 |
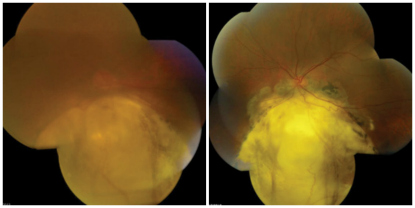
| 1, 2. Montages of our patient's OD (left) and OS (right) posterior poles.
|
Anterior segment evaluation of the left eye was significant for grade 1+ nuclear sclerosis of the lens, but otherwise unremarkable. Her intraocular pressure measured 18mm Hg OU. Dilated fundus examination of the right eye revealed a hazy view of the retina secondary to dense brunescent cataract (figure 1).
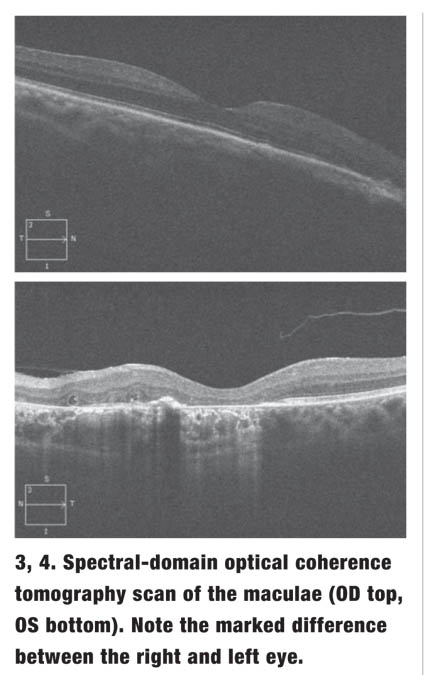
The view into the left eye was clear, which revealed a similar finding to that documented in the fellow eye (figure 2). We performed a spectral-domain optical coherence tomography (SD-OCT) scan of both eyes (figures 3 and 4).
Take the Retina Quiz
1. How do you account for the changes seen in the posterior segments of both eyes?a. Retinal atrophy.
b. Retinal detachment.
c. Progressive myopia.
d. Incomplete closure of the optic fissure during fetal development.
2. What term is commonly used to describe the funduscopic findings?
a. Chorioretinal atrophy.
b. Posterior staphyloma.
c. Coloboma.
d. Degenerative myopia.
3. Common associated ocular complications include all of the following, except:
a. Hypotony.
b. Retinal detachment.
c. Amblyopia.
d. Visual field scotoma.
4. What is the best description of the SD-OCT findings in the patient’s left eye?
a. Choroidal neovascularization.
b. Atrophy of the retinal pigment epithelium (RPE) and loss of the photoreceptor integrity layer (PIL).
c. Chronic cystoid macular edema (CME).
d. Persistent vitreomacular adhesion (VMA).
5. How should the patient be treated?
a. Monitoring.
b. Scleral buckle.
c. Enucleation.
d. Intravitreal anti-VEGF injection.
Discussion
 |
Colobomas have been reported in 3.2% to 11.2% of blind children worldwide.1 Approximately 40% of posterior segment colobomas present unilaterally, while 60% present bilaterally.1 Chorioretinal colobomas are typically located in the inferonasal quadrant and may extend to the optic nerve.1-3During fetal eye development, incomplete optic fissure closure prevents proper growth of the neurosensory retina and RPE. The choroid also fails to form correctly, because its differentiation depends on the existence an intact RPE.2,3 Thus, our patient exhibits a bare sclera without a clearly delineated retina or choroid. Defects in the optic fissure closure also frequently cause iris coloboma, which was present in our patient’s right eye. A complete iris coloboma represents a full-thickness defect involving the iris pigment epithelium (IPE) and stroma. When it extends all the way to the iris root, it appears as a “keyhole pupil.” If the iris defect involves either the IPE or the stroma, the presentation is termed an incomplete iris coloboma.2
Colobomas are associated with a multitude of systemic conditions that result from chromosomal aberrations or genetic inheritance.2 Also, patients with chorioretinal colobomas are 23% to 42% more likely to develop retinal detachments than healthy individuals.3 Further, those with colobomas are at an elevated risk for choroidal neovascularization (CNV), which can precipitate serous macular detachments and subsequent scaring. Our patient reported that she underwent a laser procedure in her left eye more than 10 years ago. But, was the laser indicated because she had developed CNV or because she had a retinal detachment? Because her eye care records were not available, it is difficult to know for sure. All we are certain about is that our clinical photographs revealed significantly more macular involvement in the left eye than in the right eye, and the SD-OCT scan showed marked RPE disruption and PIL loss OS.
A higher incidence of cataract development—including pigment clumping on the lens capsule, anterior and posterior polar cataracts, and subcapsular, cortical and total opacification—has been reported in coloboma patients.2 Other ocular conditions associated with colobomas include visual field scotomas, amblyopia and nystagmus. Visual prognosis heavily depends on the extent of foveal and optic nerve involvement.
Treatment for patients with chorioretinal colobomas includes correction of refractive error, low vision aids and proper management of associated systemic conditions. Individuals with iris colobomas can be prescribed cosmetic contact lenses. Urgently refer patients with retinal detachment or subretinal neovascularization for appropriate intervention.
We assumed that our patient’s left eye had always exhibited better visual acuity than her right eye, until she developed macular problems and underwent laser treatment. Now, the vision is equally poor in both eyes. The reduced vision in her right eye can be attributed to the extent of the cataract. Because the right macula appears anatomically normal on SD-OCT, we believe that she has a good prognosis for improved visual acuity with cataract surgery. However, it’s possible there may be an amblyopic complication, because the patient suggested that the vision in her right eye never was very good.
We discussed the options of undergoing cataract surgery OD; however, the patient elected not to have surgery at this time. We asked her to return in six months for a cataract consultation to determine whether she would benefit from surgical intervention.
Thanks to Henry Tran, fourth-year intern at UC Berkeley School of Optometry, for contributing this case.
Quiz Answers: 1) d; 2) c; 3) a; 4) b; 5) a.
1. Barnard S, Shneor E, Brauner J, et al. Bilateral chorioretinal coloboma discovered with ultra-wide field retinal imaging. J Optom. 2012 Mar;5(3):150-4.2. Onwochei BC, Simon JW, Bateman JB, et al. Ocular colobomata. Surv Ophthalmol. 2000 Nov-Dec;45(3):175-94.3. Pagon RA. Ocular coloboma. Surv Ophthalmol. 1981 Jan-Feb;25(4):223-36.

