Myopia is likely the most common condition encountered by optometrists in clinical practice, and the prevalence is only increasing.1 To make matters worse, myopia is also a well-established risk factor for serious eye diseases such as retinal detachment, glaucoma and maculopathy.2 Clinicians must prepare their practices to care for each and every patient diagnosed with myopia.3-5
A myopia management subspecialty within your practice is an opportunity to better educate your patients and families about the implications of progressive myopia, screen for at-risk patients and select the most appropriate treatments.
Here is a primer on how to put in place the systems required to successfully integrate myopia management into your practice.
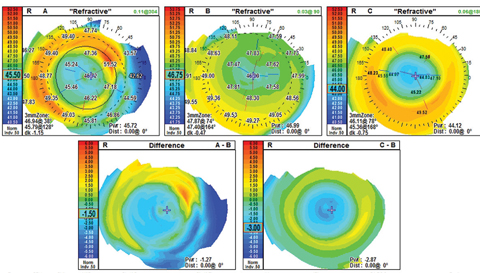  |
| Fig 1. The refractive difference map shows the similar corneal power profile for multifocal soft lenses and corneal reshaping. In map A, the patient is wearing NaturalVue multifocal 1-day -3.00. Map B is the naked cornea, and map C is the same patient after a night of corneal reshaping treatment. Click image to enlarge. |
Mind Shift
Clinicians ready to dive into myopia management as a subspecialty should start with the right mindset: focus on the condition you are treating, not the treatments you offer. For example, in our office, patients no longer make an appointment for a “corneal reshaping evaluation.” Instead, our staff schedules a “myopia management evaluation.” Likewise, we establish a comprehensive myopia management baseline before making treatment recommendations.
The more we learn about myopia and its implications, the more motivated we are to slow its progression. But when you have a child diagnosed with or at a high risk for myopia sitting in your exam chair, how do you proceed?
The answer depends on a number of factors—the most critical of which is how you frame the discussion. Our first recommendation is to stop referring to myopia as “nearsightedness.” This describes the subjective experience of blurred distance vision relative to near vision. Myopia is a condition that results in light being focused anterior to the macula, often due to excessive axial length.
Think of it this way: if a patient had LASIK for 7D of myopia and their post-surgical refraction was plano, are they still myopic? They may no longer be nearsighted, but when it comes to risk factors associated with axial length, they are still myopic. Society’s lexicon equating nearsightedness with myopia has led to a ho-hum attitude that only communicates blurred vision. In the exam room, we try to stick to the medical term myopia.
Myopia is more than an inconvenience of sight, and often patients and caregivers are more motivated to intervene when we take the time to explain myopia more completely. For one, an increase is most commonly due to an increase in axial length, which is the most likely cause of the increased risk of eye disease with higher myopia. Research estimates that if we successfully reduce progression by 33%, 73% of those children will be below 5.00D—a threshold associated with an increased risk of choroidal neovascularization, retinal detachment, glaucoma and cataract.6 Further reducing progression by 50% would mean 90% of those patients will remain below 5.00D.6
In our office, myopia education doesn’t start with the first “minus” refractive measurements. If a child has a high risk of myopia, including a positive family history and a documented reduction of hyperopia, then the conversation is started.
Table 1. Binocular and Accommodative Testing Performed in Myopia Management Assessment and Periodic After Care
|
Clinical First Steps
Clinicians can screen at-risk patients using a simple, single measure of refractive error. A child at six years of age with +0.75 or less of hyperopia has a significantly higher risk of developing myopia, and clinicians should recommend more frequent monitoring.7 Common recommendations for at-risk cases include increasing time outdoors and general visual hygiene such as monitoring working distance and taking breaks from accommodating at near for extended periods of time.8,9
Once a child is diagnosed with myopia and both the patient and parents understand myopia as a medical concern, our clinicians schedule a comprehensive myopia baseline evaluation. This includes measurements and procedures, beyond a routine eye exam, that reveal visual findings potentially contributing to myopia development and amenable to interventions (Table 1). The specialty evaluation guides the informed decision on which therapy is most appropriate and provides important data for comparison over time.
Binocular vision and accommodation are important to monitor in school-age children, as deficits can lead to difficulties with academic behaviors.10 The myopia management programs offered in our practice have the potential to impact binocular vision and accommodation, which necessitates a baseline that includes those measurements.
Practice pearl. This diagnostic battery is considered advanced testing, and the doctor should be compensated appropriately. In our practice, patients are financially responsible for the myopia management evaluation as a non-covered service billed outside of any managed care insurance program.
Table 2. Advanced Technology Used in Myopia Management
|
The Evaluation
The ocular health of our patient is our number one concern, and detailed corneal analysis is invaluable, especially for considering corneal reshaping and multifocal contact lens treatments. Clinicians should want the most comprehensive evaluation of ocular and visual findings that may impact myopia management now and into the future. That means clinicians should test beyond the standard evaluation of the cornea under the biomicroscope with fluorescein staining (Table 2).
In our practice, we gather information on endothelial cell function via specular microscopy and elevation data with corneal tomography, topography or both. Documenting pupil size in dim and bright lighting conditions is particularly important for treating with low-dose atropine. We perform infrared pupillometry, although less precise pupil size measurements are also useful.
Wavefront aberrometry, included in our baseline myopia management evaluation, documents any corneal higher-order aberrations (HOAs). Recent research suggests a correlation between HOAs and myopia progression, with larger HOAs associated with less myopia progression and smaller axial elongation.11 Comprehensive myopia management should include periodic axial length monitoring. If you are going to develop a myopia management subspecialty, axial length measurement is crucial and will likely be considered standard of care one day.
Practice pearl. In our practice, an ophthalmic technician gathers many of the measurements while the doctor discusses the pros, cons and efficacy of each treatment option to the parent. Common questions that come up include: How long will my child be treated? Is technology influencing myopia? What would you do?
A practitioner developing a myopia management practice should be prepared to address these questions. Regarding the last question, we have found that the following answer is effective: “I treat every child that I see as if they were my own. I would not recommend anything for your child that I would not do for my own children.” Of course, clinicians must truly believe it before using that statement.
Another important consideration is to include the child in the conversation once they are back in the exam room. It makes little difference if you and the parent are on the same page if the child isn’t. Ensuring the child understands the discussion will help improve compliance rates.
BHVI ResourcesBy Monica Jong, PhD, BOptom Clinicians can access many helpful myopia management tools provided by the Brien Holden Vision Institute (BHVI), including: Managing Myopia (North America). This COPE-approved course aims to help practitioners deliver the broadest and most effective management options and offers an opportunity to engage with leaders in the field during a live webinar. The course will be available March 21 through April 11, 2018, and can be found at https://academy.brienholdenvision.org/browse/usa/courses/myopia-us-2018. An evidence-based myopia calculator. This can help practitioners demonstrate the impact of various myopia management strategies on the predicted level of myopia up to the age of 17. Practitioners can access the calculator at https://calculator.brienholdenvision.org. The International Myopia Institute. This global group of experts is tasked with generating a consensus on key areas of myopia that can help guide practitioners towards an evidence-based approach to myopia management. Membership is free and open to all. The white papers will be freely accessible in late 2018. For more information, visit www.myopiainstitute.org. Dr. Jong is a senior research fellow at the Brien Holden Vision Institute. |
Choosing the Right Therapy
Research suggests slowing myopia progression is accomplished via two mechanisms of action: optical defocus and biochemical influence. Our practice has three evidence-based myopia management programs, two based on optical defocus and one on biochemical influence: corneal reshaping, soft multifocal contact lenses and low-dose atropine.
Other options may help to reduce myopic progression, but the evidence is not as compelling as it is for these three strategies. Although at times we still use other methods of myopia intervention, the formalized programs are limited to these three. Of course, all of these options are technically off-label uses, as none of them are FDA approved specifically for myopia control.
While the three options are presented, the majority of our patients still choose corneal reshaping as the primary treatment option. At our practice, approximately 80% of new myopia patients are fit in corneal reshaping lenses, 15% are fit in multifocal contact lenses and 5% are prescribed low-dose atropine. Corneal reshaping is our primary treatment option because our practice is involved in clinical research, and our doctors have a high comfort level with its safety and efficacy.12
Given the two mechanisms of action at play, it would seem logical that the combination would lead to an increased treatment effect. While our clinical experience suggests this is true, research has yet to provide evidence-based support for this modality. Thus, we reserve combination treatments for children with significant myopia progression.
 |
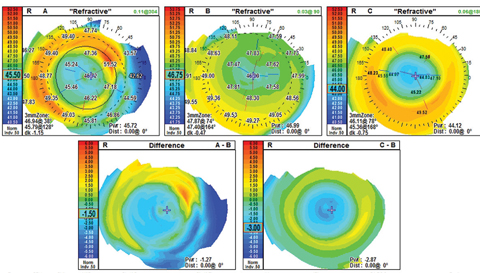
| Fig. 2. Measurements taken during a corneal reshaping patient’s first morning show a central island, indicated by the small zone of central corneal steepening. Click image to enlarge. |
Corneal reshaping. Research suggests this treatment option slows myopia progression, on average, by 45% with the added lifestyle benefit of not needing optical compensation during the day.13 However, proceed with caution with children who are outside of the FDA-approved parameters. For reference, the Paragon CRT system is FDA-approved for up to -6.00D of myopia and -1.75D of astigmatism. In our practice, if a patient is beyond that refraction, they are not candidates for the corneal reshaping program. Despite the excellent safety profile of corneal reshaping lenses, some parents are not comfortable with the concept of overnight contact lens wear.14 These patients may do better with one of the other treatment programs.
Multifocal contact lenses. This treatment option slows progression of myopia by approximately 50% and is a good option for patients who are averse to or have dropped out of corneal reshaping treatment or who are outside of the FDA-approved range for corneal reshaping.15,16 When fitting children in soft contact lenses, we are most comfortable with the single-use lens modality. Center-distance designs are our first choice, considering the optical effect is closest to mimicking the optics of a post corneal reshaping cornea (Figure 1).
Currently, only one single-use lens on the market in the United States has a center-distance design, the NaturalVue Multifocal 1-Day (Visioneering Technologies). It has a high plus effect that creates myopic defocus in the peripheral retina. Research shows myopic defocus in the peripheral retina can be a powerful stimulus to slow myopic progression and is the leading theory on the effectiveness of corneal reshaping and multifocal contact lenses.17
Low-dose atropine. This treatment program can reduce progression by approximately 50%. However, studies show it slows myopia progression after two years of treatment, one year off treatment, then two years on or off treatment, depending on progression—making generalization challenging.18,19
Regardless, treatment effectiveness is not the only factor under consideration when making myopia management recommendations. Patient and parent philosophies are also taken into account, and patients and their parents may prefer to avoid long-term medication use. While atropine has been a popular myopia control method for years, optometrists are often hesitant to recommend it due to concerns about side effects.19 The current literature, with the longest follow up of five years, reports no long-term side effects on accommodation or retinal function associated with the use of atropine.20,21 Clinically, we have yet to see a case with any significant complication due to therapy with low-dose atropine. A small percentage of cases experience mydriasis and reduced accommodative amplitude, both of which are addressed by either a further reduction in the atropine concentration or discontinuation of atropine therapy. Low-dose atropine may be a useful option for cases that are outside of the FDA-approved parameters for corneal reshaping, for those who are not appropriate multifocal contact lens candidates and in combination therapy. A thorough discussion of the benefits and risks of low-dose atropine can help patients and parents develop a comfort level with this option. In all studies to date, an inverse relationship of atropine concentration and myopia progression exists, where higher concentrations result in less myopia progression. Prior to the ATOM 2 study, the philosophy was to prescribe the highest dosage that did not result in symptomatic side effects. However, since the ATOM 2 study, we start at 0.01% atropine and consider increasing the concentration if there is evidence of inadequate myopia control.20
Marketing Your ProgramsOur practice has established a packet of information for each of our myopia management programs. The packet is organized in a branded, double-sided folder with information for the patient on one side and the treatment program contract on the other. The contract includes:
Our program fees are all-inclusive for the first year of treatment, and we do not separate professional services from materials. The exception is the low-dose atropine program, where the fee for the medication is handled by the patient and the compounding pharmacy and is not included in our program fee.
The fees for our programs are tiered and are based on several factors beyond a traditional refractive cutoff, including the estimated time investment for each patient, degree of myopia, rate of progression, patient age, complexity of the fit (for corneal reshaping and multifocal contact lenses), anticipated material costs and personality of the patient and parent. The more time we anticipate spending and the more challenging the case, the higher the quoted tier. When patients return for their second year in the program, they are responsible for another fee that covers a second comprehensive myopia evaluation. They can also enroll in an aftercare program the same day as their annual comprehensive eye examination. The aftercare program covers office visits related to myopia management for the year. If they do not enroll in the program, they must pay individually for each myopia management visit the following year. |
Ongoing Care
The follow-up schedule is similar across all modalities with the exception of corneal reshaping patients, who require a first morning follow up. The programs include visit intervals at one week, one month, three months and then every six months. More frequent visits are included in the cost of the program. Clinicians should evaluate eye health and side effects at every office visit and repeat refractive and axial length measurements at six-month intervals.
A few clinical pearls on corneal reshaping are important to share. For one, clinicians should not rush to modify the fit of a corneal reshaping lens after the first morning. Often, small concerns will disappear at the one-week visit without any modifications (Figures 2 and 3). In addition, clinicians should avoid taking visual acuities monocularly in free space. While perhaps an unusual clinical pearl, you will encounter parents who are not satisfied with one eye that is 20/20 while the other eye is 20/20-1. Taking binocular visual acuities in free space can eliminate any angst associated with slight variations. You can record monocular acuities, but with the patient behind the phoropter with no lenses before commencing refraction.
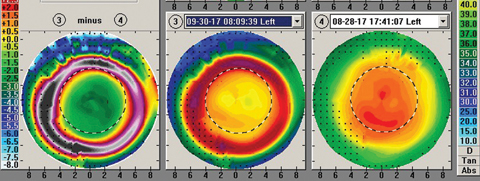 |
| Fig. 3. The same patient’s one week follow up shows complete resolution of the central island—without any changes to the prescribed lens. Click image to enlarge. |
Measuring Success
Since the area of myopia management is still in its relative infancy, clinicians will have to look to the literature to help define acceptable myopia control as more information is published. In our practice, we refer to experts in the field who reference control groups with average axial length elongations of 0.22mm to 0.24mm. Thus, we use greater than 0.23mm of axial elongation in one year as our benchmark for inadequate control for patients enrolled in one of our management programs. In those cases, we consider combined myopia management options. Unfortunately, there are times when, despite our best efforts, we are not achieving what we consider to be acceptable myopia control.
Adding formal myopia management programs has given us the opportunity to provide our patients with another area of specialized care that they have come to expect from our practice. A mother with three children undergoing myopia management in our practice recently shared, “I cannot adequately express in words what these treatment options mean for our family. Thank you.” With the right tools, you too can make a lasting impact on your myopic patients and their families.
Dr. Press is the director of Pediatric Eye Care, Binocular Vision and Vision Therapy Services at North Suburban Vision Consultants in Illinois.
Dr. Eiden is the president and medical director of North Suburban Vision Consultants and the president and cofounder of the International Keratoconus Academy.
1. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. |

