There is no rush to immediately recommend surgery for strabismus. Collaborative efforts between the surgeon and optometrist allow for better outcomes. Developing all visual skills benefits the patient with strabismus, providing sensory fusion. The critical stage for sensory fusion is less limiting with new approaches used in vision therapy (VT). When amblyopia exists, VT should be the first-line approach in order to gain the best possible outcome for misalignment.
 |
|
Prescribe performance lenses to help with functional vision. These lenses can help with symptoms of poor eye teaming, tracking and focusing. Click image to enlarge. |
The Consequences of Strabismus
Patients living with constant strabismus face a lifetime of difficulties. They are more likely to be diagnosed with psychological disorders, often have low self-esteem, are less likely to find a partner, marry or have a family.1 They even have more difficulty being a competitive job applicant, compared with those without strabismus. Patients in their third decade of life with uncorrected strabismus are more likely to face long-term psychological disorders. One study showed that individuals with constant exotropia were three-times more likely to be diagnosed with a psychological disorder than controls. Patients with uncorrected strabismus also had higher rates of homicidal and suicidal ideation.1
Strabismus puts people at a considerable disadvantage due to the noticeable nature of having a turned eye, resulting in negative social stigma. In addition, there are many professions that depend on stereopsis.2 Achieving the best possible outcomes for these patients is critical for them to avoid negative psychological, socioeconomic and employment consequences. New evidence shines light on understanding outcomes of surgical intervention.
As optometrists, we meet patients going through life with these challenges because of their strabismus. We are obligated to at least make all possible treatments known and available to those interested in pursuing better vision.
Creating the very best possible outcome involves a collaborative effort between the optometrist and the strabismic surgeon. Good communication and respect for each other’s skills allows for comprehensive care. First, take time to visit each other’s practices. Second, educate the staff on how each profession contributes to successful outcomes. Third, schedule regular meetings between the two teams to discuss specific cases.
Understanding when to refer for surgery and combining the skills of a good optometric vision therapist will give your patient the best opportunity for cosmetically straight eyes with some level of stereopsis. To facilitate this for the strabismus patient, follow these steps:
- Measure best-corrected visual acuity (VA) of each eye.
- Evaluate binocularity to determine deviation and if any immediate spectacle compensation will improve the binocular stasis.
- Evaluate the ocular motor and accommodative systems.
- Determine if there is any appreciation of diplopia under any condition.
- Identify level of suppression and fusion.
- If there is some level of visual motor function that can be improved by VT, eight sessions should be completed. Then re-evaluate the system for possible improvements, such as less suppression, better cosmetic alignment, improved oculomotor function and better accommodative flexibility.
- If improvements are identified, continue with eight more sessions and re-evaluate.
- If there is a plateau in improvement and the deviation is still obvious, referral for surgery should be suggested.
- After surgery, re-evaluation of visual motor skills should be conducted and post-VT activities should be instituted to maintain gains made through surgery.
Procedure Risks
Short- and long-term complications from surgical intervention reinforce why collaboration is important. Post-op complications of strabismus surgery include conjunctivitis, scleritis, sub-Tenon’s abscess, orbital cellulitis, endophthalmitis, hypopyon, vitreous haze and scleral perforation.3
Intraoperative surgical site complications can include scleral perforation, lost muscle, slipped muscle and oculocardiac reflex, while post-op surgical site complications can include postoperative infection, allergic reaction, foreign body granuloma, conjunctival inclusion cyst, conjunctival scarring, fat adherence, dellen, anterior segment ischemia, eyelid retraction, ptosis and possible change in refraction.4 Post-op strabismus complications can involve diplopia, hyperphoria, anti-elevation syndrome and iatrogenic Brown syndrome.4
There are several risk factors to be aware of regarding strabismus surgery. Unsatisfactory eye alignment is more likely after surgery in patients with poor fusion potential or with more complicated types of strabismus. Patients with dense amblyopia or structural problems in one or both eyes have limited potential for binocular vision and do not employ fusional mechanisms to improve or maintain eye alignment.
Similarly, patients with neuro-developmental anomalies have been shown to have higher rates of undercorrection and overcorrection after strabismus surgery. Also, patients with more unusual and severe forms of strabismus, such as cranial nerve III palsies, are more difficult to align satisfactorily with surgery.5
 |
|
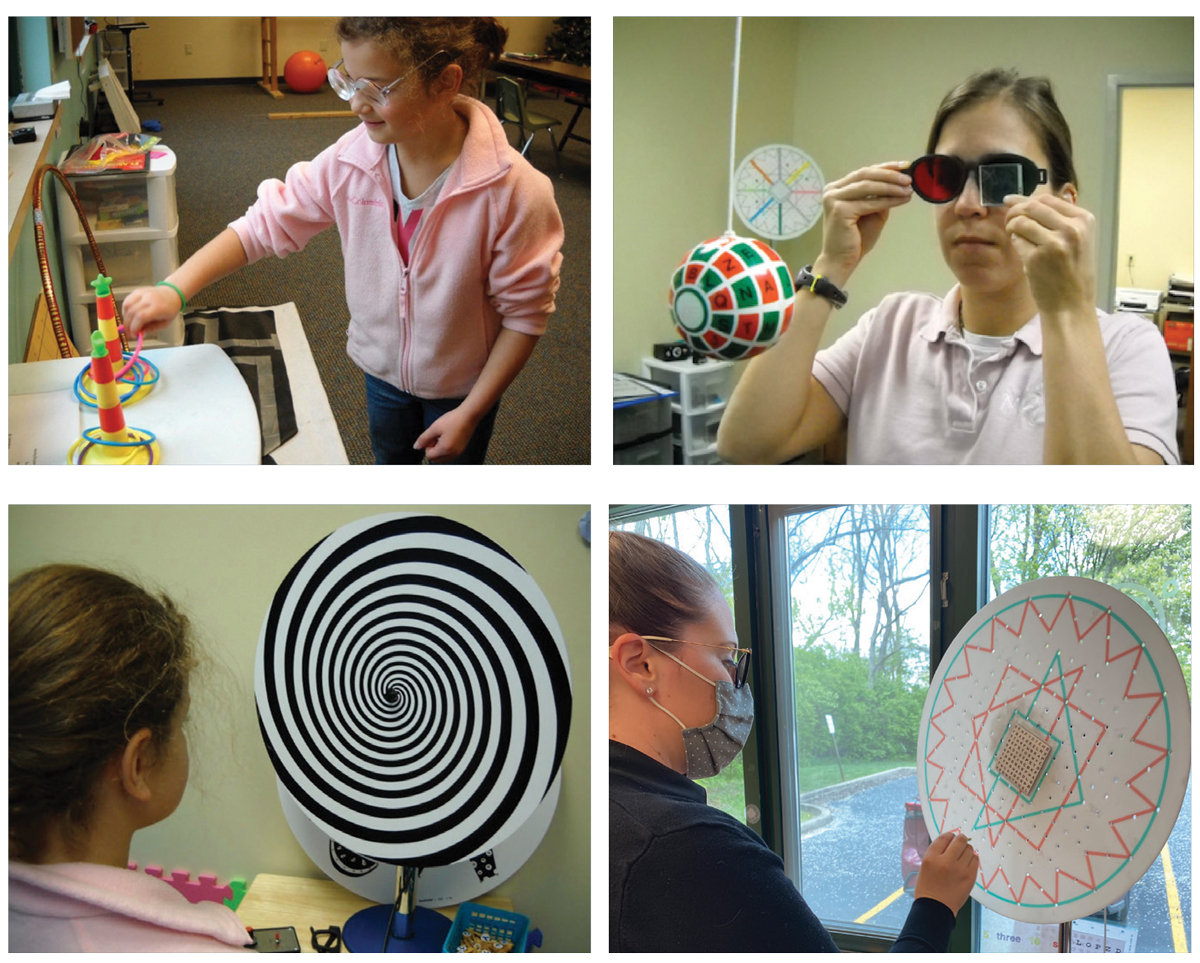
Examples of some of the many tools VT practitioners use to help improve stereopsis. Click image to enlarge. |
Surgical Timing Without Amblyopia
The outcomes of infantile strabismus surgery are based on two main factors: ocular alignment and stereopsis. Stereopsis is measured several different ways. The optimal standard is full random dot stereopsis. However, there are lesser degrees of stereo that do qualify as successful.
We are often misled into believing that strabismus surgical outcomes are high. We should note that they are considerably lower than one would hope for. Pediatric strabismus surgery has low success rates and high reoperation rates because of difficult alignment measurements and the nature of different strabismus types.
This is true when you have an inexperienced surgeon such as a first-year resident. Multiple surgeries per case are also common. The more surgeries one has, the greater chance for exotropia, vertical deviations, no stereopsis, constant diplopia or constant uncorrectable strabismus.
A successful outcome can be based on a variety of measurements. If cosmetic alignment is the criteria, the success rate is higher. Full stereopsis criteria have a much lower success rate. Socio-psychological effects are negative for those with poor eye alignment, so all efforts should be made for the optometrist and ophthalmologist to collaborate in order to achieve the best outcome possible.
The definition of success in strabismus surgery varies among different studies. Most studies set their success criteria as 8pd to 10pd deviations from orthophoria at either the three-month, six-month or last follow-up.6
Recently, an evidence-based study concluded that performing surgery later in life in patients with infantile esotropia increased the motor success rate of surgery. In addition, orthophoria is achieved with fewer surgical operations.7 Another study showed that more favorable long-term outcomes and less vertical deviations occurred when fewer surgeries were performed.8 The Cochrane study also concluded that there is no clear consensus on the optimal timing of surgery.9
Clinically, a sandwich approach—VT before and after surgery—has demonstrated that the highest outcomes are possible for these patients. This might consist of vision therapy prior to strabismus surgery to optimize sensory readiness for motor fusion and/or post-surgical therapy to stabilize or safeguard binocular vision.10
 |
|
Today, innovative technology, such as this virtual reality headset, allows us to treat amblyopia, strabismus, convergence disorders and other binocular vision problems. Click image to enlarge. |
VT Skills
Oculomotor, localization and accommodative skills build a foundation prior to sensory fusion. Management of these foundational skills prior to working on sensory fusion allows the optometrist providing pre- and post-VT to gain better outcomes. Clinically, my patients often gain cosmetic alignment simply by developing these skills, especially opposite to the direction of deviation. For example, with esotropia, working pursuits, saccades, localization and accommodative flexibility in temporal secondary gaze improves the ability to begin to appreciate fusion in primary gaze. For exotropia, these skills are emphasized in nasal secondary gaze. Poor eye movements reduce the success of gaining sensory fusion.
An overall limiting factor for patient outcomes is misaligned oculocentric localization. The patient’s awareness of where objects are judged to be located can be displaced in the direction of deviation. This needs to be addressed for both surgery and VT cases. Ocuocentric localization should match the visual axis of each eye.
After the above skills are developed, in esotropia, depending on the type, VT is used to improve sensory fusion (the patient should have good second-degree fusion prior to surgery if possible) and relative motor fusion ranges if possible. In exotropia with some sensory fusion, VT is used to improve motor fusion recoveries and ranges as much as possible prior to surgery.
Much care is needed when working with anomalous correspondence. The safest approach is to overemphasize the skills of oculomotor, localization and accommodation. Use caution when attempting to gain normal correspondence with VT prior to surgery. Attempts to break suppression should only be done for short periods (five minutes or less).
VT post-op depends on the patient’s alignment and fusional status after surgery. Generally, VT focuses on improving all visual skills including eye movements, localization, accommodation, sensory and motor fusion, again around the new angle. The ability to recover fusion is more beneficial than simply building ranges.
One study on resolution without surgery showed that esotropia with onset in early infancy frequently resolves in patients first examined at less than 20 weeks of age when the deviation is less than 40pd and is intermittent or variable. Cases with a constant deviation of greater than or equal to 40pd presenting after 10 weeks of age have a low likelihood of spontaneous resolution.10 Child development of fusion occurs at about three months; thus, misalignment is normal prior to this age.
A large percentage of patients with either esotropia or exotropia gain sensory fusion with a visual motor-based VT program. The few that do not are then referred for surgical intervention. This gives the patient the best possible outcome.
 |
|
Recent research has shown that, by developing better performance for various visual systems (e.g., eye movements, accommodation, binocularity), the amblyopic patient improves without patching. Click image to enlarge. |
Surgical Timing With Amblyopia
There is conflicting evidence whether or not to treat the strabismic amblyope before or after treating the eye deviation. One study suggested the patient obtain the best VA possible prior to surgery. Recent studies suggest that correcting eye alignment earlier will give the amblyopic eye the opportunity to develop better VA and binocular vision.11 Surgery is generally reserved for children with anisometropic amblyopia who do not respond to standard treatment, or children with serious vision impairment who are unable to wear glasses for developmental, sensory or other reasons. As a result, only a small percentage of children are suitable candidates for this surgery.12
The Cochrane study stated that the optimum timing of when to perform strabismus surgery in children with amblyopia is unknown.9 It noted that treatment for amblyopia involves methods of exercising the amblyopic eye by encouraging its increased use.
The researchers referenced several methods used to reduce the vision of the non-amblyopic eye temporarily, including penalization with cycloplegic or dilating eye drops, optical blurring of vision with high-plus lenses or physical occlusion of the normal eye. They acknowledged the newer binocular training approaches for amblyopia treatment available.9 These usually involve using a digital device that deprives the non-amblyopic eye in a bi-ocular viewing task.
To date, very few studies been conducted that represent VT. Treatment often involves a multitude of activities other than simply sitting and playing video games. These would include bi-ocular pursuits, saccades, accommodative tasks, visual spatial activities, anti-suppression decision-making procedures and visually guided movement activities. It is likely that when assessing all VT tools, successful outcomes would be much higher than those in controlled studies.
Binocular training should aim to treat amblyopia by restoring the underlying issue of reduced or absent binocularity.13
New Approaches to Amblyopia Treatment
Based on new research, the very best intervention for patients with amblyopia is to first develop a visual system in the amblyopic eye that can fixate, pursue and saccade with equal accuracy as compared with the nonamblyopic eye. The second step is to create binocularity for long term maintenance of acuity gains. Recent research has shown that by developing better visual systems, such as eye movements, accommodation and binocularity, the amblyopic eye improves without patching.13-15 This new concept has positive implications for patients, especially children who would prefer not to look different from their peers. This is a more positive psychological approach for these patients. Also, the lasting effect of VA gains is much greater using these methods than by full-time patching.
Classic teaching dictates that amblyopia must be corrected to the maximum extent possible before realignment surgery is undertaken.11
Based on my clinical experience, VT is extremely effective for amblyopia when it involves changing how the brain processes information for the amblyopic eye. This style of vision therapy uses a wide variety of eye movements and accommodative flexibility activities prior to attempting anti-suppression and fusion activities. The amblyopic eye also has opportunities to participate in a variety of perceptual activities. Typically, you will begin to see improved VA within about six to eight weeks.
After the eye movements and accommodative abilities are as equal as possible between the two eyes, incorporate the anti-suppression, fusion and convergence and divergence activities. A patient with amblyopia who develops good binocularity more readily maintains gains made in VA improvement. This is accomplished without having to continue with blur patch or deprivation activities.
Bottom line: there is no rush to jump into the deep end and recommend surgery as a first-line treatment for strabismus, and more specifically for exotropia. Wait until you have exhausted all the tools and techniques we have at our disposal.
Dr. Montecalvo practices at Nova Vision Care in Beavercreek, OH. She is a Fellow of the College of Optometrists in Vision Development, the American Academy of Optometry and the College of Syntonic Optometry. She is vice president of the College of Syntonic Optometry, a member of the AOA InfantSee Committee, board member of the Vision Leads Foundation, dean of the Vision Aces Academy and CEO of the Cedarville Vision Therapy Seminars. She is on the Neurolens Advisory Board and a compensated speaker for the company.
1. Mohney BG, McKenzie JA, Capo JA, et al. mental illness in young adults who had strabismus as children. Pediatrics. 2008;122(5):103-8. 2. Al-Saud LM, Mushtaq F, Mirghani I, et al. Drilling into the functional significance of stereopsis: the impact of stereoscopic information on surgical performance. Ophthalmic Physiol Opt. 2017; 37(4): 498-506. 3. Ing M. 7 Complications of Strabismus Surgery. Ento Key. entokey.com/7-complications-of-strabismus-surgery. February 21, 2021. Accessed March 22, 2022. 4. Clark RA, Lee AR. Strabismus surgery complications. EyeWiki. eyewiki.aao.org/strabismus_surgery_complications. Updated March 10. 2022. Accessed March 24, 2022. 5. Coats DK, Olitsky SE, eds., Unexpected postoperative alignment, in: Strabismus Surgery and Its Complications. Berlin, Heidelberg: Springer; 2007; 291–294. 6. Fu JJ, Hsieh MW, Lee LC, et al. A novel method ensuring an immediate target angle after horizontal strabismus surgery in children. Front Med. February 24, 2022. [Epub ahead of print]. 7. Muz OE, Sanac AS. Effects of surgical timing on surgical success and long-term motor and sensory outcomes of infantile esotropia. J Pediatr Ophthalmol Strabismus. 2020;57(5):319-25. 8. Lee D, Kim WJ, Kim MM., Surgical outcomes and occurrence of associated vertical strabismus during a 10-year follow-up in patients with infantile esotropia. Indian J Ophthlamol. 2021;69(1):130-4. 9. Korah S, Philip SS, Jasper S, et al. Strabismus surgery before vs. after completion of amblyopia therapy in children. Cochrane Database Syst Rev. 2014;10(10):CD009272. 10. Press LJ. The sandwich approach to vision therapy and strabismus. The Visionhelp Blog. visionhelp.wordpress.com/2019/11/14/the-sandwich-approach-to-vision-therapy-and-strabismus. November 14, 2019. Accessed February 15, 2022. 11. Von Noorden GK. Esodeviations. Binocular vision and ocular motility: theory and management of strabismus. 5th Edition. St. Louis: Mosby, 2002. 12. Bedinghaus T. Amblyopia surgery: everything you need to know. VeryWellHealth. www.verywellhealth.com/amblyopia-lazy-eye-overview-4175206. Updated October 15, 2020. Accessed March 22, 2022. 13. Hess RF, Mansouri B, Thompson B. Restoration of binocular vision in amblyopia. Strabismus. 2011;19(3):110-8. 14. Hess RF, Thompson B. New insights into amblyopia: binocular therapy and noninvasive brain stimulation. J AAPOS. 2013;17(1):89‐93. 15. Li SL, Jost RM, Morale SE, et al. Binocular iPad treatment of amblyopia for lasting improvement of visual acuity. JAMA Ophthalmol. 2015;133(4):479-80. |

