 |
A 68-year-old woman presented to the ophthalmology department after being referred by a local optometrist. She was homebound and received home care. She wore spectacles for both distance and near viewing. The doctor had diagnosed her with a nonspecific corneal infection/inflammation OD and placed her on topical antibiotics, but she failed to fill the prescriptions. Upon observation, her eye was red and photophobic. She was in substantial pain. Her vision was poor. She was COVID negative. Her systemic history was positive for poorly controlled hypertension and diabetes. She denied trauma or the use of contact lenses. She denied allergies of any kind.
Clinical Findings
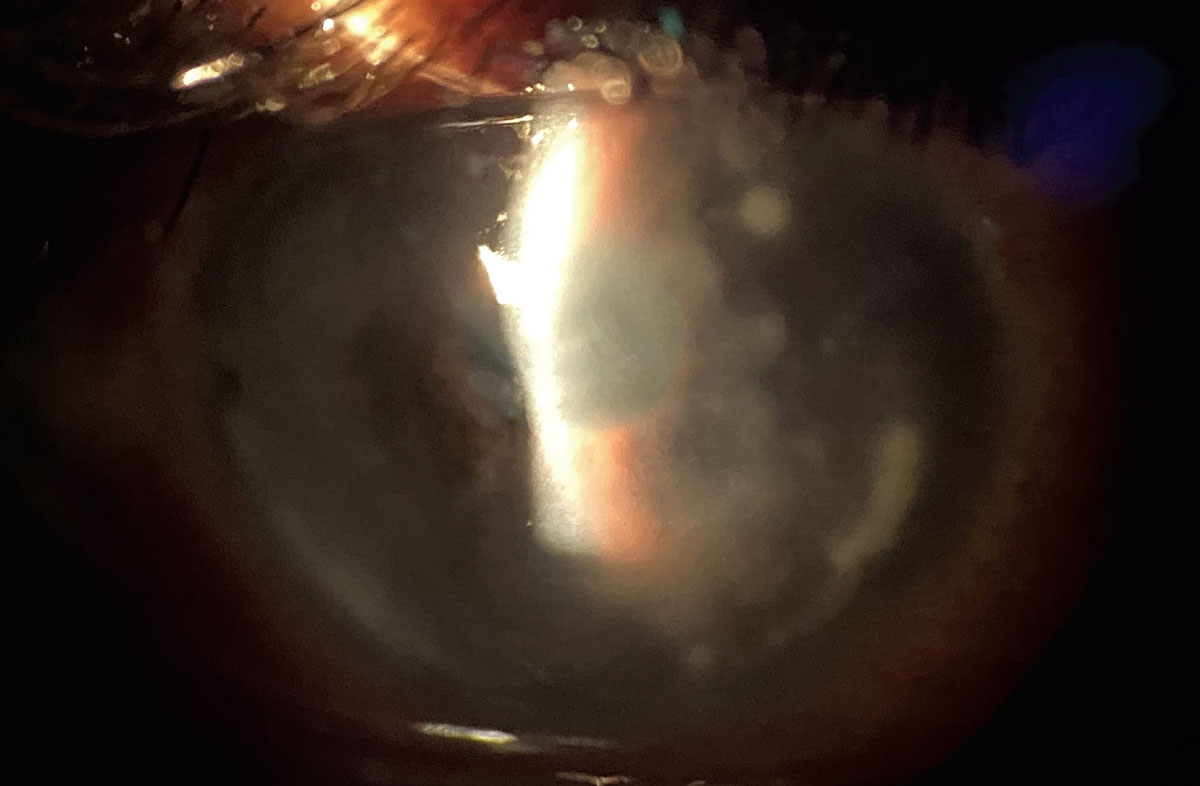
Her best uncorrected entering visual acuities were light perception at three feet OD and 20/30 OS. There was no retinoscopic reflex in the right eye. The reflex in the left eye was normal, indicating gross emmetropia. Her extraocular motilities were intact in both eyes. Her confrontation fields demonstrated awareness to finger-size isopters OD with the confrontation field in the left eye being normal. There was an afferent pupil defect in the right eye. The gross examination of the anterior segment is demonstrated in the photograph.
Her intraocular pressures measured 2mm Hg in the right eye and 16mm Hg in the left with Goldmann applanation. There was no evidence of rubeosis or ectropion uvea in either eye. The right eye was not dilated and no view of the posterior pole was possible. Dilated examination of the left eye demonstrated a cup-disc ratio measuring 0.2 round, with distinct margins and normal grounds with no macular edema or proliferative diabetic retinopathy.
 |
|
She presented with this appearance and reports of significant pain. What might be the cause? Click image to enlarge. |
Additional Testing
Dilation and cycloplegia are contraindicated in these cases. The collapsed anterior chamber indicates a full-thickness perforation. The iris apposition to the central corneal depression suggests incarceration. This should not be altered.
Corneal sensitivity was measured and found to be present only to exaggerated stimuli OD. Anterior segment photography was completed. B-scan ultrasonography was considered but postponed in favor of emergency referral to the anterior segment service of the local eye hospital. A Seidel sign was completed, demonstrating no leakage; however, it was clear the collapsed anterior chamber and forward movement of the iris created a plugging effect to the full-thickness perforation in the center of the central depression.
While no additional topical medications were recommended, in the setting of no toxic or traumatic etiology with data not demonstrating a central dense infiltrate indicating infectious etiology, vascular testing was suggested to rule out asymmetric vascular disease and vascular insufficiency on the ipsilateral side.
Diagnosis
The condition in month’s issue is diabetic neurotrophic corneal ulceration demonstrating diffuse infiltrates and central perforation with complete collapse of the anterior chamber and iris incarceration within the full-thickness corneal perforation.
Neurotrophic keratitis (NK) is generically characterized by reduction of corneal sensitivity spontaneous corneal epithelial breakdown and impairment of corneal healing.1-9 There are several known causes; included are herpetic keratitis, diabetic keratitis and keratitis or corneal breakdown secondary to ophthalmic and neurosurgical procedures.1-9
Diabetic neuropathy (DN) is the most common complication of systemic diabetes, affecting 50% patients.10 Microvascular and macrovascular complications are the pathologic hallmark of diabetes. It provokes changes in blood vessels by affecting the capillary basement membrane, including arterioles in the glomeruli, retina, skin, muscle and myocardium.10 Its complications are numerous and include acute diabetic ketoacidosis, hyperosmolar hyperglycemic states, lactic acidosis and hypoglycemia. Death can occur when these issues are not properly managed by diet, exercise and medication regimens.10 Chronic complications of poorly managed disease include diabetic nephropathy, atherosclerosis, diabetic polyneuropathy and diabetic retinopathy.10
Neurotrophic keratopathy is not an uncommon condition in patients with diabetes and is considered to be a subset of diabetic polyneuropathy.9,10 It is a sight-threatening entity caused by epithelial disturbances brought about by failing corneal metabolism when the underlying systemic condition damages the anterior segment’s neurological system.4-10
Clinical Findings
Diabetic keratopathy exhibits several clinical manifestations, including persistent corneal epithelial erosion, superficial punctate keratopathy, delayed epithelial regeneration and decreased corneal sensitivity.1-9 In the earliest and mildest forms, patients may notice compromised visual acuity; however, if left untreated it may progress and produce all of the aforementioned advanced signs with or without corneal melting (ulcer) and perforation.1-7
The mechanism of diabetic NK is trigeminal nerve (generic or ophthalmic division) damage.1-5 Diagnosis of NK in general is based upon systemic history (e.g., history of ocular surgery, upper respiratory infection, injury or poorly controlled hypertension, diabetes or history of vascular disease) and biomicroscopic examination in the setting of decreased corneal sensitivity.1-7
The slit lamp exam will uncover a red and inflamed eye with an inflamed cornea containing diffuse infiltrates and pockets of microcystic edema from corneal tissue failure.6,7 When trigeminal signaling is absent, corneal ulceration without dense infiltrate (melting) will produce progressive thinning, which can lead to perforation without the dense infiltrate characteristically seen in infectious cases.1-9
As neurological signaling becomes impaired, corneal wound healing suffers.6 Research indicates diabetic NK corneas have a reduction of and thickening of long corneal nerve fiber bundles, leading to corneal neuropathy capable of producing tissue thickening and epithelial thinning with eventual increased risk for recurrent epithelial disease (erosion/abrasion), general keratopathy or ulceration (melting).6,7,10
Generically, NK can be classified according to severity of the corneal damage as follows: stage 1: epithelial alterations; stage 2: persistent epithelial defects; stage 3: corneal ulceration.1
Treatment Options
Management of NK is based upon the clinical severity of the condition and is focused on both promoting corneal healing and the future prevention of progression (stromal melting and perforation).1-7
The presence of other ocular diseases, such as exposure keratitis (cranial nerve VII palsy, thyroid eye disease, ectropion), dry eye and limbal stem cell deficiency from toxic injury can influence the outcome of both the process and prognosis of NK. These issues will require concomitant management.1-10
While there are no specific topical or oral medical treatments that produce rehabilitation, surgical approaches such as amniotic membrane transplantation and conjunctival flap procedures are effective in preserving eye integrity.1-5 Recently, the role of growth factors has been investigated for their properties of maintaining the normal structure and function of the cornea, as well as their ability to increase corneal epithelial healing.8 Many clinical trials have shown that growth factors and cytokines can significantly enhance epithelialization (epithelial proliferation and migration), accelerating corneal wound healing.8 Recently, investigators were able to show that topical administration of insulin, naltrexone (opioid antagonist) and nicergoline (ergoline derivatives) were found to improve and significantly increase, the corneal wound healing rate.8
Case Outcome
This patient was emergently referred to the local eye hospital and failed to recover vision. It is unclear whether or not the poor outcome was related to the severity of the anterior segment disease or their noncompliance with the initial topical treatment (never filled). At the time of publication, it is unclear what actions were taken by the surgical team at the local eye hospital; however, commentary by a local cornea specialist included possible anterior chamber reformation using corneal glue with administration of topical antibiotics, topical steroids, topical cycloplegia after reformation for uveitis control with consideration for a partial or full tectonic graft procedure. The prognosis for this case was felt to be poor.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
|
1. Sacchetti M, Lambiase A. Diagnosis and management of neurotrophic keratitis. Clin Ophthalmol. 2014;8(3):571‐9. 2. Versura P, Giannaccare G, Pellegrini M, Sebastiani S, Campos EC. Neurotrophic keratitis: current challenges and future prospects. Eye Brain. 2018;10(6):37‐45. 3. Hyndiuk RA, Kazarian EL, Schultz RO, Seideman S. Neurotrophic corneal ulcers in diabetes mellitus. Arch Ophthalmol. 1977;95(12):2193‐6. 4. Priyadarsini S, Whelchel A, Nicholas S, et al. Diabetic keratopathy: Insights and challenges [published online ahead of print, 2020 Feb 22]. Surv Ophthalmol. 2020;S0039-6257(20)30029-1. 5. Lockwood A, Hope-Ross M, Chell P. Neurotrophic keratopathy and diabetes mellitus. Eye (Lond). 2006;20(7):837‐9. 6. Rosenberg ME, Tervo TM, Immonen IJ, et al. Corneal structure and sensitivity in type 1 diabetes mellitus. Invest Ophthalmol Vis Sci. 2000;41(10):2915‐21. 7. Liu XW, Pang GX, Wang Z. Zhonghua Yan Ke Za Zhi. 2005;41(10):920‐3. 8. Abdelkader H, Patel DV, McGhee CNj, Alany RG. New therapeutic approaches in the treatment of diabetic keratopathy: a review. Clin Exp Ophthalmol. 2011;39(3):259‐70. 9. Bikbova G, Oshitari T, Tawada A, Yamamoto S. Corneal changes in diabetes mellitus. Curr Diabetes Rev. 2012;8(4):294‐302. 10. Sitompul R. Corneal Sensitivity as a potential marker of diabetic neuropathy. Acta Med Indones. 2017;49(2):166‐172. |

