Pediatrics in the Optometric PracticeFollow the links below to read the other articles from our report on pediatrics in the optometric practice: |
Accommodative and binocular vision (BV) conditions are about nine times more common than ocular disease in patients six months to 18 years old.1 Of these, approximately 20% have a binocular vision condition (Table 1).1
These bold statistics highlight how necessary it is for primary care optometrists to assess every pediatric patient’s BV system. Many patients with BV conditions can be easily managed in the primary care setting with a few tips.
This article streamlines the primary care pediatric exam by providing practical strategies for successfully examining children as well as BV test selection, interpretation, and diagnostic techniques.
 |
| Fig. 1. This young patient is being trialed with overminus lenses. Constant exotropia improves to intermittent exotropia with -2.00 OU. |
Exam Strategies
An attentive patient is essential to the binocular vision exam because it ensures fixation and accommodation.2,3 Consider a patient with esophoria at near who has an accommodative convergence/accommodation ratio (AC/A) of 9/1. If this patient is distracted and under-accommodates by a diopter during cover test, they might appear orthophoric, or even exophoric (relaxing accommodation increases divergence).2,3
To ensure adequate fixation, continuously engage the patient by asking questions about the target, such as, “What color is Spiderman’s face,” or “Can you see Spiderman’s two eyes?”
You can verify fixation by moving the target from side to side very slightly (1cm to 2cm), and watch for the expected pursuit movement. This is a highly sensitive technique because a pursuit movement not only requires accurate fixation but accommodation as well.
 |
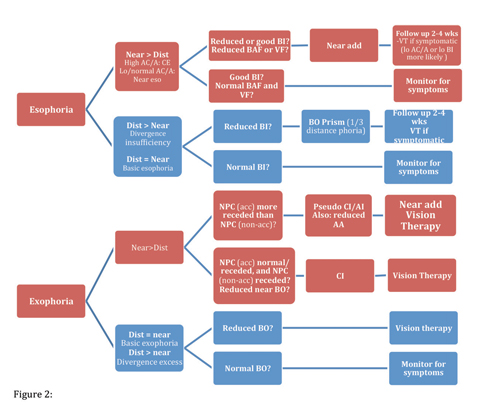
| Fig 2. Follow this sequencing chart to perform a proper BV exam. Click image to enlarge. |
Pediatric patients with BV conditions can be more passive and inattentive during the exam because the task is difficult. Explaining that the testing is like “gym class for the eyes” can encourage participation by creating a relatable analogy. If the patient responds poorly, switch to objective testing (e.g., for vergence ranges, use prism bars and watch for the expected converging/diverging eye movements).
Controlling fixation and accommodation is not difficult if the optometrist is vigilant about target selection, room lighting and verifying fixation. Targets for fixation that are small and of high contrast most effectively stimulate accommodation and encourage good fixation.2,3 Sticker targets are excellent for young children, and can be the deciding factor in the exam’s success. Stickers should be small, popular among children and include fine detailing to guarantee accurate accommodation. We have successfully had infants fixate stickers with proper engagement.
For distance fixation, parents can load a video on a smartphone or tablet computer. Normal room lighting should be employed during BV testing. The only tests where dim room lighting is indicated are binocular fused cross cylinder test (rarely used in pediatrics), retinoscopy and manifest refraction.
Pediatric patients with BV conditions do not always complain to adults because they may have no concept of what “normal” even is. To guard against this possibility, optometrists must ask probing questions during case history, and always question the family about symptoms if a BV condition is suspected during the exam.2,3
Optometrists should ask about frontal headaches, visual blur, diplopia, words jumping or moving on the page and poor attention and scholastic performance.
Case 1. Uncorrected Hyperopia with Esotropia
The patient has refractive esotropia that improves to resolution with full correction of refractive error. If the manifest refraction was prescribed without assessing the BV system, the patient would be left with a residual strabismus and anisometropia. Previously uncorrected high hyperopes will always present with reduced DVA through dry retinoscopy, because the lens is in accommodative spasm. An objective measure of refractive error is critical in the management of all pediatric patients. Final prescription is based upon binocular status, dynamic visual acuity (DVA) and age. Here are some tips to treat these patients: • Older children require good DVA for school and are given a partial prescription (offering ~20/30 OU DVA). Preschool children rely less on their distance vision because their world is at arm’s length. They can be given more of the full prescription initially. • Cut the distance prescription and prescribe a near add to facilitate adaptation. Follow up every two to four weeks and incrementally increase the prescription, as accommodation relaxes and DVA improves. If binocularity is good, the near add can be removed entirely. • In general, cut the hyperopia by the same amount in each eye from the cycloplegic refraction. However, you may not cut symmetrically initially if the prescription was, for example, +4.00 in one eye, and +0.25 in the other.2,3 |
Be Comprehensive
In a busy private practice setting, optometrists are constantly challenged to be efficient, yet thorough. However, to rule out binocular dysfunction, every primary care exam must evaluate eye alignment and fixation, eye movement skills, vergence skills and accommodative skills.2,3
To perform a BV test in a proper sequence and select sensitive tests that minimize redundancy, follow the exam sequencing succession chart provided (Figure 2). Refractive error that induces amblyopia or disrupts normal binocular functioning requires a prescription (Table 3). In children older than three years, +2.00D of uncorrected bilateral refractive error can be disruptive in some cases.2-4
BV testing is performed with the intended refractive correction in place. If no significant refractive error is found, testing is performed uncorrected.
Table 1. Most Common BV Conditions in Children1 | |||
| Accommodative (5%) | Non-strabismic (14%) | Strabismic (12%) | |
| Most common |
|
|
|
| Least common |
|
|
|
Retinoscopy vs. Autorefraction
In pediatric exams, autorefractors frequently give falsely myopic readings due to the effects of proximal accommodation.2 The SPOT (Welch-Allyn) autorefractor is the exception and produces readings similar to actual refractive error.5 Still, retinoscopy provides valuable data an autorefractor would miss.
Retinoscopy racks/sciascopy bars are useful for young children who are unable to sit behind the phoropter. Be careful to scope along the visual (foveal) axis, while maintaining working distance. Scoping off axis may result in more myopia or astigmatism. This becomes especially important when assessing patients with strabismus. A neutralizing prism should be placed over the fellow eye to help the practitioner scope on axis.2,3 Another option is to occlude the turned eye during retinoscopy to ensure the eye is fixating the target.
Table 2. Recommended Minimum Database Testing for the Primary Care BV Assessment2,3 | |||
| Test | School-aged | Preschool | Infant |
| Visual acuity | Snellen | Lea matching, picture chart | Preferential looking Fix and follow |
| Stereoacuity | Randot | Randot | Lang |
| Extraocular Muscles (EOM) | Transilluminator | Transilluminator | Finger puppet |
| Cover test (dist/near) | Letter target Dist: 1 exo +/-2 Near: 3 exo +/- 3 | Sticker target Dist: 1 exo +/-2 Near: 3 exo +/- 3 | Sticker target Hirshberg/Kappa <4 mo: phoria, <20 ET/XT >3mo: 3 exo +/- 3 |
| Refractive status | Retinoscopy Manifest | Retinoscopy Manifest | Retinoscopy |
| Near point of convergence (NPC) –Non-accommodative target | Transilluminator 7cm/10cm | Transilluminator 7cm/10cm | Transilluminator 7cm/10cm |
| Near point of convergence (NPC) –Accommodative target | Letter target 5cm/7cm | Sticker target 5cm/7cm | Sticker target 5cm/7cm |
| Accommodative amplitude | Letter target 15 – ¼(age) +/-2 | Letter target 15 – ¼(age) +/-2 | |
| Vergence facility (12 BO/3 BI at near) | Letter target >10 yo: 15 cpm +/-2 | ||
| Binocular accommodative facility (+/- 2.00) | Letter target 8-12 yo: 5 cpm +/- 2.5 | ||
Eye Alignment
An uncorrected distance and near cover test (CT) is recommended for all patients. If spectacles are being prescribed, CT may be repeated with the correction in place to note changes in alignment (Case 1). Repeating the cover test depends on the refractive error found and is not always necessary.
Case 2. Near Esophoria and Convergence Excess (CE)CT (dist) Orthophoria CT (near) 8 esophoria Retinoscopy Plano OU Near BI x/12/10 AC/A 4/1 This patient's CT is abnormal, and the compensating vergence range is near BI. This child might benefit from a near add. Binocular accommodative facility (BAF) and monocular estimation method (MEM) retinoscopy can both help determine whether the patient will be symptomatic. If symptoms persist at follow up, the child should be referred for vision therapy to increase BI reserves.2,3 CE is differentiated from near esophoria by a high AC/A. Clinically, this distinction helps the optometrist understand the utility of a near add (i.e., high AC/As respond best to adds). Newly corrected myopes often have near esophoria in the presence of accommodative insufficiency (AI) and normal BI reserves. The eso is secondary to poor accommodative skills (convergence is driving accommodation) and usually improves following spectacle adaptation.2,3 |
The expected CT results are 0-3 exo for distance, and 0-6 exo at near. Esophoria is always abnormal. Patients who deviate from expected results need to have their compensating vergence ranges, and AC/A, measured (Figures 4 and 5).2,3 Base in (BI) ranges compensate for eso deviations (norms near 11/19/10, dist x/5/3), and base out (BO) for exo (norms near 14/18/17, dist 7/15/8). Gradient AC/A is calculated by repeating CT with -1.00 OU at near. A high AC/A is defined as a change in phoria greater than 6pd, and a low AC/A is a change less than 2.2,3
CT is valuable because it is objective and can be confidently performed on most children. Always give the patient enough time to fixate and accommodate the target before moving the paddle and verify by moving the target side to side. Patients with strabismus have poor monocular skills and take longer to fixate.
Patients with symptomatic convergence excess (CE), near esophoria or accommodative esotropia frequently have poor binocular accommodative skills because they are continually relaxing accommodation to help with divergence. Hence, CT often underestimates the eso. The importance of a careful CT with a small, accommodative target cannot be understated.
Hirschberg/Kappa is a test of alignment for patients who are poorly attentive or can be used to confirm a CT finding. To perform this test, a transilluminator is held at 40cm. Typically, corneal reflections are displaced 0.5mm nasally from the center of the pupil. If the light is displaced nasally, the eye is turned out; if the light is displaced temporally, the eye is turned in. Alternately, occluding each eye verifies angle kappa (location of reflection relative to center of pupil). A displacement of the light 1mm equates to 22pd.3
 |
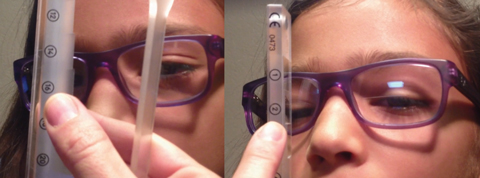
| Fig. 3. This young patient is using a polaroid bar reader and glasses as suppression checks for binocular accommodative facility testing. |
Managing Strabismus
The first question with this condition tends to be, “Is the deviation constant or intermittent, and does it alternate?”
Table 3. Amblyogenic Refractive Error2-4 | |
| Anisometropia | Bilateral |
| Hyperopia >0.75 D Myopia >3.00 D Astigmatism >1.50 | >4.00 D >-8.00 D >-2.50 D |
Establishing frequency and laterality gives valuable insight into the patient’s sensory status and guides all management decisions.3 Infants’ constant deviations that do not improve with refractive correction require timely interventions to facilitate the development of stereopsis.
If correction of the refractive error does not improve the deviation, a Fresnel prism may be considered to achieve alignment.
Surgery should be considered for infants only as a last resort due to the risks. The Infantile Esotropia Observation Study showed infants with large angle deviations who had surgery at six months had better stereo outcomes at four and a half years than those who waited until seven to 15 months.6,7
Children with intermittent deviations do not require immediate referrals because development of stereopsis is not at risk.2,3 Infants and toddlers with constant strabismus who do not alternate fixation almost always have amblyopia due to lack of sensory stimulus to the turning eye. With that in mind, in the absence of confident visual acuity (VA) measurements, commencing amblyopia therapy on this evidence alone is appropriate.2,3
Accommodative InsufficiencyThis is the most common accommodative condition among children. Patients tend to be symptomatic if their amplitude of accommodation is less than two times the dioptric working distance.2 In young children, MEM is useful for identifying symptomatic patients.2 Treating accommodative conditions. Most patients with accommodative conditions experience symptomatic relief with a near add because it reduces the need for patients to use the accommodative system (Table 4).
| ||||||||||||
Esotropia and Exotropia
Patients with esotropia at near should have CT re-performed with plus at near over the proposed distance prescription. If the magnitude or frequency improves, a near add maximizing alignment should be prescribed.2,3 Sometimes, improvement does not occur right away, especially in partially accommodative cases. Prescribing an add is always recommended in these cases. (Case 2).
Patients with exotropia at distance and near may be re-evaluated with -2.00 overminus OU. In this case, the least amount of overminus that improves the frequency of the turn at distance is prescribed.2,3,8,9 Overminus lenses are only indicated in strabismic cases and should not be used in treating convergence insufficiency (intermittent or constant exotropia at near only).
Retrospective case analyses demonstrate overminus to effectively improve eye alignment.8,9 The final overminus is tapered over time.8,9 Research into alternate patching (occluding the right and left eye for two hours every day) shows no therapeutic benefits over observation in children.10,11
 |
| Fig. 4. Diagnosis and sequential management of heterophoric binocular vision conditions. Click image to enlarge. |
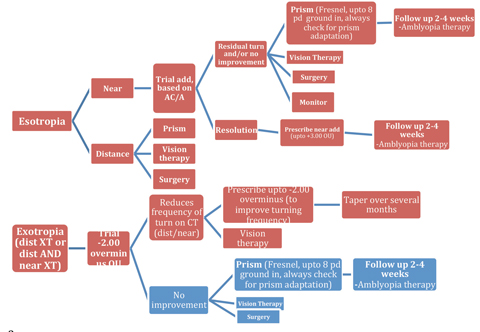 |
| Fig 5. Diagnosis and sequential management of strabismic binocular vision conditions. Click image to enlarge. |
My Five Favorite Binocular Evaluation TestsBy Megan Sumrall Lott, OD When examining children with complaints of blurred vision or strained eyes, a variety of tests can detect binocular deficit that spectacles alone may not correct. Today, more and more near point demands are being placed on children, and many are not able to meet them. These five tests can be easily administered without adding significant time to your examination: 1. COVD QOL Checklist 2. Randot Stereo Testing 3. Vergence Facility Using a Prism Stick This is performed for 30 seconds, and each change of the prism is counted. The expected result for this test is 15 cycles/minute.3 If the patient is lower than this, they may have a binocular problem. Keep in mind that some patients may suppress, so watch the eye movement to ensure that they are actually fusing two images. You should see the eyes move in the appropriate direction with each change of the prism. In particular, observe how a patient focuses while actively engaged in near tasks. 4. Spot Retinoscopy
5. NSUCO Ocular Motility Testing Dr. Sumrall Lott is founder of Belle Vue Specialty Eye Care in Hattiesburg, MS. 1. Maples W, Hoenes R. The College of Optometrists in Vision Development checklist related to vision function: expert opinions. Optometry. 2009;80(12):688-94. 2. Benjamin W, Borish I. Borish's Clinical Refraction. St. Louis: WB Saunders Co; 1998. 950. 3. Gall R, Wick B, Bedell H. Vergence facility: establishing clinical utility. Optom Vis Sci. 1998;75(10):731-42. 4. Maples W, Atchly J, Ficklin T. Northeastern State University College Of Optometry’s oculomotor norms. J Behavioral Optometry. 1992;3(6):143-50. |
Vergence and Accommodative Skills
Near point of convergence (NPC) should be performed with accommodative and non-accommodative targets (e.g., penlight). Patients with convergence insufficiency often leverage accommodation to drive convergence. Performing this test with a penlight is important because it can tease out a receded NPC.2,3 Patients with “pseudo-CI” accommodative insufficiency (AI) will show an improved NPC with a non-accommodative target.2,3
Accommodative amplitudes are measured using a push up, pull away or minus lens to blur. In young children, pull away can be efficiently performed by occluding an eye, presenting a 20/20 target close to the eye and asking the child to “guess the secret letter” as the fixation stick is slowly pulled away. The dioptric working distance is measured when the correct answer is given.
Vergence facility (VF) and binocular accommodative facility (BAF) are sensitive tests for uncovering symptomatic conditions.2,12 These tests are efficiently performed without the phoropter.
For VF, the patient fixates a 20/30 target at 40cm and alternates between fusing 12BO/3BI. The cycles per minute (CPM) are recorded (less than 12cpm is indicative of a vergence disorder).2,12
BAF is administered with +/-2.00 flippers, polaroid glasses/bar reader and a near target. Research demonstrates the importance of suppression checks to ensure continued binocularity.2 If the patient is suppressing, the target, as seen by the
suppressed eye, appears black.
Failing (+) on BAF is indicative of a convergence disorder, or AI. Failing (-) suggests accommodative excess or a divergence disorder. Decreased overall CPM may be associated with any BV condition.
 |
| Fig. 6. Constant alternating esotropia improves to 4 esophoria through +1.50 add. Click image to enlarge. |
Prescribing
A near add is indicated in most accommodative and some vergence conditions. It can be quickly determined based on the results of monocular estimated method (MEM) testing (Figure 7).
MEM retinoscopy measures binocular accommodative response. It is performed at Harmon’s distance (between child’s shoulder and elbow). MEM is performed over the subjective distance. Age appropriate targets are attached to the retinoscope and lenses are quickly dipped down to neutralize the reflex (Figure 4). Expected values are +0.25DS to +0.75DS. The add power is increased if a lag (extra plus) is noted, and decreased with a lead.2
 |
| Fig. 7. Monocular estimated method retinoscopy near target cards. |
All patients with esophoria, esotropia, moderate to high hyperopia, and accommodative spasm should undergo cycloplegic retinoscopy.2 Patients with accommodative spasm demonstrate against motion on MEM retinoscopy. The reflex switches between neutral and against motion, which may frustrate the optometrist, but is strong evidence of this condition. These patients typically have a low minus prescription in distance (<-1.00D), which reduces to plano or hyperopia on cycloplegic retinoscopy. They may also be esophoric.2,3
Patients with newly uncovered BV conditions should be followed up two to six weeks after they have been wearing their new spectacles to assess adaptation and BV status.13
Additional amblyopia therapy should not be started before the child has adapted to the spectacle prescription. Spectacle therapy is first-line intervention for amblyopia. Maximal improvement of VA occurs at 18 weeks, with 32% showing complete resolution at this time.13
The final decision to begin amblyopia therapy is based upon patient factors and clinician preference (e.g., if patching is burdensome, therapy may be deferred). Bangerter foils, patching and atropine therapy are all effective treatments. In-office vision therapy is a good option.2,14-16
An attentive child is critical for the BV exam. Children must be engaged and participating throughout to ensure accurate results. Significant refractive error must always be corrected prior to BV evaluation. For a primary care exam to be comprehensive, it must evaluate alignment, accommodation, vergence and eye movement skills. BV conditions are managed with near add lenses, prism, overminus, vision therapy or surgical referral.
Dr. Jhajj is an assistant professor at Nova Southeastern University where she teaches binocular vision, pediatric, vision therapy and primary care.
1. Scheiman M, Gallaway M, Coulter R, et al. Prevalence of vision and ocular disease conditions in a clinical pediatric population. J Am Optom Assoc. 1996;67(4):193-202. |

