Q. I am involved in the care of an elderly patient with significant conjunctivitis in one eye and heavy mucopurulent discharge. Unfortunately, recent cultures and sensitivity testing reveal a multi-drug resistant Staphylococcus aureus infection. The patient has been on fortified vancomycin along with all the fourth-generation fluoroquinolones and still displays a non-resolving clinical picture. Where do I go from here?

A. The Centers for Disease Control estimates 25 to 30% of the population carries staph in the nose at any given time.1 Over the years, staph infections have traditionally been treated with penicillin antibiotics, leading to staph strains that are resistant to this type of antibiotic. These strains are dubbed methicillin-resistant Staphylococcus aureus (MRSA). The CDC reports about 100,000 people in the U.S. are hospitalized with MRSA infections each year. The incidence of infection with methicillin-resistant staphylococcus aureus has rapidly increased over the last twenty years.2
This patient is likely colonizing a staph bacteria in the skin or naso-pharynx. In this case, a culture of the patients nasal mucosa may confirm the source of infection.
Some patientsincluding healthcare workers, the elderly or very sick patientsare more likely to acquire these infections than others. Patients who harbor the bacteria are often in nursing homes, immun-osuppressed or immunocompromised. The CDC also says certain factors can put some people at an even higher risk for infection:1
Prolonged hospital stay, especially in an intensive care or burn unit.
Use of broad-spectrum antibiotics.
Close contact with MRSA patients.
Recent surgery.
Active skin disease.
Crowded living conditions.
MRSAs have traditionally been successfully treated with vanco- mycin. However, the overuse of this antibiotic may have contributed to development of VRSA, vancomycin-resistant Staphylococcus aureus. The first VRSA case was reported in a patient in June 2002.3 The CDC has recorded a total of 10 infections of VRSAs or VISAs (vancomycin-intermediate S. aureus.) However, all cases have been treatable with other medications.5
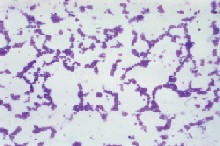
Microscopic view of Staphylococcus aureus bacteria. Centers for Disease Control.
Fortunately, topical agents achieve much higher threshold levels than systemic treatments, and some topicals are often potentially sensitive even when comparable systemic treatments are not. In our case, the patient may actually be re-infecting herself. Treatment with Zyvox (linezolid, Phizer), an oxazalidinone or fortified bacitracin may be helpful.
If you encounter a patient with VRSA, contact your local or state health department and the CDC. The CDC notes that patients who develop VRSAs generally have several underlying health conditions (like diabetes and kidney disease), previous infections with MRSA, tubes going into their bodies, recent hospitalizations and recent exposure to vancomycin and other antimicrobial agents.5
The CDC has published recommendations for systemic infections intended to reduce the development and transmission of VRSAs. Some of these include isolating the patients in a private room, minimizing the number of people caring for the patient, and using infection control precautions during patient care.6 Its also important to educate the patients relatives and friends about the need for proper hygiene, because those in close contact may also be harboring the organism.
1. Centers for Disease Control, MRSA-Methicillin Resistant Staphylococcus aureus Fact Sheet. www.cdc.gove/ncidod/hip/Aresist/mrsafaq.htm.
2. Da Silva Coimbra MV, Silva-Carvalho MC, Wisplinghoff H, et al. Clonal spread of methicilin-resistant Staphylococcus aureus in a large geographic area of the United States. J Hosp Infect 2003 Feb;53(2):103-10.
3. Chang S, Sievert D, Hageman J, et al. Infection with Vancomycin-resistant Staphylococcus aureus containing the vanA Resistance gene. NEJM 2003;348:1342-7.
4. Ultili R. Gram-positive bacterial infections resistant to antibiotic treatment. Ann Ital Med Int 2001 Oct-Dec;16(4):205-19.
5. Centers for Disease Control, VISA/VRSA, Vancomycin-Intermediate/Resistant Staphylococcus aureus Fact Sheet. www.cdc.gov/ncidod/hip/ARESIST/visa.htm.
6. Hageman J, Fridkin S, Jernigan D, Tenover F. Investigation and control of vancomycin-intermediate and -resistant Staphylococcus aureus: A Guide for Health Departments and Infection Control Personnel. Centers for Disease Control and Prevention, Atlanta GA 2003.

