecking the Rx, here are two exceptional situations to keep in mind:
1. Mature presbyopes. Defined as near additions of +2.00D and above, lenticular changes often precipitate changes seen in total astigmatism and sphere power. With all progressive lenses possessing some residual astigmatism, not fully correcting the eye’s astigmatism can result in patients having to hold their head “just so” to see clearly in the distance—which is colloquially called “hot-spotting.”
As stated previously, this effect arises from uncorrected refractive cylinder alternately interacting with the varying surface astigmatism of the progressive surface. Do not shy from prescribing the full change found in the cylinder and axis.
Further, reducing habituated plus power in the distance Rx can backfire in mature presbyopes—with new distance or driving improvements offset by unexpected loss of face-level computer utility.
2. Eye dominance and the binocular pupillary distance (PD). Essilor introduced the importance of using monocular PDs when fitting progressive lenses to help better align the narrow intermediate and near areas of early progressives. But maintaining an accurate binocular PD is of greater importance. Patients will naturally align their dominant eye to that lens’s progressive umbilic—thereby placing the total error in binocular PD, if any, into the companion eye.7
This means that the current ANSI fabrication tolerance of 1mm per eye could actually result in a 2mm error in corridor placement for the companion eye—something most wearers will find disturbing to their reading comfort and utility.
A proven technique to effectively evaluate optimal binocular progressive corridor overlap involves a chart and light source, wherein the patient views the chart and wears the light source during a progressive lens verification process.8
NEVER VISION NEEDS CHANGE THE GAME In today’s world, people are performing more varied and different types of near activities, many of which are centered on multitasking while using a phone or tablet. Whether it’s walking down the street, cooking a meal, or having a conversation while waiting for an important text, the arrival of the smartphone, smartwatch and a cornucopia of associated apps has changed the visual experience dramatically. And people are using their phone for more than just calling and texting. They use them to secure home loans, pay bills, watch movies and even to monitor their workouts. All of this added near activity comes with a cost to our eyes and our visual comfort. Zeiss has assembled a portfolio of progressive lens products call SmartLife for this very reason, with a goal of creating general-use progressive lenses that will—in one lens—attempt to better address all these new visual challenges.1 But remember that even today’s most robust, premium designs cannot fully solve all the unique challenges of every situation in one lens design. Throughout our day we do many tasks that require differing visual needs, which in turn requires a lens specifically made for that task. For example, 67% of middle-aged drivers complain of traveling at night, which requires a design that is very wide in the distance and intermediate to allow drivers the freedom to move their eyes. Zeiss’s DriveSafe attempts to address these needs.2 Drivers prefer to move their eyes rather than move their head—Zeiss DriveSafe starts the progressive corridor 2mm to 3mm lower than general purpose designs. The result is more freedom of eye movement in the distance and intermediate areas. Zeiss DriveSafe is optimized for a mesoscopic pupil, which results in wider areas of lateral vision from smoother surface contour and reduced astigmatism power. Newer LED headlights are a source of debilitating glare and emit an elevated amount of blue spectrum compared with halogen headlights. DriveSafe has an advanced blue light filter tailored to reduce glare specific to LED headlights. While DriveSafe is an excellent lens choice for everyone who drives at night, its lowered progressive corridor may be less ideal for office tasks like face-level computing. There are many types of task-specific lenses that you can recommend alongside an optimized, general purpose progressive, such as a computer lens. So, the best approach to choosing one, best general-use progressive might just be to prescribe two or more pairs.
|
Squishy Satisfaction
The one aspect of vision care that online vendors cannot address easily is the ability to follow-up on the complaints of an unsatisfied progressive wearer. So, never shy from welcoming anyone who requires after-sale attention—whether they’ve purchased the glasses from you or not. From the ECP’s end, the time spent learning to troubleshoot any spectacle wearer’s problems informs and readies oneself better for the next patient who may have similar problems (Figure 3).
My mantra has always been: “What do you learn from a patient who never returns?” So, while getting wearers to 20/happy is a convenient goal, true progressive experts never refrain from exploring where the limits of progressive satisfaction lie for an individual wearer. Patient satisfaction will always be a moving target and new lens designs will always be introduced, so remain a lifelong learner in order to stay at the top of your game.
Keep in mind that trying to choose an overall “one best lens” solution for many patients may not really be a solution at all, and this is where prescribing two or more pairs is really the best recipe for optimal visual comfort and utility.
Mr. Santini is a New York state licensed and ABOM-certified master optician and contact lens fitter at Long Island Opticians. Mr. Rue is an optical consultant and educator and progressive lens expert in the Seattle area. Mr. McCardle is a technical education specialist in North Carolina for Carl Zeiss Vision NA. Mr. Santini and Mr. Rue have no financial interests to disclose.
1. Alonso J, Gómez-Pedrero Jm, Quiroga J. Modern Ophthalmic Optics. Madrid, Spain: Cambridge University Press. 2019: 301-22. 2. Koeppen W. Progressive memories. www.wernerkoeppen.com. 2010. Accessed May 14, 2021. 3. Whitney, R. American Optical history. www.dickwhitney.net/AOHistoryLensDesigners.html. 2011. Accessed May 14, 2021. 4. Zeiss. How a patent filed by ZEISS set new standards for progressive lenses 30 years ago. www.zeiss.com/vision-care/us/better-vision/understanding-vision/how-a-patent-filed-by-zeiss-set-new-standards-for-progressive-lenses-30-years-ago.html. October 16, 2017. Accessed May 14, 2021. 5. Shaw Lens. What makes the Shaw lens different? shawlens.com/the_shaw_lens/the_science. Accessed May 14, 2021. 6. Santini B. Deep secrets. 20/20. www.2020mag.com/article/deep-secrets. 2014. Accessed May 14, 2021. 7. Clark TH. Improve PAL success with improved PAL fitting. 20/20. www.2020mag.com/article/improve-pal-success-with-improved-pal-fitting-4-1. 2018. Accessed May 14, 2021. 8. Clark TH. Apparatus for and methods of determining if progressive add lenses (PALs) are properly positioned in a subject’s eyeglasses. US Patent no. 9,104,046 B1. August 15, 2015. patents.google.com/patent/US9104046. Accessed May 14, 2021. |