 |
The eye is an extension of the brain and central nervous system. Through a simple ocular examination, we can glean significant insight into complex neurological processes. Ophthalmologic examinations thus serve as conduits through which we can detect and diagnose many underlying neurologic conditions.1
One of the anatomic conduits that connects the eye to the brain is the cavernous sinus. This structure is one of two paired intracranial dural venous sinuses located posterior to the orbit and on either side of the sella turcica of the sphenoid bone. Anteriorly, the cavernous sinus communicates directly with the superior and inferior orbital fissures and indirectly with the pterygopalatine fossa.
Its primary function is the transport of deoxygenated blood. As such, it communicates with numerous venous structures, including the superior and inferior ophthalmic veins, basal venous plexus, superficial middle cerebral vein and superior and inferior petrosal sinuses.
The cavernous sinus is so much more than a simple vein. Many important neurovascular structures travel through it due to its location between the orbit and brain proper. These include the internal carotid artery (ICA), cranial nerve (CN) III, CN IV, two divisions of CN V (1 and 2) and CN VI. All the constituents of the cavernous sinus are related to and have an effect on ocular function.2 As such, it is important we understand them.
Deep Dive
Often, observable ocular abnormalities on clinical exam aid in identifying the source, if not also the etiology, of a patient’s condition. Here’s what disruptions to the features of the cavernous sinus look like and tell us.
ICA. The common carotid artery (CCA) arises directly from the aorta on the left and indirectly on the right through the brachiocephalic artery. The CCA bifurcates within the neck, giving rise to the ICA, which continues intracranially and gives off several smaller branches.3 Surrounding the ICA are postganglionic, sympathetic fibers. The sympathetic system affects many ocular structures and is responsible for innervating the superior tarsal muscle of the upper eyelid and the pupil dilator. Sympathetic disruption may occur in cavernous sinus disease, allowing the parasympathetic system to dominate, resulting in a miotic pupil and ptosis. These features, with the addition of anhidrosis on the affected side, constitute Horner’s syndrome.4
Oculomotor nerve (CN III). Running along the superior-lateral wall of the cavernous sinus is CN III. In conjunction with the aforementioned sympathetic stimulation of the upper eyelid, CN III innervates the levator palpebrae superioris, contributing to the majority of eyelid elevation. Additionally, it innervates many ocular muscle branches, such as the superior rectus, inferior rectus, medial rectus and inferior oblique. Fibers also extend to the pupillary sphincter. As such, a lesion in the cavernous sinus affecting the third nerve causes ptosis that is more significant than in sympathetic dysfunction.
Additionally, patients may have a resting position where their eye is sitting “down and out” due to the lack of muscular innervation. If pupil involvement is present, dilation would be evident. A patient with CN III palsy may report symptoms of diagonal, binocular diplopia and a drooping eyelid, among other side effects.5
|
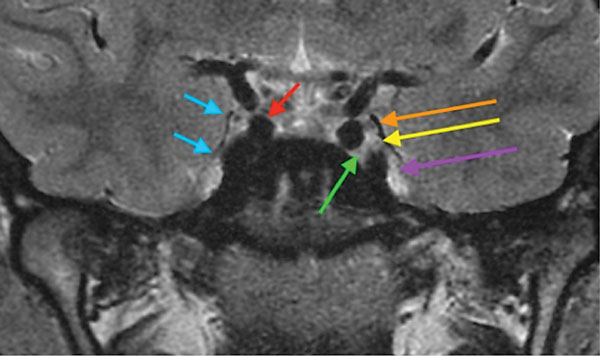
| MRI imaging of the brain through the cavernous sinus shows the lateral border of the right cavernous sinus (blue), cavernous segment of the right ICA (red), left CN III (orange), left CN IV (yellow) and left CN VI (green). The left CN V-1 and left CN V-2 are not well resolved (purple). Click image to enlarge. |
Trochlear nerve (CN IV). Subadjacent to CN III within the lateral wall of the cavernous sinus is CN IV. This nerve, after exiting the cavernous sinus, continues on its course to eventually innervate the superior oblique (SO) muscle. The SO is the sole extraocular muscle that is innervated by CN IV and functions primarily as a depressor. Secondary and tertiary functions include abduction and intorsion of the eye. Patients with SO palsies may report vertical or diagonal diplopia that is worse on downgaze. They may also have a compensatory head tilt to balance out the torsional effect.6
Trigeminal nerve (CN V). CN V consists of three branches on either side to provide sensory and motor function to the entire face. Only the first two of these branches, the ophthalmic (V-1) and maxillary (V-2), are contained within the inferior aspect of the cavernous sinus. These two divisions are primarily sensory in function. The ophthalmic division provides sensory innervation to the orbital and supraorbital portion of the face. It also supplies various ocular structures, such as the lacrimal gland, ciliary body, cornea and conjunctiva. The maxillary division innervates the infraorbital portion of the face above the mouth, as well as the maxillary teeth and sinuses.
Cavernous sinus pathology that affects the area housing these branches reduces sensation on the ipsilateral side of the face.7 This can be tested clinically using the end of a tissue or cotton wisp to stroke the area of distribution on either side while the patient has their eyes closed, to check for symmetry.
Abducens nerve (CN VI). Cranial nerve VI is responsible for the abduction of the eye. It is the most medially positioned cranial nerve within the cavernous sinus, located just slightly inferior to the cavernous ICA. After exiting the cavernous sinus, it eventually innervates the lateral rectus muscle within the orbit.
Patients with CN VI dysfunction may report horizontal, binocular diplopia due to their inability to abduct the eye.8
THE FUNCTION AND DYSFUNCTION OF CAVERNOUS SINUS STRUCTURES | ||
| Structure | Ocular Function | Ocular Dysfunction |
| ICA |
|
|
| CN III |
|
|
| CN IV |
|
|
| CN V-1 |
|
|
| CN V-2 |
|
|
| CN VI |
|
|
Take-home Message
With a clear understanding of cavernous sinus anatomy, we can see how pathology in and around the structure leads to a myriad of ocular manifestations. These pathologic conditions of the cavernous sinus typically fall into one of four categories: vascular, tumor, trauma or inflammation.2 Vascular conditions include aneurysms arising from the cavernous ICA or venous thrombosis of the cavernous sinus itself. Numerous tumors may arise from or invade the cavernous sinus, including schwannoma, meningioma, extramedullary plasmacytoma, pituitary macroadenoma and metastasis.9 Trauma may lead to the formation of a cavernous-carotid fistula. Finally, inflammation may affect the cavernous sinus in the form of idiopathic orbital inflammation, also called Tolosa-Hunt syndrome.2
Pathology within the cavernous sinus can lead to many vision-threatening scenarios. But more than that, these ocular signs and symptoms may often be the initial heralds of a life-threatening cavernous sinus syndrome. It is imperative to identify and appropriately work up suspected cavernous sinus pathology with timely diagnostic neuroimaging and referrals.
In the event that multiple cranial nerves are implicated on clinical examination, it is necessary to keep in mind this specialized intracranial compartment.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Yap TE, Balendra SI, Almonte MT, et al. Retinal correlates of neurological disorders. Ther Adv Chronic Dis. 2019;10:2040622319882205. 2. Kuybu O, Dossani RH. Cavernous Sinus Syndromes. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 3. von Arx T, Tamura K, Yukiya O, et al. The face—a vascular perspective. A literature review. Swiss Dent J. 2018;128(5):382-92. 4. Khan Z, Bollu PC. Horner Syndrome. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 5. Margolin E, Freund P. Third nerve palsies: review. Int Ophthalmol Clin. 2019;59(3):99-112. 6. Kim SY, Motlagh M, Naqvi IA. Neuroanatomy, Cranial Nerve 4 (Trochlear). In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 7. Huff T, Daly DT. Neuroanatomy, Cranial Nerve 5 (Trigeminal). In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 8. Graham C, Mohseni M. Abducens Nerve Palsy. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 9. Labib ML, Som PM. Unusual extramedullary plasmacytoma of the head and neck: a case series. Neurographics. 2017;7(2):115-20. |

