LASIK offers rapid visual recovery, safety, adjustability and stability, and it can be an economical alternative to glasses or contact lenses. Thanks to excellent results, advanced surgical techniques and the evolution of new equipment, LASIK has become the most popular surgical technique for the correction of refractive errors.1-3

While the postoperative visual acuity results in most LASIK cases are excellent, some patients do need additional surgery to achieve their best results. The most common type of surgery for additional laser treatment of residual refractive error is frequently called enhancement or re-treatment surgery.
When you refer for enhancement depends mainly on the patients recovery from the primary procedure. You must consider several clinical issues, particularly the amount of stromal tissue that was ablated in the primary procedure. The higher the attempted correction iswhether myopia, hyperopia or astigmatismthe more corneal tissue ablated, and the longer visual and corneal recovery.2,4

Right: The surgeon positions a blunt instrument to mark the edge of the flap.
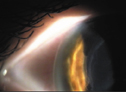
Left: Monitor the rough epithelium for ingrowth after flap lift.
Regression Rates
The highest regression rate occurs between the initial correction and eight weeks post-op. The higher the refractive error, the greater the regression effect.1,4 Over the next 6-12 months, the regression slows. Some patients, especially those with higher refractive errors, will take up to a year before their vision stabilizes. We dont know the exact mechanism. It may be due to postoperative epithelial hyperplasia or changes in keratocyte density.1,5
Additional ocular and medical factors that may affect the stability of the post-op refractive error are history of previous corneal surgery, dry eye syndrome, epithelial and endothelial integrity, age, fluctuating estrogen levels (in pregnant or nursing mothers), collagen vascular disease, smoking and diabetes. All can delay or alter the healing after LASIK.
Enhancement surgery for residual refractive error has a lower surgical risk and greater predictability than the initial LASIK procedure.6 The general technique for re-treatment involves lifting the original flap or making a new flap with a second pass of the microkeratome, and then performing laser surgery. A recent study by Y. Domniz, M.D., found both techniques to be safe, effective and highly predictable.1
However, Dr. Domniz also found that major flap complications are more likely to occur when recutting the flap because the corneal contour is flatter following the original myopic LASIK procedure.1 This change in corneal contour increases the risk of free, perforated or thin flaps.1,6 Additionally, a second cut can also result in a free lamellar wedge of stromal tissue where the second flap intersects with the original LASIK interface.6 The instrumentation and techniques involved with lifting the flap have improved so that its now possible to lift the flap in most cases, even years after the initial surgery.
Corneal Thickness
Whichever re-treatment technique is indicated, most U.S. surgeons believe its important to leave at least 250 microns of posterior stromal or bed tissue to decrease the risk of corneal ectasia.1 Many surgeons in Canada, however, consider it safe to leave 200 microns because corneal ectasia is so rare (although theres no guarantee that a patient wont develop corneal ectasia with a 300-micron bed).
Ectasia after LASIK can produce a cornea that appears as though it has keratoconus a serious but rare complication. Reducing the risk of corneal ectasia post-op demands prudent patient selection, accurate pachymetry and a stromal bed of no less than 250 microns.1
The average normal corneal thickness is 540-700 microns, from center to periphery, with the greatest thickness nasally and superiorly.6 The typical LASIK procedure creates a flap of 160 microns, leaving about 380 microns in the bed. The average amount of ablation removes about 12 microns per diopter. Thus, the maximum myopic ablation that can be performed on a patient with 540 microns of cornea and still maintain the 250-micron bed is about 11.00D.
These pachymetry calculations are important for planning surgical strategy and counseling the patient during the pre-op evaluation. If the patients corneas are too thin, then alternative procedures such as PRK or LASEK (laser epithelial keratomileusis) may be indicated. (For a more in-depth discussion on LASEK, please see Refractive Surgery Update, December 2001, LASEK: Its Like LASIK, Only with an E.) Like PRK, LASEK allows the surgeon to treat up to 15.00D or more in an average cornea. As with PRK, however, patients with higher corrections are prone to regression and post-op corneal haze.
During LASIK on higher myopes, routine intraoperative pachymetry readings help calculate actual flap thickness and residual bed thickness after the ablation. These readings are key when considering enhancement treatments.
Re-treatment Evaluation Protocols for LASIK Re-treatment
A patient youre considering for LASIK enhancement surgery should have serial office visits at which you monitor routine, postoperative healing, and fluctuations in visual acuity and residual refractive error; assess the cornea; and perform topographic analysis. Corneal evaluation includes flap-edge alignment, edema assessment and lamellar interface monitoring. Routinely, every patient needs at least one cycloplegic examination prior to enhancement surgery as well as documentation that the ocular health (IOP, peripheral retinal exam, etc.) is stable.
Todays patients have high demands. They want rapid results, so theyll push for enhancement surgery as early as possible. Pre-op education is critical.When counseling the patient at the initial pre-op evaluation, discuss timing and visual acuity factors for enhancementsespecially for the higher myopes and hyperopes (see table).
Guidelines based on two years of retrospective clinical observations over 15,000 managed patients who had LASIK on the Nidek EC 5000.
Type of LASIK Patient Minimum
Waiting Period For Re-treatment
Hyperope
6 months
Myope >-6.00D spherical equivalent
6 months
Myope <-6.00D spherical equivalent
3 months
Astigmat >-2.75d
6 months
PRK/LASEK
6 months
Previous RK
1 year
Corneal bed thickness <250 microns
contraindicated
A patient is ready for surgery when there is no more than 0.25D to 0.50D of fluctuation in refractive status for two months post-op. To evaluate corneal thickness, review the pre-op pachymetry, the lasers operative report and the actual post-LASIK results. For example the ablation on a -5.00D myope is approximately 60 microns, based on a 5.5mm optical zone with a transition to 7mm. So, if the virgin corneal thickness was 550 microns, you would expect clinically that it would be 490 microns post-LASIK. Variations often occur with this calculation due to the dynamic nature of the cornea, perhaps because of residual stromal edema or epithelial hyperplasia. Further research will help determine why the calculated and actual post-op corneal thickness measurements vary.
Because of the variations in LASIK healing, under-corrections and over-corrections are common. These residual refractive errors are usually minor and easy to manage with occasional-use spectacles. On many pre-op consent forms, patients must write that they realize they may need glasses after LASIK for clear vision.
Most eyes that have LASIK re-treatment achieve excellent visual acuity and good stability. LASIK re-treatment allows you to further improve upon outcomes in a safe and effective manner. Timing of post-LASIK stability and corneal thickness calculations are paramount for excellent results.
Dr. Augustine is national director of optometric clinical services for Clear Choice Laser Eye Centers, Brecksville, Ohio, and president of the Optometric Refractive Surgery Society.
1. Domniz Y, Comaish I, Lawless M, et al. Recutting the cornea versus lifting the flap: Comparison of two enhancement techniques following laser in situ keratomileusis. J Refract Surgery 2001;17:505-510.
2. Guell JL, Muller A. Laser in situ keratomileusis (LASIK) for myopia from -7 to -18 diopters. J Refract Surg 1996;12:222-228.
3. Perez-Santonja JJ, Bellot J, Claramonte P, et al. Laser in situ keratomileusis to correct high myopia. J Cataract Refract Surg 1997;15:150-153.
4. Helmy SA, Salah A, Badawy TT, Sidky AN. Photorefractive keratectomy and laser in situ keratomileusis for myopia between 6.00 and 10.00 diopters. J Refract Surg 1996;12:417-421.
5. Lohmann C, Guell JL. Regression after LASIK for the treatment of myopia: the role of the epithelium. Sem Ophthalmol 1998:13;79-82.
6. Probst LE, Machat JJ. Enhancement techniques and results. In: Machet JJ, Slade SG, Probst LE, eds. The Art of LASIK, 2nd ed. Thorofare, N.J.: Slack Inc. 1999;225-238.

