Vision CareCheck out the other feature articles in this month's issue: - Kids and Screens: Debating the Dangers |
Amblyopia can be described as a reduction of the best-corrected visual acuity of one or both eyes, caused by conditions that affect normal visual development.1 It is not progressive and does not continue to cause further vision loss after visual maturation. Some may consider it an unavoidable disease process that results in visual difficulties in children, but amblyopia is actually a preventable and manageable condition.
While it can be treated successfully, it can also be undertreated, leaving the patient with long-term visual consequences. This article dives into the specifics of the condition and the factors at play that dictate the right treatment approach.
 |
| Vision screening in young children is crucial to identify amblyopia early and initiate timely treatment. Click image to enlarge. |
Visual Consequences
The effects of amblyopia can impact a patient throughout their lifetime, from childhood reading to adult career choices. Amblyopia affects both acuity and binocular function. For example, patients with anisometropic amblyopia may suffer from reduced binocular function on a permanent basis (e.g., monofixation syndrome).2
Additionally, the amblyopic eye has deficits of accommodation, contrast sensitivity, motion detection and hyperacuity.3,4 Some studies suggest the amblyopic eye can still retain these deficits, even with improved acuity.
Fixation stability is another known visual dysfunction in amblyopia.5 If the unsteady fixation of the amblyopic eye leads to confusion during visuoscopy assessment for eccentric fixation, amblyopia may be undetected and possibly undertreated.
Amblyopic patients also have some type of suppression. If macular or extra-macular suppression is causing amblyopia, suppression testing may help confirm amblyopia, instead of just reduced vision from pathology of the visual system.2
Types and Staging
Amblyopia is categorized into three main forms:
Refractive. Patients with anisometropia of as little as 1.50D can develop amblyopia.2 Bilateral amblyopia can occur in patients with high levels of hyperopia (4.00D or more).
Strabismic. Any constant deviation at both distance and near, as long as it is unilateral, will lead to amblyopia. This is thought to be due to a lack of macular re-enforcement from the suppression.2
Deprivation. Amblyopia can also be found in conditions that limit sensory input, such as congenital cataract, and it can be masked by concurrent pathology, such as optic nerve hypoplasia or corneal scarring.
The prevalence of amblyopia is often cited as between 2% and 3%.2 However, amblyopia may be underreported, as many families do not have access to health care. Screening guidelines and autorefractors have become tools for pediatricians and other health care providers, but the conversion of failed screenings to comprehensive eye examinations for these children is unknown.
Considering the visual maturation process, there is a critical period when insult to the visual development of children will create amblyopia. The earlier this happens, the more severe the amblyopia, especially if left untreated. Consider the child with unilateral congenital cataract, which interferes with visual development from day one, in contrast to the three-year-old who develops anisometropia and subsequent amblyopia. The visual impairment is likely to be less severe, and the treatment more successful, in the latter patient.
The debate on the age at which patients stop responding to amblyopia treatment recently made progress, thanks in part to updates from the Pediatric Eye Disease Investigator Group (PEDIG). This series of studies shows patients as old as 17 can respond to standardized treatment.6 The findings led researchers to speculate that neural plasticity allows the visual system to respond at least up to age 17, even though visual development slows by the age of seven. Nonetheless, generally speaking, the older the patient and the longer the amblyogenic factor has been in place, the more difficult the amblyopia will be to treat.
 |
|
Consider developing handouts for families to increase their understanding of the vision problems associated with amblyopia. Click image to enlarge. |
Adults with amblyopia have been known to respond to the same treatment options as children, but studies suggest limited improvement in this population. The use of levodopa, a drug used to treat Parkinson’s disease, to enhance the neural plasticity in adults showed minimal benefit for both initial treatment and sustained vision gains.7
The PEDIG studies suggest strabismic and refractive amblyopia respond similarly to treatment, so perhaps there is no difference in the type of amblyopia, only in the age of onset.4
If the amblyopia is more severe in early onset deficits, clinicians should initiate more aggressive treatment at that point.
Treatment
Evidence-based treatment trials for amblyopia exist in the literature, including the multicenter PEDIG studies. Many reports focus on moderate (20/40 to 20/100) and severe amblyopia (20/100 to 20/400) and investigate various treatment protocols, such as two hours of occlusion a day and two days of atropine a week. These are several of the available options:
Correcting the refractive error. This is often the first step for treating patients with moderate anisometropic or strabismic amblyopia, although improvement in the amblyopic eye’s vision to curative levels with this technique occurred in only 30% of trial patients.8 While many clinicians may feel this is an acceptable initial treatment, that also means 70% of patients may require additional therapies.
Guidelines for correcting the refractive errors in amblyopia management include prescribing the full cycloplegic correction for hyperopia, myopia and astigmatism and reducing the hyperopic correction, symmetrically, by up to 1.50D. With the known deficits of accommodation in the amblyopic eye, fully correcting the refractive error can be a simple starting point.
Preventing refractive amblyopia should be a consideration for patients up to age three. Consider prescribing in cases of 1.50D or more of hyperopic anisometropia or 2.50D or more of astigmatic anisometropia. It is better to intervene early rather than wait for the amblyopia to develop and cause other visual deficits.
 |
|
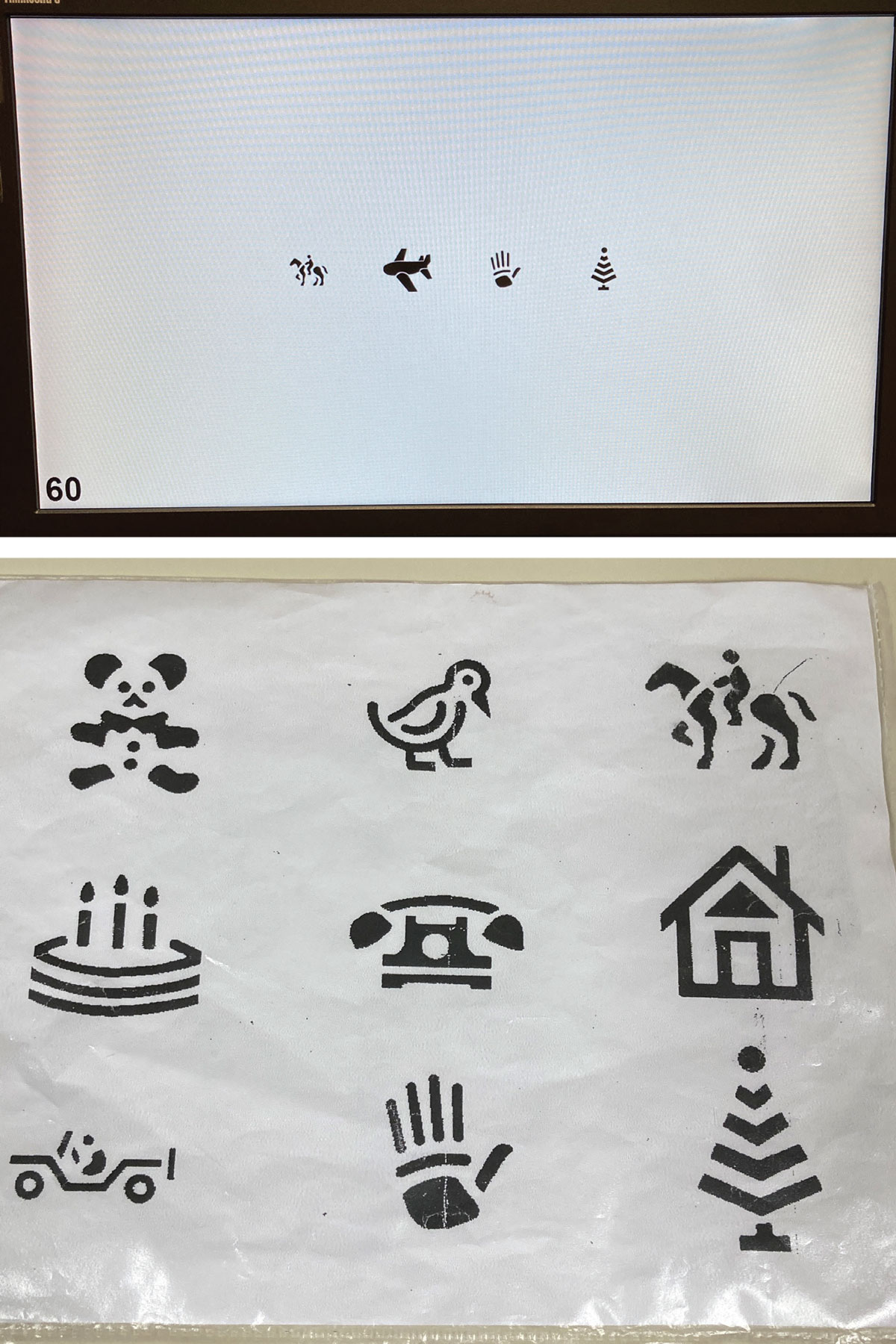
Picture acuity charts can be very useful when working with younger children. Click image to enlarge. |
Occlusion of the non-amblyopic eye. As little as two hours of occlusion a day can be as effective as six hours a day in moderate amblyopia.9 Two hours of occlusion often seems easier to manage for busy families, but even that can be a barrier to positive outcomes. For some, increasing occlusion to six hours might actually increase compliance, although more research is needed to better understand the nuances.
If a patient with amblyopia is occluding two hours a day and their visual improvement plateaus, recent studies suggest that increasing the occlusion time to six hours can help.5 One study reported that 40% of patients who increased occlusion to six hours a day showed improved vision compared with only 18% of patients who continued a regimen of two hours a day.5
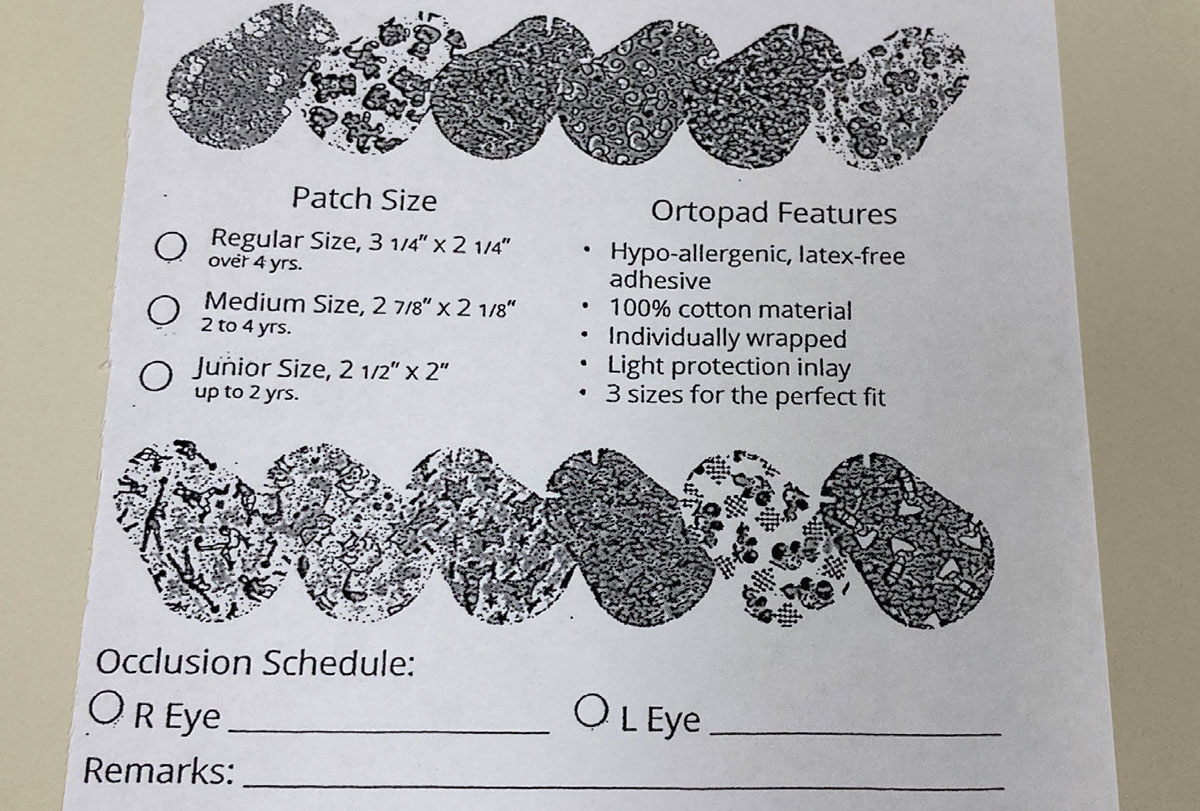
There are many types of patches available to families for occlusion treatment. The most common type of patch adheres to the skin and can be worn under a patient’s glasses. Soft patches that fit over the patient’s glasses may also be effective. Another occlusion option is Bangerter foils.
Atropine 1%. This is a proven treatment for hyperopic patients with amblyopia. One drop a day to the non-amblyopic eye can be as effective as two hours of occlusion in moderate amblyopes.1 Even weekend-only use of atropine is beneficial.1 While weekend atropine seems to lend itself to convenience and compliance, some families report remembering to use the drop every day is easier than only on weekends. Of note, the weekend regimen can be applied to any two consecutive days that work for a family.
Atropine penalization can also be augmented in patients with hyperopic refractive errors. Removing the correcting lens of the non-amblyopic eye, in addition to atropine installation as a combined treatment, can enhance the visual outcomes in some patients.
Video games. New technological treatment options have been studied, including the use of iPad games and dichoptic viewing tasks. In recent updates, these options show no superiority in treatment outcomes to patching or atropine.
Keep in mind these treatment pearls when deciding on the right path for each patient:
- Because patient and parent buy-in is crucial to treatment success, clinicians must discuss the available choices with everyone involved to ensure the treatment approach will meet the patient’s visual needs and mesh with the family’s lifestyle. This will go a long way to increase compliance and provide faster visual recovery.
- Often, clinicians can begin with a minimal treatment protocol because they can always intensify occlusion and atropine therapies for patients who do not respond or whose amblyopia does not resolve. Clinicians should set an aggressive goal of 20/20 or no more than one line of difference between interocular acuities. Do not set a low goal and discontinue treatment prematurely.
- Many clinicians monitor their amblyopic patients at five- to six-week intervals. If the patient does not show any improvement at the first follow-up visit, clinicians can monitor progress over another few visits before deciding to change the treatment plan. One study suggested making modifications after three visits with no improvement.10 When considering your options, it’s worth noting that all amblyopia treatments have shown some improvement in visual acuity and binocular function. Choose what’s best for your patient.
- Research shows treatment groups with and without a supplemental hour of near activities achieved the same visual gains.11
- For all of these therapies, the key to success is patient compliance. However, it can be difficult to know if a patient’s poor progress is due to under-treatment or lack of compliance. When following an amblyopic patient whose vision is not improving, asking about compliance should be your first step before changing the treatment approach.
Regression and Maintenance
Regression rates for atropine and two hours of occlusion are approximately 21%, and most regressions occur in the first six months. The PEDIG studies found that all regressions occurred within the first 12 months after discontinuation of treatment with no tapering.12
If a patient is undergoing maximum occlusion therapy (six hours or full-time), they have a higher chance of regressing if they discontinue treatment rather than taper treatment to two hours a day for one additional month.
 |
|
Providing patients with written occlusion instructions may help with compliance. Click image to enlarge. |
Clinicians should monitor for regression at three-month intervals to help preserve the visual gains from treatment. If regression occurs, simply restart the treatment protocol.
As the visual maturation process can occur in the first eight to 10 years of life (or longer in some patients), regression is possible for the duration of the young patient’s life. To manage or reduce this risk, clinicians can consider maintenance therapy, such as patching for two hours a day until the visual system has matured.
Key Takeaways
Detecting amblyopia can be as simple as comparing the corrected visual acuity between eyes in patients of amblyogenic age. However, amblyopia may be harder to detect in preverbal patients or in patients with concurrent pathology. When in doubt, clinicians can consider initiating treatment in the presence of any visual difference in patients of any age. A trial could be as short as three months, and, if the patient experiences improvement, the clinician can consider the visual implications of any concurrent pathology.
While current studies show binocular function improvements as visual acuity improves, other deficits from amblyopia—such as accommodation, hyper acuity and contrast sensitivity— require further evaluation regarding treatment effects.1,4,6
As with most ocular conditions, early detection and treatment are critical for the best outcomes. The first step is always a detailed discussion with the family about treatment options, and the second is proper correction of the patient’s refractive error. Clinicians should become familiar with each patient’s family, seeing as they are going to work with them a lot over the next 12 to 18 months. Remember, don’t be too hasty to end treatment, as under-treating and early discontinuation are risk factors for poorer outcomes.
Dr. Hug practices in the division of ophthalmology at the Phoenix Children’s Hospital. He has no financial interests to disclose.
1. Park SH. Current management of childhood amblyopia. Korean J Ophthalmol. 2019;33(6):557-68. 2. Nelson L, Olitsky S. Harley’s Pediatric Ophthalmology, 5th edition. Lippincott Williams & Wilkins; Philadelphia: 2005. 3. Manh V, Chen A, Tarczy-Hornoch K, et al. Accommodative performance of children with unilateral amblyopia. Invest Ophthalmol Vis Sci. 2015;56(2):1193-207. 4. Birch E, Kelly K. Pediatric ophthalmology and childhood reading difficulties: amblyopia and slow reading. J AAPOS. 2017;21(6):442-4. 5. Wallace DK, Lazar EL, Holmes JM, et al. A randomized trial of increasing patching for amblyopia. Ophthalmology. 2013;120(11):2270-7. 6. Subramanian V, Jost R, Birch E. A quantitative study of fixation stability in amblyopia. Invest Ophthalmol Vis Sci. 2013;54(3):1998-2003. 7. Scheiman MM, Hertle RW, Beck RW, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123(4):437-47. 8. Cotter SA, Foster NC, Holmes JM, et al. Optical treatment of strabismic and combined strabismic-anisometropic amblyopia. Ophthalmology. 2012;119(1):150-8. 9. Buckle M, Billington C, Shah P, et al. Treatment outcomes for amblyopia using PEDIG amblyopia protocols: a retrospective study of 877 cases. J AAPOS. 2019;23(2);e1-98, e4. 10. Keech RV, Ottar W, Zhang L. The minimum occlusion trial for the treatment of amblyopia. Ophthalmology. 2002;109(12):2261-4. 11. Sala NA, Hodde RM, Zeto VL, et al. A randomized trial of near versus distance activities while patching for amblyopia in children aged 3 to less than 7 years. Ophthalmology. 2008;115(11):2071-8. 12. Sloper J. The other side of amblyopia. J AAPOS. 2016;20(1):e1-13. |

