 |
One unique thing about an ocular examination is its ability to elucidate features of underlying systemic health. As such, laboratory testing is commonly used to confirm or augment clinical findings. A frequently ordered set of laboratory tests are the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). To best optimize the use of these tests in clinical practice, it is important to understand how and why they are measured as well as the significance of their values.
Both the ESR and CRP are basic blood tests used to assess the presence of inflammation in the body. However, they have low specificity, making it somewhat difficult to effectively employ in the diagnosis of a specific disease. Though they are both general markers for inflammation, their mechanisms are different, allowing for some interpretation in their respective values, both separately and together.1,2
ESR
The principle of this lab test depends primarily on the properties of red blood cells. Also known as erythrocytes, they typically possess a negative charge and repel each other, keeping them suspended in blood. In the case of inflammation or injury, the liver produces increased levels of proteins such as fibrinogen and immunoglobulins. These proteins are positively charged and act as bridges between erythrocytes, causing them to clump them together. This leads to red blood cells becoming heavier and settling more quickly at the bottom of a test tube.
The rate of sedimentation of red blood cells over time, usually over 60 minutes, is the basis of the ESR test, measured in millimeters per hour (mm/hr).1,2 Elevations in fibrinogen levels are not limited to inflammatory diseases alone, but also exist in conditions such as systemic infection, malignancy, diabetes or collagen vascular disease—all of in which inflammation is a byproduct.3
A unique distinguishing feature of the aforementioned plasma proteins is that many possess a long half-life and subsequently longer, amplified response time. As a result, ESR values will often have a slow initial rise, then slowly normalize, when compared with other acute phase proteins. This also allows for its use not only in the diagnosis of underlying inflammatory conditions, but also in monitoring disease activity.2,4,5
ESR values naturally increase with age as well as in pregnant patients.6,7 Due to these typical fluctuations of erythrocytes, the general calculation to determine the normal or reference range involves dividing the age—in number of years—by two for men, and the age plus 10 divided by two for women. Other factors contributing to abnormal ESR values include conditions that impact the quality and quantity of red blood cells in general, such as anemia, polycythemia and other erythrocyte hemoglobinopathies.3
CRP
This blood test is another way to measure inflammation in the body. Much like the basis of ESR, this measurement relies on release of CRP by the liver in response to inflammation caused by infection, tissue injury or autoimmune diseases.8
CRP is a pattern-recognition protein that is part of the acute phase of the innate immune response. It is produced in the liver in inflammatory conditions to assist in cellular processes such as complement binding and phagocytosis, and potentially in the clearance of apoptotic cells. In contrast to ESR, CRP levels typically rise within a few hours of inflammation and decrease as the body heals.9 Additionally, the CRP level is proportional to the intensity of inflammation.3
There are two main types of CRP measurements. The first is standard, measuring the overall level of CRP in the blood. There is an additional high-sensitivity CRP that detects even minor CRP elevations, making it particularly useful for assessing cardiovascular disease risk.10
CRP levels are typically reported in milligrams per liter (mg/L) and can vary slightly depending on the lab with regards to the normal or reference range. Generally speaking, low CRP is classified to be below 10mg/L and is suggestive of minimal inflammation. Moderately elevated CRP is approximately 10mg/L to 20mg/L, indicating possible infection or inflammation, while highly elevated levels are usually above 20mg/L, suggestive of significant inflammation.11
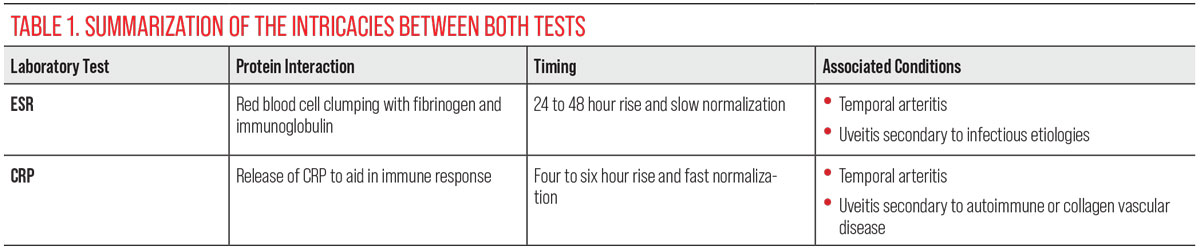 |
| Click image to enlarge. |
Ocular Connection
Both ESR and CRP provide similar information, are relatively inexpensive, readily available and have low specificity. However, using both tests in tandem can offer the most clinical utility in diagnoses and monitoring of inflammatory disease processes. As previously mentioned, these two tests differ in peak measurement. CRP is initially elevated and serves as an acute marker for disease, typically within four to six hours; ESR often peaks later on, around 24 to 48 hours. CRP will also normalize much quicker with treatment, whereas the ESR levels can take weeks, allowing for better long-term disease monitoring.3
There are many ocular diseases in which inflammation is a key factor, potentially leading to abnormalities in these ancillary tests. The two most common and relevant clinical scenarios are temporal arteritis and uveitis. Elevations in ESR and CRP levels, for example, are often diagnostic for temporal arteritis or polymyalgia rheumatica in conjunction with the clinical picture.12
 |
|
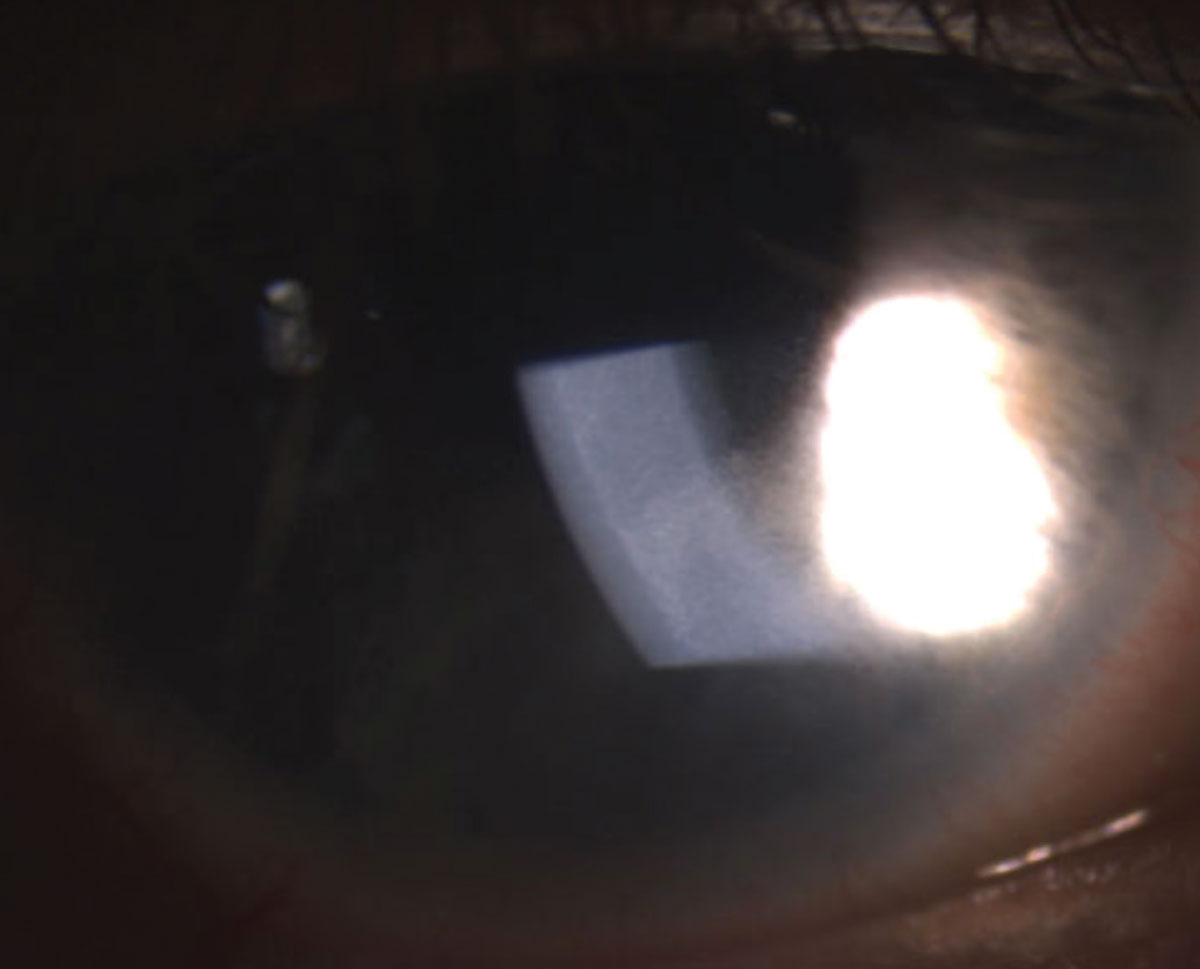
Uveitis, pictured here, is one ocular condition with marked inflammation, which would be indicated upon ESR or CRP testing. Photo: Kyle D. Dohm, OD. Click image to enlarge. |
Uveitis is a manifestation of numerous underlying systemic conditions, many of which would result in elevated ESR and/or CRP values. While uveitis in and of itself is inflammation, regardless of cause, studies have shown that first attacks of uveitis do not often lead to abnormal laboratory values. However, elevated levels of ESR and CRP suggest a systemic process causing uveitis. Further investigation has also attributed elevations in ESR to be due to autoimmune or collagen vascular disease etiologies, whereas abnormal CRP was more associated with trauma and infectious causes.3,13
When taken together, both ESR and CRP laboratory tests can be helpful in the clinical setting. Understanding the nuances of each test and why they are measured will give the clinician the highest yield in the diagnosis and monitoring of diseases with inflammatory components.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Lee, GR. Erythrocyte sedimentation rate. Korean J Lab Med. 2011;31(6):438-46. 2. Sed rate (erythrocyte sedimentation rate). Mayo Clinic. www.mayoclinic.org/tests-procedures/sed-rate/about/pac-20384797. September 21, 2023. Accessed March 20, 2024. 3. Bray C, Bell LN, Liang H, et al. Erythrocyte sedimentation rate and C-reactive protein measurements and their relevance in clinical medicine. WMJ. 2016;115(6):317-21. 4. Erythrocyte sedimentation rate (ESR). National Library of Medicine. medlineplus.gov/lab-tests/erythrocyte-sedimentation-rate-esr. Last updated November 8, 2022. Accessed March 20, 2024. 5. Mittal S, Gupta N, Awasthi S. Erythrocyte sedimentation rate in normal pregnancy. J Clin Diagn Res. 2014;8(8):CL01-03. 6. McPherson RA, Pincus MR. Henry’s clinical diagnosis and management by laboratory methods. 23rd edition. Elsevier Inc.; 2017. 7. Singh G, Bombardier C, Clégg LA, et al. Defining clinically important improvement in rheumatoid arthritis. Arthritis Rheum. 2000;43(2):343-51. 8. Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111(12):1805-12. 9. Ridker PM. C-reactive protein: a simple test to identify a greater risk of future cardiovascular disease. J Clin Invest. 2003;111(6):977-83. 10. Pearson TA, Mensah GA, Alexander RW, et al. American Heart Association C-Reactive Protein Writing Group. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107(3):499-511. 11. C-reactive protein test. Mayo Clinic. www.mayoclinic.org/tests-procedures/c-reactive-protein-test/about/pac-20385228. December 22, 2022. Accessed March 20, 2024. 12. Chan FLY, Lester S, Whittle SL, Hill CL. The utility of ESR, CRP and platelets in the diagnosis of GCA. BMC Rheumatol. 2019;10(3):14. 13. Groen-Hakan F, Eurelings L, van Laar J, Rothova A. Relevance of erythrocyte sedimentation rate and C-reactive protein in patients with active uveitis. Graefes Arch Clin Exp Ophthalmol. 2019;257(1):175-80. |

