 |
As the scope of optometry broadens across the nation, more optometrists now have access to an expanding array of simple yet highly effective treatments that they can seamlessly integrate into their practice. ODs having the capability to practice to the full extent of their training can offer their patients the highest caliber of care. Optometric surgery consisting of minor surgical procedures such as eyelid cyst removals should be integrated into the practice of every medical optometrist practicing in states where scope has expanded to include these procedures.
Background
Encountered frequently on the eyelids, cystic growths can originate from various glands surrounding the ocular adnexa. These can include sebaceous glands, namely the glands of Zeis and meibomian glands.1 Cysts of Zeis are sebaceous cysts of the eyelid that present as solitary lesions found at the base of eyelashes near the eyelid margin. They are filled with yellow or turbid material and do not transilluminate. The most common type of sebaceous cyst of the eyelids affects the meibomian gland and is known as a chalazion.1
Cysts of the sweat glands of the eyelids can be categorized into two categories depending on the type of sweat gland it affects. The apocrine sweat glands of Moll open into the hair follicle, while the eccrine sweat glands open directly on the skin’s surface.1,2 These sweat gland cysts are collectively known as hidrocystomas. Apocrine hidrocystomas, also known as cysts of Moll, commonly manifest as sudoriferous cysts at the base of the eyelash or in the inner canthus as clear papules or nodules ranging from 1mm to 3mm in size. They may appear flesh-colored, blue or black and will transilluminate, while their size remains unaffected by temperature variations.1-4 Eccrine hidrocystomas typically present as clear cysts ranging from 4mm to 10mm in size and are located on the nasal or temporal side of the eyelid close to, but not on, the eyelid margin. These cysts exhibit transillumination and undergo size fluctuations in response to temperature shifts.1-4
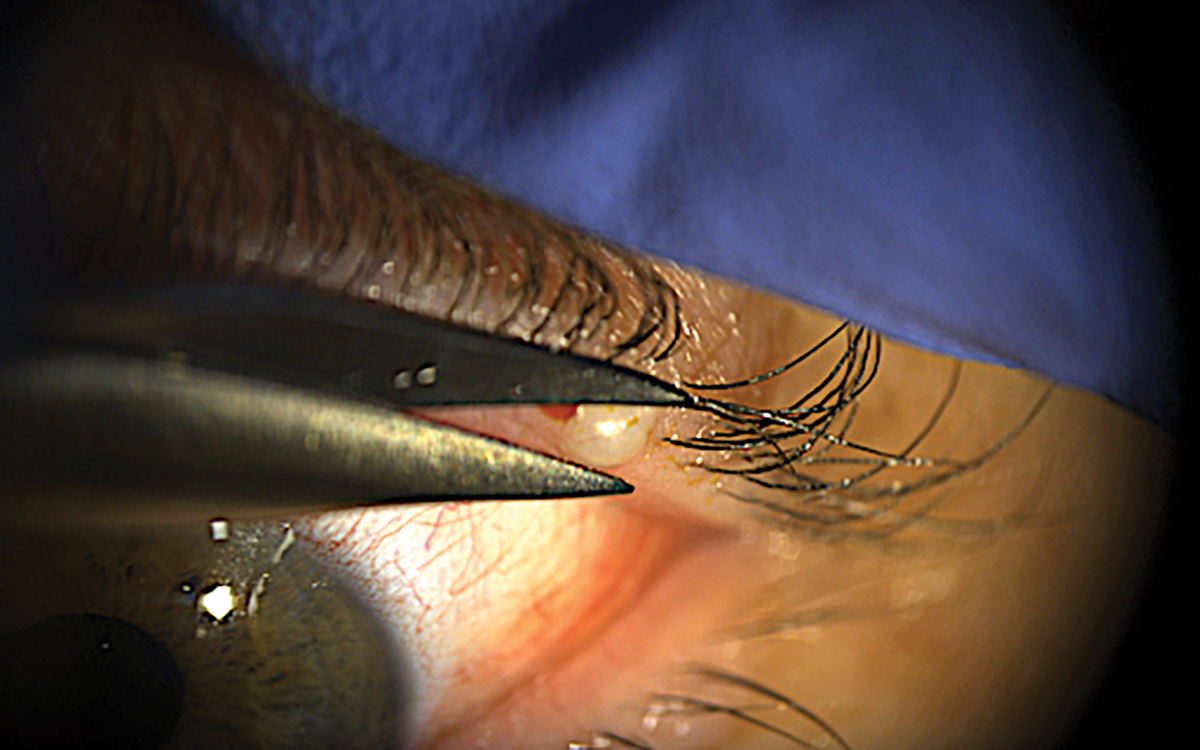 |
| A superficial eccrine cyst “unroofed” using Wescott surgical scissors. A characteristic clear blister bubble is present superficially. The patient stated it would grow in size with hotter temperatures. Topical anesthetic ointment was used rather than an injection of a localized anesthetic. Click image to enlarge. |
Cyst formation is caused from a blockage or obstruction in the duct, impeding the normal flow of sweat. Histologically, hidrocystomas present with a thin, non-keratinized epithelium lining and the cystic cavity holds clear or slightly turbid fluid. Surrounding the cyst wall are myoepithelial cells.3 Suspected to involve a chronic inflammatory process, various factors like genetics, sun exposure and age may contribute to their development. Additionally, epidermal inclusion cysts commonly develop on or around the eyelids, stemming from hair follicle obstruction or skin trauma, accumulating keratin, sebum and debris within a sac-like structure.1,5,6 While generally considered benign, the cysts described above can cause ocular discomfort and elicit cosmetic concerns for most patients.
 |
|
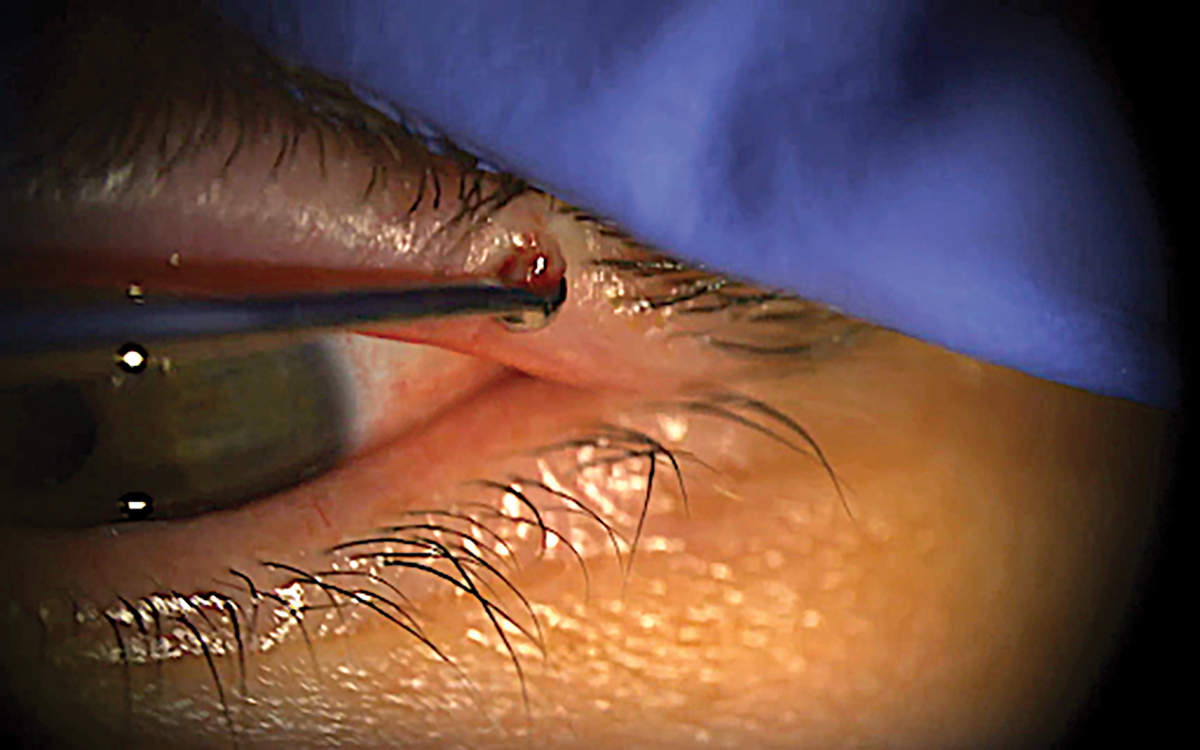
Using a foreign body curette can help excavate cystic capsules and contents. Click image to enlarge. |
Generally, a simple excision is the treatment of choice for these cystic eyelid lesions.1-6 Due to high rates of recurrence, complete removal of the capsule and contents needs to be achieved. The superficial nature of these growths still can warrant localized anesthesia as an incision or “unroofing” is performed followed by an excision of deeper tissue. Hemostasis is achieved with epinephrine and pressure; however, thermal cautery is usually warranted to achieve proper tissue destruction and hemostasis. Biopsies are recommended for atypical growths but cannot be achieved if a radiofrequency (RF) surgical unit is used in the excisional process, especially for small lesions. However, one may use an RF unit directly after a simple excision to “clean up” the operated area for improved cosmesis postoperatively.
Preoperative Procedures and Considerations
The equipment needed is readily available in most office settings. The simple excision procedure can be performed in an in-office setting where no surgical suite is necessarily needed. In a standard exam room, the patient can be supine in the chair is adequate. A surgical microscope is not needed, but loops are recommended to enhance precision. Alternatively, an RF unit can be used instead of the Westcott scissors and thermal cautery pen. Having a device that uses high-frequency electrical currents to cut, coagulate or ablate tissues, enables precise and controlled tissue removal while minimizing bleeding and promoting quicker healing.
 |
|
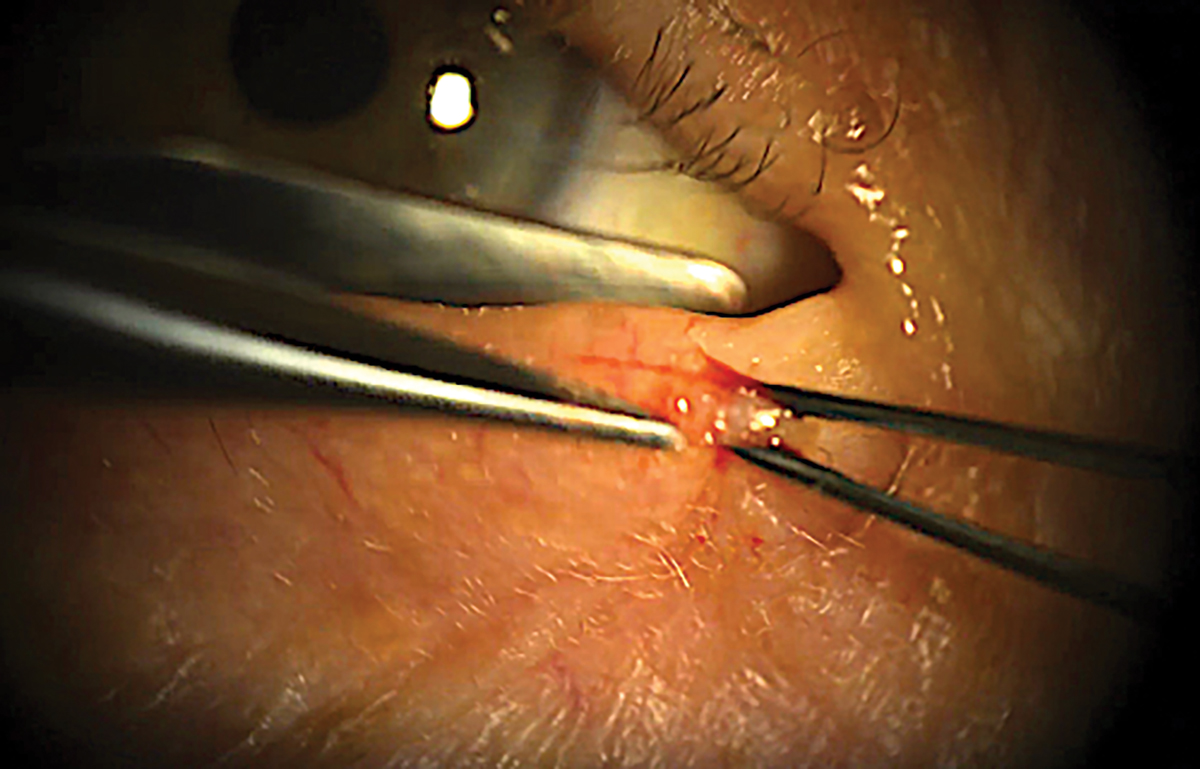
Handheld thermal cautery pen used for hemostasis. Note to not turn on the pen until the wires are on the targeted tissue. A quick touch usually gets the job done. Apply antibiotic ointment after. Click image to enlarge. |
When using an RF unit, it’s imperative to observe additional precautions, including keeping the target tissue wet with saline solution before ablation, avoiding use on patients with pacemakers or other electronic implanted devices and employing a smoke evacuator or vacuum system. Taking vitals, such as blood pressure and pulse rate, is recommended prior to performing any minor surgical procedures in the office. If a patient is on blood-thinning medications, it is not required to discontinue them prior to the procedure. Taking preoperative photos as well as obtaining proper informed consent are also part of the usual preoperative process.
Procedural Technique
To optimize patient comfort and procedural efficacy, the choice to administer localized anesthetic via intradermal injection hinges on factors such as lesion size, location and patient preference. Deeper cysts necessitating aggressive tissue manipulation and cautery will require the use of localized anesthetic. Conversely, superficial “bubble” cysts can be readily unroofed using surgical scissors post-topical anesthetic application with minimal discomfort.
Equipment Needs
|
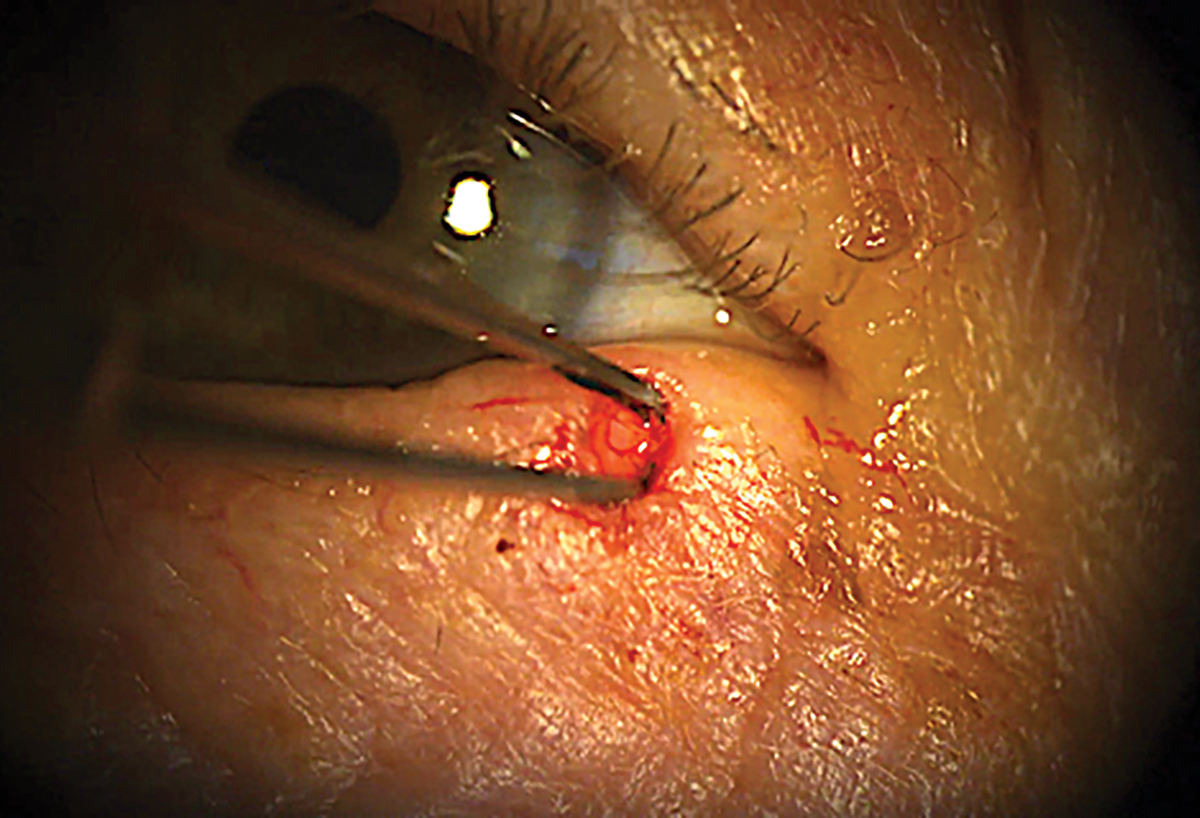
When local anesthesia is deemed necessary, it’s helpful to delineate the lesion’s borders using surgical markers before administering any injections. This process follows the sterilization of the operative lid with povidone-iodine or alcohol swabs. After the lid has been sterilized and the cystic borders marked, a 27- to 30-gauge needle attached to a syringe containing 0.5%, 1% or 2% lidocaine HCl with 1:100,000 epinephrine is carefully inserted into the subciliary skin adjacent to the cyst, with the bevel up angled at 10° to 15° degrees. Then, 0.3mL to 0.5mL of anesthetic is administered continuously as the needle is gradually withdrawn until a bolus of anesthetic is seen under and around the lesion, which is the injection endpoint. Pull the targeted lid taut with the free hand while using the other to inject the anesthetic. Prior to proceeding, test the anesthesia by palpating the target tissue with sterile forceps. Digital palpation over the injected area helps enhance anesthesia. Using toothed forceps to grip the apex of the cyst and pulling upward with one hand, Westcott surgical scissors are wielded in the dominant hand to “unroof” the lesion. Alternatively, RF could also be used with a “bent tip” electrode to make an incision into the cyst.
 |
|
Grabbing taut the apex of the cyst and pulling anteriorly while moving Westcott surgical scissors in position for initial “unroofing.” Click image to enlarge. |
Once the incision has been made, the forceps can then grab the contents of the cyst, ensuring the removal of the capsule and capsule wall entirely. Any excess cystic material is removed using a curette to minimize the chance of recurrence. The center of the cystic pocket is cauterized using a handheld thermal cautery pen (or alternatively RF).
Ensure that the cautery wires are on the tissue before activation to treat only the targeted tissue. Debris or blood is cleaned off using cotton-tipped applicators while applying slight pressure to the area to aid in hemostasis.
Finally, a single layer of topical ophthalmic antibiotic ointment is applied to the treated area. The ointment should have good gram-positive coverage, such as erythromycin 0.5% ophthalmic ointment.
 |
|
The cystic capsule is extracted using forceps with teeth to ensure the entire contents are removed to prevent recurrence. Click image to enlarge. |
Follow-Up
A topical antibiotic ointment with good gram-positive coverage is prescribed. Instruct the patient to apply a small layer to the treated area twice daily for one week. Educate them with post-op care instructions, including recommendations for managing any discomfort or swelling and instructions for proper wound care, as well as to contact the office readily if any issues are noted between visits. Recommended follow-up should typically be scheduled in two to four weeks for a recheck to ensure proper healing and to discuss pathology reports if a biopsy was obtained at the time of the excision. It is recommended to take photos of the lesion preoperatively and postoperatively for documentation purposes.
Takeaways
As medical optometrists incorporate eyelid cyst removal procedures into their practice, they will find that, with experience the process becomes increasingly manageable. Confidence grows with each successful removal performed, paving the way for more opportunities to provide patients with the highest level of medical eye care. By integrating eyelid cyst removals, medical optometrists can enhance their ability to treat a broader range of ocular diseases, ultimately bolstering the overall quality of care received by patients.
Dr. Daniel specializes in ocular disease and refractive surgery at Edmond Regional Eye Associates in Edmond, Oklahoma, having received advanced clinical training in the diagnosis and management of ocular disease. He is also certified in laser vision correction, anterior segment laser procedures and other minor surgical procedures. Dr. Daniel is a fellow of the American Academy of Optometry, as well as a diplomate of the American Board of Optometry. He has no financial disclosures.
Dr. Lighthizer is the associate dean, director of continuing education and chief of specialty care clinics at the NSU Oklahoma College of Optometry. He is a founding member and immediate past president of the Intrepid Eye Society. Dr. Lighthizer’s full disclosure list can be found here.
1. Stokkermans TJ, Prendes M. Benign Eyelid Lesions. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK582155. Last updated May 29, 2023. Accessed March 19, 2024. 2. Couto Júnior Ade S, Batista GM, et al. Hidrocystoma: surgical management of cystic lesions of the eyelid. An Bras Dermatol. 2010;85(3):368-71. English, Portuguese. 3. Penne R. Oculoplastics. 2nd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins Health; 2012. 4. Yanoff M, Duker J. Ophthalmology. 4th ed. Philadelphia: Elsevier Saunders; 2014. 5. Cape HT, Mukit FA, Mukit M, et al. Apocrine hidrocystoma of the upper eyelid. Eplasty. 2022;22:ic13. 6. Trischman T, Scott JF. Comparative Efficacy of hidrocystoma treatments: a systematic review. J Cutan Med Surg. 2020;24(5):474-80. |

