Zoom in on Contact LensesThis August issue is our 46th annual contact lens report, where we help you use new and old techniques to improve your fitting skills. Check out the other featured articles here:
|
As the world population ages and lives longer, more and more presbyopic patients are going to fall into your chair. It’s up to you to know how to proceed when they do. From my years of experience working in this particular field of care, I have devised a set of guidelines that, when followed, will help set you up for the best possible results.
Here, I’ll outline the suggested steps for success, as told through a theoretical patient: Ms. Lopez, who was referred by a colleague for presbyopia management.
1. Check Your Attitude
First, express your willingness to help the patient. A successful multifocal lens fitting starts with a positive attitude toward engaging them and a strong desire to achieve optimal results.1 Indeed, Ms. Lopez will be hard to convince to give multifocal lenses a try if you don’t seem convinced yourself. The patient’s motivation remains a key factors in the transition to this modality.2
How you frame the multifocal lens talk is very important in making a good first impression. Avoid the term “compromise.” This commonly used word tells the patient that they will have to give up some of their vision or comfort while also paying more money for their lenses. Not appealing. Focus on the positives. Let patients know that, with modern designs, presbyopes tend to find multifocal contact lenses easier to adapt to than multifocal spectacles, one of which they will inevitably need.
To involve the patient, I outline the lens fitting process with a team approach. My responsibility is to provide the patient with the best lens design considering their refractive status and visual needs. I focus on the importance of balance between distance, intermediate and near vision. The patient is asked to report any signs or symptoms they experience during the first 10 days following lens fitting after neuroadaptation takes place. Achieving equilibrium by balancing distance, intermediate and near vision, knowing that changing one will affect the others, is the goal. Thus begins the process of finding a set of parameters that will allow us to achieve optimal vision at all distances.
At the same time, don’t underestimate the importance of taking a proactive approach and talking about presbyopic correction options with patients who will eventually reach this reality. From ages 38 to 40, near vision can become difficult for some patients, especially if they have introduced increasingly long hours of screen time into their life. We have a duty to provide education about changes that occur to the visual system with time and which options should be considered to ease this transition. Many patients give up contact lens wear altogether because they begin to face difficulty or experience eye strain seeing at near, and they are not aware that the problem can be solved with multifocal lenses. This is where ODs come in. We must intervene before this process begins.
It is also important to suggest contact lenses as a mode of correction for candidates who are currently wearing glasses. Initiating the conversation is important; don’t wait for the patient to bring it up. Almost 40% of glasses wearers are interested in lenses but don’t mention it at the time of their visit and would benefit from OD guidance, as would we in the form of practice growth.
Why is it important to convert these patients to lenses or keep those already in lenses committed? Because patients who wear contact lenses, even part-time, are the most profitable to our practices. They spend 2.3-times more money than spectacle wearers and are more loyal, consulting every 14 to 16 months rather than every three to four years.3
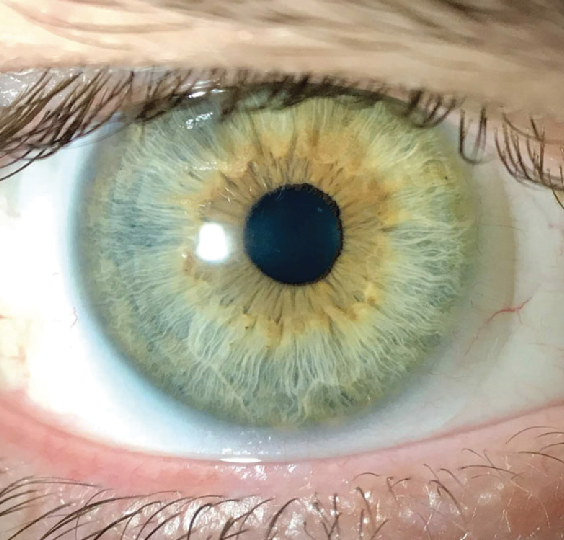 |
| Multifocal contacts offer a good option for presbyopes, often more so than spectacle lenses. Photo: Alex Nixon, OD, MS, and Erin Rueff, OD, PhD. Click image to enlarge. |
2. Ask Insightful Questions
Case history reveals that Ms. Lopez has very high expectations and wants her visual needs fully met. She doesn’t want to wear glasses because she feels they age her. She tried soft contact lenses previously but was not satisfied with her vision. She is a manager and travels between several stores for work. Distance vision is therefore crucial, both for day and night driving. She reads a lot of reports sometimes in small print, and she regularly reviews data on her phone or tablet sometimes in challenging light environments. She is open to any type of lens that may help her and is even willing to consider refractive surgery.
The most important part of any eye examination is the case history.4 Too often, the patient questionnaire is limited to a few routine questions that don’t really give us much direction. If you let the patient express their concerns, even for as little as 90 seconds without interrupting them, you will be surprised what you learn. Most of the time it will not even take 60 seconds to get on the same page.5
Encourage patients to talk about their symptoms. Many patients who experience discomfort with their contact lenses do not talk to their eyecare professional about it, considering it to be routine and normal, which could lead to dropout.6 More focused patient questions identify yellow flags before they turn red. Only once you’ve been alerted that something is wrong can you act on it.
With multifocal lenses, it is even more important to identify the patient’s visual needs and document their history. Understand patient expectations to better meet them, and set your own. Patients who we refit into multifocal lenses have already experienced contact lens wear and, accordingly, have higher, predetermined expectations. Find out which lenses worked for their vision and comfort. New candidates for contact lenses will come at the fitting process differently as first-timers. They are unsure of what to realistically expect, so the possibilities offered by modern technology need to be clearly defined, namely the unfamiliar adaptation period associated with multifocals.
The patient’s visual needs must be well-targeted. In what circumstances will the lenses be used—work, sport, social activity, specific hobbies? Some sports require high precision (archery), good distance vision (cycling) or both (golf). What visual tasks will be involved? Reading a book, using a screen, meeting with a team, driving? Do the activities take place during the day or in the evening? In normal or dim light? A truck driver working through the night will not have the same lens design as a football player or someone who works at a computer during the day.
3. Take Reliable Data
Performing an accurate refraction is crucial to achieve success with presbyopic contact lens fitting. It starts habitually with retinoscopy, which has unfortunately become a lost art. Instead, most practitioners rely on electronic refraction as a starting point. This method can offer some accuracy in cases where the cornea is normal and accommodation is well controlled. However, if the cornea is irregular or the patient over-accommodates, electronic refraction becomes unreliable.7
 |
|
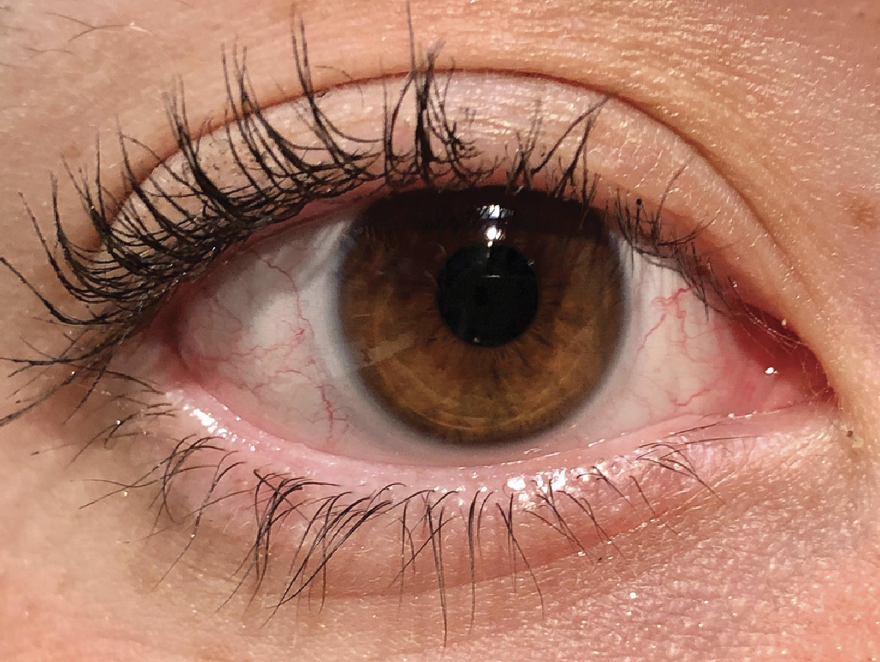
A successful multifocal lens fitting goes back to a thorough patient history and evaluation of signs and symptoms. Photo: Erin Rueff, OD, PhD. Click image to enlarge. |
Retinoscopy, on the other hand, is never misleading when done properly. It often provides elements (quality of the light reflex, for example) that cannot be quantified but are very useful clinically. How else can we detect the 38-year-old patient who is over-corrected in a concave lens, masking a hyperopic-toric over-refraction, and has 20/20 distance vision but complains of eye strain when working on the computer? Not taking advantage of this option likely means missing the opportunity to refit this patient in less concave toric lenses which will restore visual comfort and alleviate a potential dropout.
Then, you must refract the patient to the best of your ability. In the case of pre-presbyopes and presbyopes, we must not over-minus the patient and aim for maximum convex refraction at distance.8 For near vision, make sure to measure the value of the addition according to the functional reading distance. A patient who looks at a tablet at 33cm all day as a salesperson may not be well-corrected at near if assessment occurred at 45cm.
Another tip to assess near vision: throw away the reading cards. Everyone wants to read the smallest row of letters, which is a perfect recipe for overcorrection at near. I now ask the patient to pick up their phone and try to read their texts or emails at their habitual reading distance, with their regular font and letter size. This is a more realistic target, especially during multifocal lens trials, and helps instill confidence in the patient who now feels that this lens option will work for them on a daily basis.
Finally, I always use refraction to measure dominance. Once all the refractive phases have been completed, I have the patient look at the 20/30 line and blur their vision with the retinoscopic lens (+2.00D), alternating between the two eyes. The patient then tells me which combination is more comfortable, allowing me to identify the dominant and the dominated eye. This is useful information to keep in mind during the fitting process.9
4. Correct for Astigmatism
One of the most important refractive considerations is to fully correct any clinically significant astigmatism.10 Correcting astigmatism gives accuracy, especially at near where it is important for presbyopic patients. On the contrary, masking astigmatism requires increasing concavity, therefore taking a toll on vision at near.
Ms. Lopez is moderately myopic, astigmatic and presbyopic in both eyes and slightly over-corrected based on her last prescription. She has never heard the term “astigmatic” and most likely was never fitted to fully compensate for her refractive error.
In our patient’s case, try a toric lens and evaluate the subjective response. I have had patients -8.00 -0.75x60o who had a “wow” effect when fitted with toric lenses, and I have had others -2.50 -1.25x180o who saw no difference. Obviously against-the-rule astigmatism is more challenging, but a trial of toric lenses should be considered as soon as 0.75D or more of refractive astigmatism is reached. Several products now exist in soft toric multifocal lenses and should be considered right off the bat for astigmatic patients.
Similarly, hybrid multifocal lenses provide good correction of corneal astigmatism while using a spherical lens.11 Extended depth-of-focus technology is an interesting addition to the hybrid lens profile, and empirical ordering makes this process simple. For more advanced cases, spherical multifocal scleral lenses can compensate for higher levels of corneal astigmatism with the help of the fluid reservoir. The option to design lenses with decentered optics also helps to optimize the results.12
5. Treat the Tear Film
When thinking about fitting contact lenses or assessing a current wearer, remember that the tear film is the primary refractive surface of the eye. A disturbed and unstable tear film is associated with fluctuating vision and loss of contrast sensitivity—a recipe for failure in multifocal lens wear.13 Ms. Lopez has a reduced tear breakup time and a normal tear secretion, but she wears mascara and eye liner that leave an oily layer on her tear film and obstruct her meibomian glands. Makeup habits must be modified and lid hygiene therapy must be done before successful lens wear can be achieved.
It goes without saying that a detailed eye exam should be conducted before fitting a presbyopic patient. Many physiological changes occur in middle-aged patients, and hormonal changes can influence the balance of the tear film. Any cause of marginal dry eye, which is only increased by lens wear, should be proactively treated. Selection of the material, its wetting angle and wearing mode is heavily influenced by ocular health. Thus, a more fragile eye with persistent marginal dryness, despite treatment, will be better suited to materials with a lower coefficient of friction, a very low angle of wettability in rigid lenses and a daily disposable mode of wear in soft lenses.14
6. Personalize the Lens Fitting
 |
|
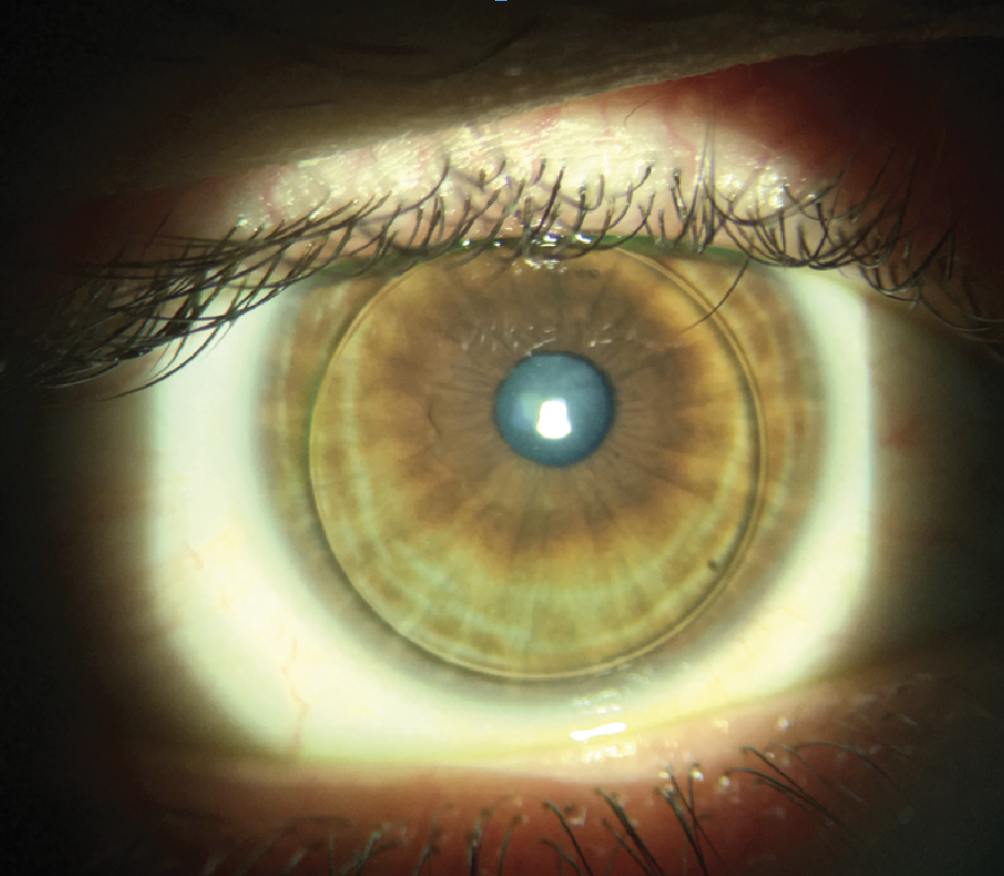
The transition to multifocal contact lenses is made smoother by educating patients and setting expectations. Photo: Robert Ensley, OD, and Jessica Jose, OD. Click image to enlarge. |
We all have a preferred brand/design of multifocal lenses that we are most comfortable working with and that will lead to success more often than not. The obvious trap is offering this option to every presbyope who sits in our exam chair.
Instead, we should keep all doors open. We must familiarize ourselves with all possible options, not neglecting rigid, scleral or hybrid lenses, which can represent excellent alternatives. That was the case here, and Ms. Lopez was fitted with the newest design of hybrid multifocal lenses.
It is one thing to know that X, Y and Z lenses are aspheric with a near-centered design. But it is another to know that the X-lens has an intermediate zone—a plateau—that covers intermediate vision at 50cm to 60cm, which the other lenses do not have. This lens is ideal for the patient who works on a computer all day long. The Y-lens is designed to fit the patient’s pupil and their prescription, offering an optimized combination according to the degree of myopia and the patient’s age. This lens is ideal for older patients who want to wear their lenses for outdoor activities, as it comes with a UV filter. The Z-lens with a center-distance design is better suited for emerging presbyopes. This is an ideal option for the patient who works for a shipping service and is looking for some relief when working in his notepad and driving at night.
7. Use Your Resources
I know several colleagues who feel they have developed enough clinical experience to fit multifocal lenses without any guidance. They have composed their recipe and are convinced that with it, success is all but guaranteed.
I have fallen victim to this attitude in the past, but in recent years my approach has changed. Without denying my competence and that of my colleagues, it is becoming very difficult to apply homemade recipes to designs that have been developed and refined with hundreds of patients. Modern multifocal lenses are optically complicated and must be used as they were designed. Otherwise, a very good product may fail to provide the intended positive outcome.
Lens manufacturers offer fitting guides that have proven effective after passing many tests. They know the limitations of the optical profiles they offer and can help professionals achieve the best possible results. Do not hesitate to consult with allies in our field such as these.
Following clinical fitting guidelines saves chair time and improves the patient experience.9 Don’t run a patient around in circles because you failed to do this, promising that the next time will be better. Your patient’s time is as valuable as yours, and multiple lens failures will surely make them doubt their adaptation ability and your overall competency.
Multifocal soft, hybrid and scleral lenses must be stable and centered to provide the best performance. It is important to validate the lens position and movement under the slit lamp. Soft multifocal lenses are expected to move less than spherical lenses while keeping the tear exchange unaltered. The push-up test is important to perform in this stage.
Centration can be established by performing topography on top of the lens.15 The design of the lens becomes clear, and the position of the optical axis vs. the visual axis can be determined. In the case of significant decentration with soft lenses, another design must be selected entirely as different base curves and diameters within the same brand are not offered. In hybrid and scleral modalities, modification of lens parameters can help to fix this issue. The sagittal depth of the soft lens will offer the most significant guidance.16 Keep in mind that lenses must ideally be fitted with 100µm to 200µm overvaulting the ocular sag height (3200µm @ 14mm and 3600µm @ 15mm of chord).17
Takeaways
With a wider range of products than ever before in soft, hybrid, rigid corneal (gas permeables) and scleral lenses, presbyopia correction is more than possible with contact lenses. Success can be significantly increased by adopting a positive attitude, talking to patients about their options, listening to their needs and directing them to the right product. Personalizing our care can make all the difference.
We must complement our approach with reliable refractive data and lens fitting in accordance with manufacturer recommendations. By using the right words, justifying our choices and teaming up with patients, it is possible to find the balance that will allow for successful multifocal lens correction. This keeps our patients happy in lenses, and it helps our practices remain economically healthy.
Dr. Michaud is the dean of the School of Optometry at the L’École d’optométrie de Université de Montréal. He is a Diplomate of the American Academy of Optometry and a Fellow of the British Contact Lens Association, the Scleral Lens Education Society and the European Academy of Optometry. He has received honoraria from Bausch + Lomb, CooperVision and Acculens.
1. Compton JE. Get prepped for multifocal success. Modern Optometry. modernod.com/articles/2022-jan-feb/get-prepped-for-multifocal-success. |