 |
A 68-year-old Caucasian male presented with acute vision loss for eight days. He described a sudden and painless decline in right eye visual acuity that had remained stable since onset. He denied associated flashes, floaters, light sensitivity, recent trauma or any symptoms in the other eye. His past medical history included hypertension, which was controlled with lisinopril, metoprolol and furosemide. He had no known drug allergies and noted an unremarkable eye exam one month prior.
Upon examination, his uncorrected visual acuity was counting fingers at four feet OD with no pinhole improvement and 20/70 OS with pinhole improvement to 20/30. The pupils were equally round, but there was a marked relative afferent pupillary defect (rAPD) in the right eye. Confrontation visual field testing revealed a central scotoma with peripheral constriction in the right eye, but was normal in the left eye; extraocular motilities were full. Intraocular pressure (IOP) was 12 mm Hg OD and 13 mm Hg OS. The patient was pseudophakic OU and had an otherwise unremarkable anterior segment exam. Dilated fundus exam of the left eye was completely normal. The right eye, however, showed findings, as seen in Figures 1 and 2.
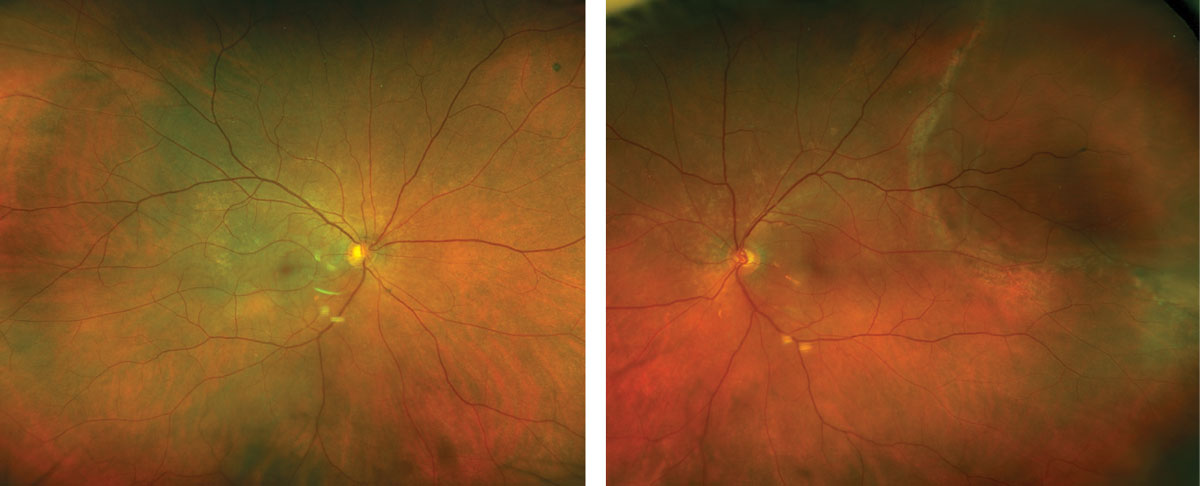 |
Figs. 1 and 2. Ultra-widefield fundus photography of the right eye (left) and left eye (right). Click image to enlarge. |
Take the Retina Quiz
1. Which of the following best describes the OCT of the right eye?
a. Central inner-segment/outer segment loss.
b. Inner retinal thickening and hyper-reflectivity.
c. Inner retinal thickening and intraretinal fluid.
d. Outer retinal thinning/atrophy.
2. What is the diagnosis for the patient's vision loss in the right eye?
a. Branch retinal artery occlusion.
b. Carotid retinal artery occlusion.
c. Central retinal artery occlusion.
d. Ophthalmic artery occlusion.
3. What would be the most appropriate next step in the management of this patient?
a. Intravitreal bevacizumab in the right eye.
b. Observation.
c. Pars plana vitrectomy in the left eye.
d. Transfer to emergency room.
4. What is the most likely visual prognosis of this patient's right eye?
a. 20/40 or better.
b. Counting fingers.
c. Full recovery back to baseline.
d. No light perception.
5. Which of the following is not considered conservative standard treatment?
a. Anterior chamber paracentesis.
b. Intra-arterial tissue plasminogen activator.
c. Ocular hypotensive eye drops.
d. Ocular massage.
For answers, see below.
Diagnosis
The fundus exam of the right eye revealed mild retinal whitening of the posterior pole with a subtle cherry-red spot, suggestive of a central retinal artery occlusion (CRAO). Of interest, he also had a superotemporal macula-on retinal detachment with a complete pigment demarcation line in the left eye, suggesting chronicity; this was an incidental finding and completely unrelated to his vision loss (Figure 2).
OCT of the right macula showed diffuse inner retinal thickening and hyper-reflectivity without intraretinal or subretinal fluid, consistent with a CRAO. The left eye was normal.
Given the diagnosis of a CRAO, we initiated an emergent transfer to the emergency department for an immediate systemic work-up. Imaging of the brain, head, neck, heart and serology testing for giant cell arteritis (GCA), was negative. However, urinary toxicology screening revealed the presence of cocaine metabolites. The cardiology team felt that the most likely etiology of CRAO in this patient was vasospasm in the setting of cocaine use.
Discussion
While the true incidence of CRAO is not known, it is estimated to comprise about one out of 10,000 cases at tertiary care referral centers.1,2 There is a male predilection and it is more common in older adults with an average age of 60; over 90% of cases are in patients over the age of 40.1,2 The disease largely presents unilaterally with potential for sequential eye involvement, but rarely presents simultaneously and bilaterally in 1-2% of cases.1,2
The pathophysiology of arterial obstructions is primarily via one or a combination of the following five mechanisms: embolism, vascular narrowing, thrombosis, arterial spasm and reduction in blood flow caused by carotid or ophthalmic artery obstruction, systemic hypotension or elevated intracranial pressure.3
Typically, patients retain at least light perception vision; thus, in cases of no light perception, choroidal circulation has likely been compromised due to carotid or ophthalmic artery obstruction.3 Rubeosis iridis at presentation should raise suspicion for concomitant carotid artery obstruction.1
Clinically, the site of arterial obstruction is only visible in 20% to 25% of cases, suggesting that thrombotic events are more frequently the etiology of CRAOs compared to embolic events.2 Other causes of CRAO include vasculitis (i.e. GCA), optic neuritis and local trauma.2
On clinical exam, the earliest signs are diffuse retinal whitening of the posterior pole with a central cherry-red spot, as mentioned earlier. Retinal whitening indicates acute retinal ischemia and represents opacification of the retinal nerve fiber (RNFL) and ganglion cell layer (GCL).3 The foveola is perfused by the underlying choriocapillaris, so this normal tissue appears cherry-red in contrast to the surrounding hypoxic tissue; normal retinal transparency typically returns two to three weeks after onset.1,3
Peripheral retina typically appears grossly normal due to thinner RNFL and GCL.1,3 Other possible vascular signs include arteriolar narrowing, boxcarring or segmentation; arteriolar emboli may also be visible on clinical exam.3 Typically, a marked rAPD can be observed within seconds of onset.3
The natural disease course results in optic atrophy, inner retinal atrophy, retinal arterial attenuation and cilioretinal collaterals.1 About 20% of patients may develop neovascularization (anterior segment more commonly than posterior segment) typically four weeks after onset.1,5
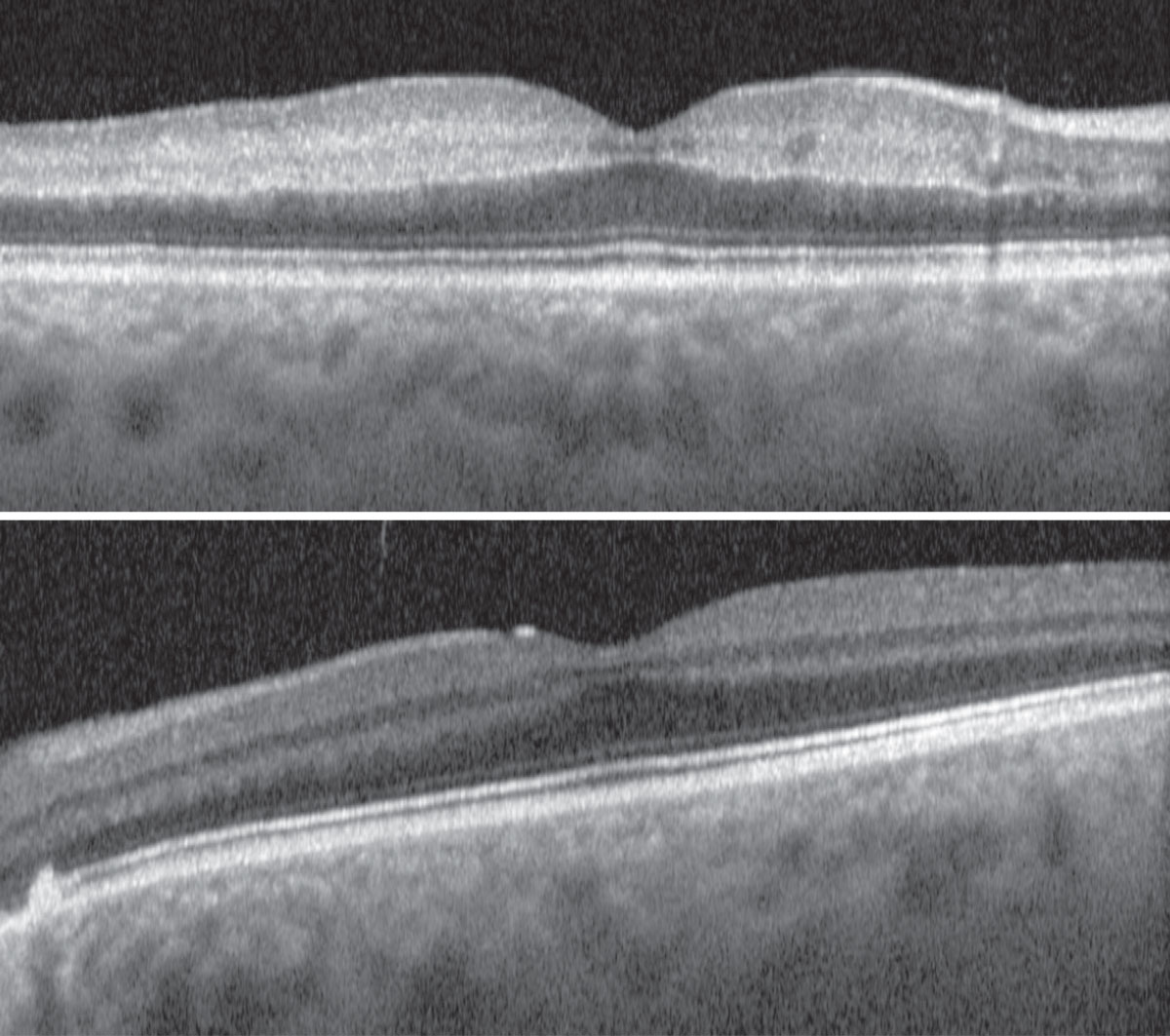 |
| Figs. 3 and 4. OCT of the right eye (top) and left eye (bottom). Click image to enlarge. |
Treatment
The vision loss from CRAO is severe and irreversible with no proven effective treatment options. Due to the rapidity of tissue damage, attempted intervention may only be indicated if patients present within a few hours of onset. The optimal window has been reported to be within the first 100 minutes, but some clinicians feel that there is still indication to treat within the first four to six hours. Unfortunately, most patients tend to present an average of one week after symptom onset.1,6
CRAOs are true ophthalmic emergencies and require immediate transfer to the nearest hospital for complete stroke work-up and neurology/cardiology consultation to rule out underlying, impending or concomitant disease (i.e. GCA or cerebrovascular accident).1,5,6 Patients with CRAO are at greatest risk for systemic morbidity within the first seven days after symptom onset, which makes their often delayed presentation problematic.6
If primary etiologies for CRAO are uncovered during systemic evaluation, they should be treated appropriately in efforts to spare the fellow eye. Otherwise, conservative standard treatment aims to aid retinal reperfusion through procedural or pharmacologic means. Options include ocular massage (digital or contact gonioscopy lens compression) or rapidly decreasing IOP with topical and/or systemic meds, or with anterior chamber paracentesis.5, 6
In general, these patients require long-term follow-up to monitor for neovascularization in the affected eye, as well as to ensure optimal ocular health in the fellow eye. Monocular precautions should be discussed (protective eyewear/polycarbonate lenses) and a low vision referral is warranted.
Our patient returned one week later for evaluation. He was counseled on the guarded prognosis of the right eye and the need to monitor for complications such as neovascularization. The decision was made to closely monitor him at this time given the asymptomatic nature and signs of chronicity.
Retina Quiz Answers
1: b; 2: b; 3: d, 4; b 5; b
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
| 1. Schachat AP, Wilkinson CP, Hinton DR, et al. Ryan’s Retina, 6th Edition. Elsevier. 2018. 2. Yanoff M, Duker J. Ophthalmology, 5th Edition. August 9, 2018. 3. Gass JDM. Stereoscopic atlas of macular disease: a fundoscopic and angiographic presentation. January 1, 1970. 4. Sharma S, Naqvi A, Sharma SM, et al. Transthoracic echocardiographic findings in patients with acute retinal arterial obstruction. A retrospective review. Retinal Emboli of Cardiac Origin Group. Arch Ophthalmol 1996;114(10):1189-92. 5. Bagheri N, Wajda B, Calvo C, Durrani A. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 2016. 6. Schumacher M, Schmidt D, Jurklies B, et al. Central retinal artery occlusion: local intra-arterial fibrinolysis versus conservative treatment, a multicenter randomized trial. Ophthalmology 2010;117(7):1367-75.e1. |

