 |
A patient complains of burning, irritated eyes, especially late in the day after working at the computer. Sounds like classic dry eye disease, doesn’t it?
Every week I see patients like this who were diagnosed with dry eye and treated with artificial tears, therapeutics and omega fatty acids—all to no avail. After a year or two, they continue to have the same symptoms with little to no improvement. Furthermore, early diagnostic testing typically reveals common dry eye signs such as mild inferior staining, meibomian gland dysfunction and even a rapid tear film break-up time. These signs may improve with treatment, but the symptoms do not.
While their lack of improvement with traditional dry eye treatments may already have most clinicians suspicious, osmolarity testing can provide another clue. These patients will often have normal osmolarity readings in the range of 280mOsm/L to 295mOsm/L, making it extremely unlikely that they truly have dry eye.
A complicated clinical picture such as this warrants a closer look at the nervous system, because some patients who complain of dry eye with concurrent headaches, neck/shoulder pain and eyestrain when using digital devices, reading or doing near work, may be experiencing symptoms of trigeminal dysphoria. While these patients can be treated with traditional base-in prism, they now have a new treatment option with specialized contoured prism spectacle lenses.
 |
| Research now suggests specialized lenses can help patients overcome symptoms of dysfunction of the ophthalmic branch of the trigeminal nerve, trigeminal dysphoria. Click image to enlarge. Image: eyeBrain |
The Nerve Disconnect
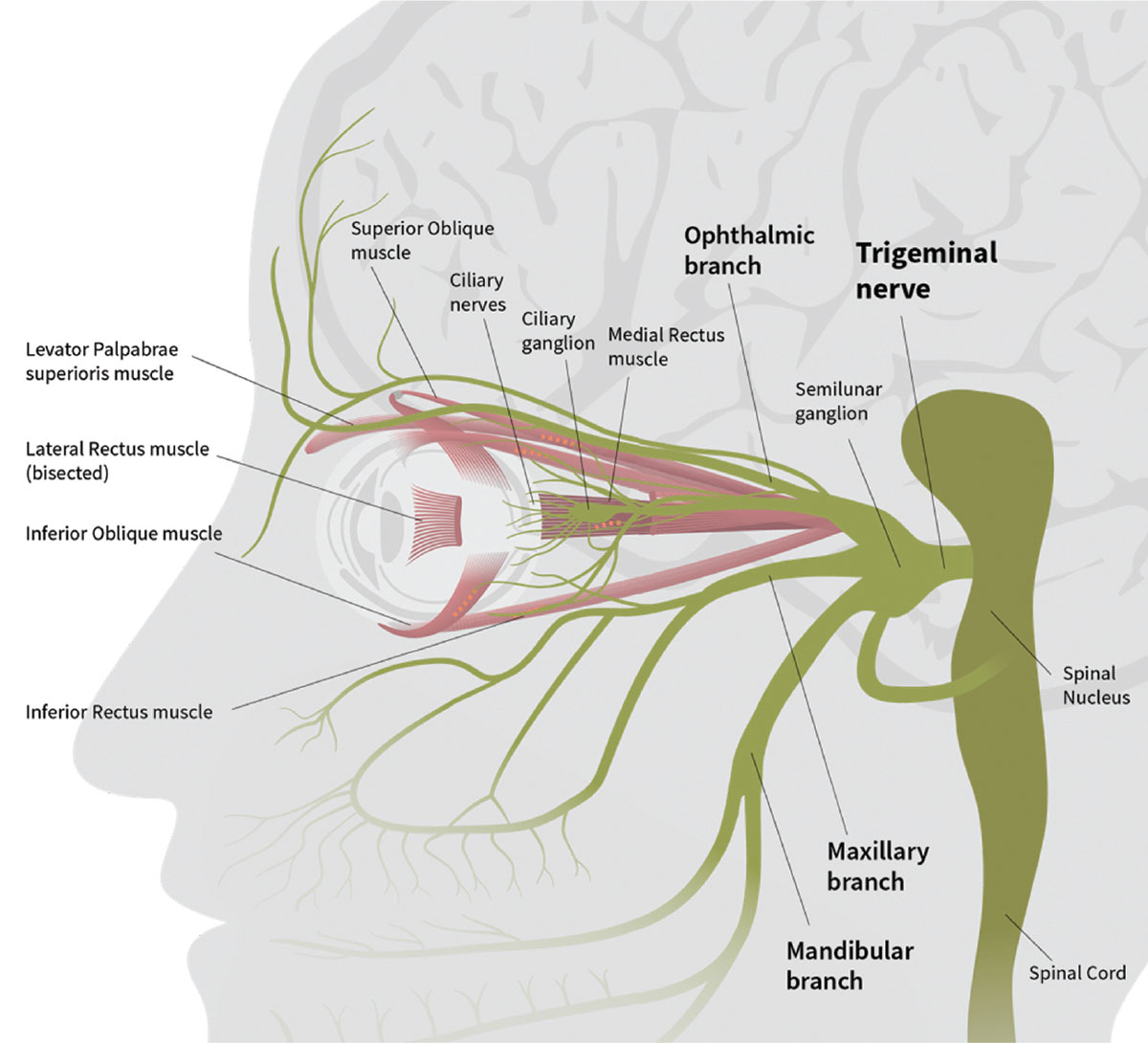
The trigeminal nerve is the largest and most complex nerve connected to the brain. It splits into three branches as it leaves the brain to innervate the eyes, nose and mouth; it also provides head and neck sensation.
Its involvement with the eye has spurred growing interest in both research and industry. Recently, for example, we have seen the introduction of nasal neurostimulation for dry eye, in which a device is used to stimulate the trigeminal nerve and increase tear production.1 Researchers are also expanding our understanding of the commonalities between neuropathic migraine and ocular pain.2 A series of clinical studies on patients with chronic headache revealed that symptomatic patients shared a common trait: a misalignment in their synchronization of peripheral and central visual tracking systems.3 Investigators have termed this condition—with its related symptoms—visually induced trigeminal dysphoria.
Researchers have long known proprioceptive fibers innervating the extraocular muscles provide afferent feedback to the brain around the location of each eye—feedback required to avoid binocular misalignments. These signals are transmitted through the ophthalmic branch of the trigeminal nerve, which is responsible for detecting sensation and reporting pain. Research now suggests these signals play a large role in the stimulation of the trigeminal nerve, resulting in symptoms such as headache, neck and shoulder pain, light sensitivity, eyestrain and dry eye.4,5
In addition, both mild exophoria at distance and convergence insufficiency are associated with trigeminal dysphoria. The degree of misalignment is much less than what is commonly classified as strabismus and often goes unnoticed precisely because it does not lead to loss of binocularity. However, the more subtle degree of misalignment greatly increases the compensatory demands on the visual system during near work, overstimulating the trigeminal nerve and causing symptoms.
Similar symptoms have been described in the ophthalmic literature for years.5-7 They haven’t been thoroughly explored until recently, likely because our highly visual, digital device-dependent world now exacerbates the condition. American adults spend more than nine hours per day on digital devices, requiring prolonged near focus and reducing the blink rate.8
Uncovering the Truth
To get to the heart of a patient’s suspicious dry eye complaints, clinicians need to be more diligent history-takers. Because headaches and neck strain are so common in trigeminal dysphoria, I have added these symptoms to my patient questionnaire, which already includes questions about near vision problems and end-of-day eyestrain. Patients often don’t connect the head and neck symptoms to their eyes and might not mention them during an eye exam without direct questioning.
In patients with symptoms that lead to a suspected trigeminal dysphoria, I begin with a cover test. I have the patient look at a distant object or letter, move a paddle from eye to eye and tell me if the object moved. If it moved with the paddle, I suspect exophoria, the most common presentation leading to trigeminal dysphoria. If it’s also present at near, I have my technicians screen for this condition with SightSync (eyeBrain Medical), the neurolens measurement device. This provides a customized measurement of misalignment from 50cm to a non-accommodative distance. The device also incorporates other ocular fusion analyses, including heterophoria, vergence conditioning, fixation disparity, accommodative convergence response and alternating monocular central fixation. Clinical research shows more than 90% of patients have a larger misalignment at near than at distance.9
In my referral clinic, when examining patients with unresolved dry eye symptoms despite treatment, we find that about 50% have three or more symptoms that could be related to eye misalignment.
Calm Some Nerves
Luckily, this new diagnosis comes with a new treatment option: neurolenses. SightSync provides precise measurements to 0.01D of prism, giving clinicians a prescription for neurolenses (eyeBrain Medical).10 These prescription lenses incorporate a contoured prism to bring the eyes into alignment. Unlike standard prism lenses, they are designed to relieve binocular misalignment at distance, intermediate and near in a single lens, in addition to correcting the patient’s refractive prescription.
In my personal experience, patients’ late-day dry eye symptoms disappear when given spectacles with neurolenses, and patients often report improvements in headache and neck strain as well. In a survey conducted by the manufacturer, 93% of patients who had previously been diagnosed with computer vision syndrome reported a reduction in symptoms, including 86% who said their symptoms were substantially reduced or “basically gone” after 90 days of wearing neurolenses.11
Patients should be counseled that it can take a few weeks for neuroadaptation, similar to what we expect when prescribing any new progressive or prism lens. Wearing the glasses all day will speed up the neuroadaptation process.
This exciting new development is twofold: the new diagnosis can help clinicians better distinguish dry eye from other masquerading conditions and the accompanying treatment can bring relief to those who have continued to struggle with these unresolved symptoms.
Dr. Karpecki is a consultant for eyeBrain Medical.
1. Friedman NJ, Butron K, Robledo N, et al. A nonrandomized, open-label study to evaluate the effect of nasal stimulation on tear production in subjects with dry eye disease. Clin Ophthalmol. 2016;10:795-804. 2. Digre KB. More than meets the eye: The eye and migraine—what you need to know. J Neuro-ophthalmol. 2018;38:237-43. 3. Miles C, Krall J, Thompson V, Colvard DM. A new treatment for refractory chronic daily headache. Data on file, eyeBrain Medical. 4. Leigh RJ, Zee DS. The ocular motor periphery. In: Neurology of Eye Movements. 5th ed. Oxfort University Press, 2015. 5. Weir CR. Proprioception in extraocular muscles. J Neuro-ophthalmol. 2006;26(2):123-7. 6. Steinbach MJ. Inflow as a long-term calibrator of eye position in humans. Acta Psychol (Amst). 1986;63:297-306. 7. Ventre-Dominey J, Dominey PF, Sindou M. Extraocular proprioception is required for spatial localization in man. Neuroreport. 1996;7:1531-5. 8. Sheikh K. Most adults spend more time on their digital devices than they think. Scientific American Mind. www.scientificamerican.com/article/most-adults-spend-more-time-on-their-digital-devices-than-they-think. March 1, 2017. Accessed July 1, 2018. 9. Indiana University School of Optometry. Cross-coupling of accommodation and convergence (AC/A and CA/C). In: Oculomotor Functions & Neurology. 2004. 10. EyeBrain. Neurolens. www.neurolenses.com/eye-care-professionals. Accessed July 13, 2018. 11. Survey of 360 neurolens patients after 90 days of treatment. Data on file, eyeBrain Medical. |

