 |
For patients older than seven, we can usually start to incorporate subjective data they provide us into our examinations rather than relying exclusively on objective data. The same, unfortunately, isn’t usually true for younger children. This column addresses how to approach refracting and prescribing in this population. Specifically, we will cover the protocols a focus group of optometrists—including us—who work with children helped develop for a handful of different ages. About 40 people came together in an effort to establish a shared evidence base that would act as a foundation for the emergence of clinical guidelines for the visual care of young children.
Don’t Get Ahead of Yourself
The group consisted of optometrists who were mostly from the United States, but some came from the United Kingdom, Denmark and Norway. We shared a similar understanding of the process of emmetropization, how the optics of the eye develop in healthy children and how we prescribe today has an impact on the future. Emmetropization should be left to follow its natural progression, and our prescribing should help it along. We only need to prescribe to shift the visual system within an envelope of refractive tolerance, at which point emmetropization takes over from there.
We could not, however, come to the consensus that refractive status of the developing eye and visual system is plastic earlier on in life and the actions we take as optometrists can have large consequences over time. A retrospective study of a large patient population seen at SUNY over many years showed the following refractive trends in infants:1
- Less than +2.50D of hyperopia increases emmetropia
- Greater than +2.50D of hyperopia increases hyperopia until 3.5 years of age
- Greater than 3.00D of anisometropia increases the chances of still having anisometropia at age 10 to 90% and the chances of also developing amblyopia to 60%
Infants average almost 3.00D of cylinder at birth, which decreases to about 1.00D by 2.5 to five years of age. When we look at refraction as a whole, infants lose about one-third of their spherical equivalent and two-thirds of their astigmatism by two years of age. For most of this tuning to occur, though, we can’t over-prescribe.
Just because you measure it doesn’t mean you should prescribe it, especially in a younger child. Prescribing the full refraction earlier on often gets in the way of emmetropization and its active tuning process that helps the optics of the eye put clearer images on the retina.
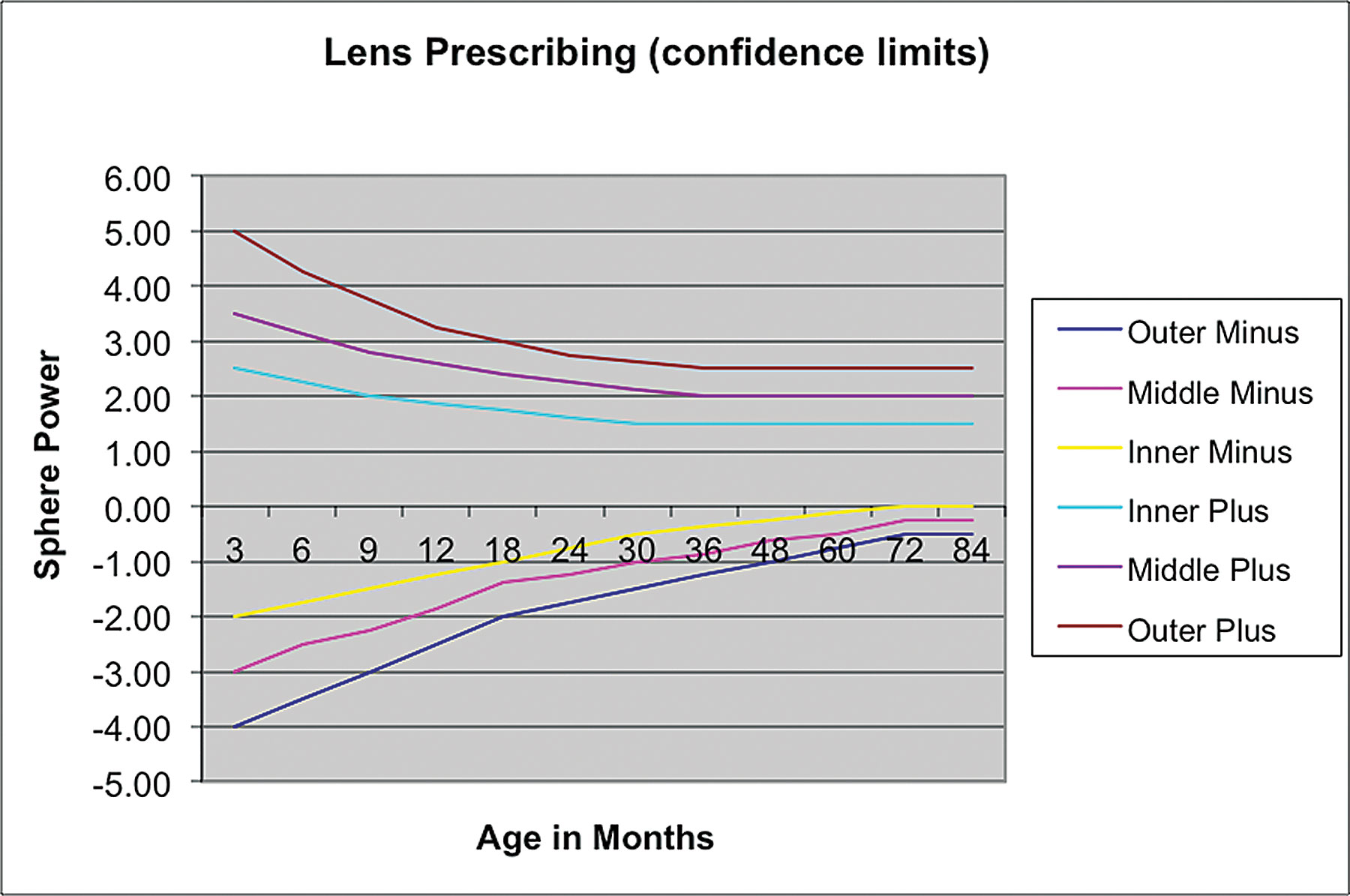 |
| A focus group of optometrists who work with children came up with these guidelines to follow when prescribing for younger patients. Click image to enlarge. |
The Break Down
As the graph illustrates, the inner two lines show measurement tolerances. If a child’s refraction at that age is inside the lines, we should not prescribe. For example, at three months of age it is advisable not to prescribe if the infant has a spherical power that falls within -1.75D to +2.50D. At 48 months of age, this range shrinks to between -0.25D and +1.50D.
The next most informative lines are the outer two. If a refraction falls outside of these lines, then action should be taken. For example, at three months of age, any hyperope in excess of +4.50D and any myope in excess of -3.50D should not be left alone. Some optometrists require the child to return for at least one additional visit at a different time of day, either with or without cycloplegia, before prescribing.
Between the inner and outer lines on either side of plano, we have a sort of sliding scale with “watch closely” toward the inner line to “take action” toward the outer. A child near the inner line might have to schedule a follow up appointment in four to five months, while a child near the outer line might have to be seen in two to four weeks. Generally, the younger the patient, the shorter the time between follow ups, and the older the patient, the longer the time between follow ups.
Once we decide to act, what actions should we take and to what extent should we react? If we are prescribing a patient’s first pair of glasses, it is advisable to shift the situation toward the inner line without fully correcting the refractive error.
For example, assuming both eyes are the same, let’s say we measure +5.00D in an 18-month-old whose eyes are straight and demonstrate good binocularity. Looking at the top portion of the graph, the outer line is at about +3.00D and the inner line is at +1.75D for an 18-month-old. The minimum lens we might give would have a spherical power of +2.00D, which would require the patient to have to supply +3.00D of accommodation to see clearly at distance. This is when the emmetropization process kicks in and helps reduce the hyperopia over time. The maximum lens needed to stabilize the system, leaving +1.75D uncorrected, would be +3.25D. At this level of correction, with little chance of emmetropization, we should expect the total amount of hyperopia to remain the same.
Thus, our range is from +2.00D to +3.25D, with the +2.00D activating the refractive tuning mechanisms maximally and the +3.25D simply stabilizing the system in place. Each case is different, but the lenses prescribed for this particular patient should live between these two values. Schedule a follow up sooner the closer to +2.00D you prescribe (three to four months) and further away the closer to +3.25D you prescribe (five to six months). The hope is that by focusing less on the hyperopia at first, emmetropization will partially correct it over time.
Pay attention to these general guidelines and refer back to our graph findings when seeing and prescribing in younger patients. For concrete, real-world cases that show our evidence-based clinical protocols in action, stay tuned for our next installment.
| 1. Sethee SK, FitzGerald DE, Krumholtz I. Exotropia in a pediatric population less than six years of age. J Behav Optom. 2003;14(6):149-57. |

