 |
A 71-year-old Hispanic male presented for an evaluation of a cataract in his left eye. He had undergone cataract surgery in the right eye three years earlier with excellent visual results. However, over the past year he said he has noticed more difficulties seeing out of both eyes. He denies any flashes, floaters, double vision or ocular pain. His past medical history was significant for a recent diagnosis of prostate cancer. The prostate was removed three months prior without radiation. His most recent prostate specific antigen (PSA) test was 0ng/mL one month prior.
Evaluation
Upon examination, his uncorrected vision was 20/25 OD and 20/25 OS, which was correctable to 20/20 in both eyes. Confrontation visual fields were full to careful counting in both eyes. Pupils were equally round and reactive to light; no afferent pupillary defect was found. The intraocular pressure (IOP) was 14mm Hg in both eyes.
A slit lamp examination revealed mild meibomian gland dysfunction and posterior blepharitis in both eyes and a well centered PCIOL without PCO in the right eye. The left eye had a mild nuclear sclerotic cataract. Dilated fundus exam of the left eye was normal. The right eye revealed a 1.5DD elevated lesion (Figure 1). An OCT (Figure 2) and ultrasound imaging, including B-scan (Figure 3) and standardized A-scan (Figure 4), were also obtained.
Upon further questioning, he was not certain about his ocular history other than having cataracts. Given the history and suspicious appearance of the lesion, we referred him promptly to the ocular oncologist.
Take the Quiz
1. How would you describe characterize the A-scan findings?
a. Essentially normal.
b. Highly reflective.
c. High and low reflectivity.
d. Low to medium reflectivity.
2. What high-risk characteristic does the lesion in the fundus photo display?
a. Orange pigment.
b. Subretinal fluid.
c. Proximity to the fovea.
d. a and b only.
3. What is the most likely diagnosis?
a. Choroidal nevus.
b. Choroidal melanoma.
c. Choroidal hemangioma.
d. Choroidal metastasis.
4. Given the location of the lesion, how will this patient likely be managed?
a. Observation.
b. Enucleation.
c. Plaque therapy.
d. External beam radiation.
5. Which statement is accurate with regards to his diagnosis/prognosis, respectively?
a. Choroidal nevus; observation.
b. Small choroidal melanoma; plaque radiotherapy.
c. Medium choroidal melanoma; enucleation.
d. Large choroidal melanoma; transpupillary thermotherapy.
For answers, see below.
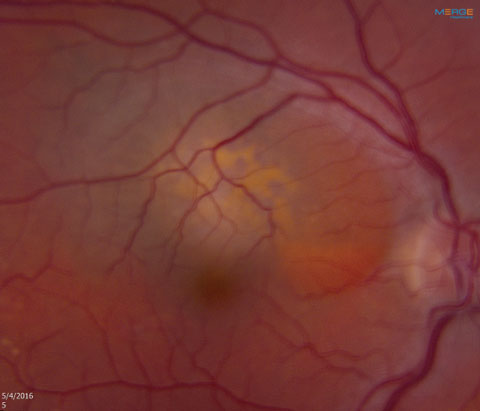 |
| Fig. 1. The patient’s left eye. Note the lesion superior to the macula. |
Diagnosis
Based on the clinical findings and imaging studies, the lesion most likely represents a small choroidal melanoma, although we were not 100% certain. Clearly, the patient displayed risk factors that make this lesion particularly worrisome, but because it is still quite small (5mm x 4mm x 1mm) and located near the fovea the ocular oncologist felt it was appropriate to observe it with close follow up to determine if it grows.
Discussion
Choroidal melanoma is the most common primary intraocular malignant tumor in adults, and the second most common site for malignant melanoma in the body.1 They can either arise de novo or from a preexisting choroidal nevus.2 Melanomas in the eye occur in the uveal tract, which includes the iris, ciliary body and choroid.3 Only four to six primary choroidal melanomas cases are reported per one million cases a year in the United States, totaling about 1,400 annual cases, with a slightly higher rate in Scandinavian countries.1,4,5,7 They are more common in middle-aged Caucasian men of Northern European descent with fair complexion and blue or green irises, typically with a mean age of 55 years.1,7 Hispanic and Asian patients have a small risk, while the incidence in black patients is extremely low.4 There is a possible association among arc welders, due to excessive UV light exposure, while an increased risk from a history of chronic sunlight exposure remains inconclusive.1,2,4
Patients with choroidal melanomas are typically asymptomatic, unless the tumor involves the macula, there is subretinal fluid, retinal detachment or even a vitreous hemorrhage. The most common symptoms include decreased visual acuity, as well as visual field deficits, flashes, floaters and, in rare cases, pain.2,7 When present, pain can come from inflammation, tumor necrosis, neovascular glaucoma, massive extraocular extension or impingement of the long posterior ciliary nerves.1,7 If large enough, the classic presentation of these lesions is a pigmented dome-shaped or collar button-shaped tumor with an associated exudative retinal detachment and orange pigment at the level of the RPE.1 Orange pigment, or lipofuscin, is composed of components from the incomplete metabolism of photoreceptor outer segments.7
 |
| Fig. 2. OCT slightly superior of the macula. |
Uveal melanomas can be quite variable in shape, size and presentation. They are typically elevated either like a mushroom or a dome but can be yellowish (amelanotic), dark-brown, green or grey in color.7 Commonly, subretinal fluid is present, and with the progressive breakdown of the retinal pigment epithelium (RPE), an exudative retinal detachment can occur.7 If the melanoma is large enough or involves the ciliary body, there can be the presence of prominent episcleral vessels, referred to as sentinel vessels.1
Treatment
The biggest challenge is trying to determine if a lesion is a suspicious nevus or a small choroidal melanoma, and the best way to differentiate between the two is to closely observe for growth over time. However, there are features that are more suggestive the lesion is a small melanoma such as orange pigment (lipofuscin), the presence of subretinal fluid, thickness greater than 2mm, largest base diameter greater than 7mm, visual symptoms, less than 3mm from the disc margin, ultrasound hollowness, and the absence of drusen and a halo.1,4,7 The presence of one of the above risk factors increases the chance of growth from 3% to 38% over the course of five years, while the presence of two or more risk factors increases the risk of growth to more than 50%.7 Along with low-medium internal reflectivity on the A-scan, our patient’s lesion also has lipofuscin and subretinal fluid, suggesting it is likely a small choroidal melanoma. Choroidal nevi on the other hand are usually less than 2mm thickness and less than 6mm in diameter.7 Drusen are often present in a suspicious nevus, indicating chronicity.
 |
| Fig. 3. Note the elevation in these B-scans of the lesion. |
 |
Besides recognizing the clinical features that suggest a choroidal melanoma, A-scan ultrasonography is perhaps the most sensitive and diagnostic test. Choroidal melanomas will show low-to-medium internal reflectivity while B-scans can show acoustically silent zones. The B-scan can also show a bright anterior aspect of the lesion, biconvexity, choroidal excavation and a solid mass shadowing of the orbit.1,7 Together, A- and B-scans have a more than 95% sensitivity in diagnosing choroidal melanomas.1 The value of the OCT is that it can show the presence of serous fluid as well as a choroidal lesion pushing up on the RPE.
The importance of determining if the lesion is malignant is to reduce the risk of metastasis and possible death. There is ongoing research exploring the molecular and genetic markers that can predict metastatic potential, and researchers believe that Monosomy 3 (loss of chromosome 3) is indicative of a more aggressive tumor.1,2,6,9 Once a lesion is determined to be choroidal melanoma, treatment is initiated based on upon COMS (The Collaborative Ocular Melanoma Study) protocol.
Tumor treatment usually depends on the size of the lesion. Small melanomas, which are typically 2mm to 3mm in thickness and 6mm to 7mm in basal diameter, can be observed until evidence of growth. Once a decision is made to treat small melanomas, I-125 plaque radiotherapy is commonly used. With plaque therapy, a radioactive plaque is sutured on the surface of the globe exterior to the tumor for three to seven days depending on tumor size, with provides excellent control in about 98% of patients.1,2,7 Other treatment options include external beam charged particle radiation, and transpupillary thermotherapy (TTT), among others.1,7 TTT is done with a low-power infrared laser for a long duration, which is effective for small tumors about 3DD away from the ONH or center of vision.2,7 It can be done in conjunction with plaque brachytherapy. Despite the diagnosis of a small choroidal melanoma, the estimated five-year mortality rate related to the tumor is only about 1% according to COMS.8
Medium size tumors, usually 3mm to 8mm thick and 7mm to 14mm in diameter, are usually treated with globe-sparing treatments such as I-125 (iodine) plaque brachytherapy, which showed about the same benefit in terms of mortality compared with enucleation.1,6 From the medium arm of the COMS trial, patients had a 90% five-year survival in both the enucleated group and the plaque brachytherapy group.8 Large tumors, which are greater than 8mm in thickness and greater than 14mm in diameter, are still generally enucleated although plaque therapy may be an option if a large enough plaque will fit over the tumor.8 Unfortunately, however, according to COMS, the tumor-related mortality rate of patients with large choroidal melanomas is over 25% within five years, while the all-cause mortality is upwards of about 40%.8
 |
| Fig. 4. What does this A-scan of the patient’s right eye reveal? |
Patients with uveal melanomas are always at risk for developing metastatic disease. In most of the studies, the larger the tumor, the greater the risk of metastasis.9 Fortunately, about 98% of patients do not have metastatic disease at the time of diagnosis, but if a metastasis occurs, it is most often within the first year of diagnosis, although it can metastasize even more than 10 years after treatment.4,7 Therefore, extensive testing is needed at the time of diagnosis such as CBC, liver enzymes, abdominal CT scan (or MRI or ultrasound) and a chest x-ray.7 If, however, a distant metastasis is found at the time of diagnosis, treatment of ocular melanomas is simply palliative; the patient needs systemic chemotherapy.1
Unfortunately, the most common site of metastasis is to the liver, which has an estimated survival rate of about six months, compared with 19 months to 28 months in extrahepatic metastases.1
The choroidal lesion in our patient was relatively small, measuring 1mm in thickness and 5mm x 4mm in diameter. The ultrasound showed medium reflectivity as well as orange pigment and subretinal fluid involving his macula, all suggesting the lesion is a small choroidal melanoma. Because it was small, the ocular oncologist elected to follow the patient to determine growth. The patient was asked to return in two months for revaluation.
Dr. Brafman is an optometric resident at the Bascom Palmer Eye Institute in Miami.
|
1. Singh P, Singh A. Choroidal melanoma. J. Ophthalmol. 2012 Jan-April;5(1):3-9. 2. Choroidal Melanoma. WillsEye Hospital. 2011 Oct 5. Available at www.willseye.org/health-library/choroidal-melanoma. 3. Finger P. Choroidal Melanoma. New York Eye Cancer Center. Available at https://eyecancer.com/eye-cancer/conditions/choroidal-tumors/choroidal-melanoma/. 4. Komatsu T, Sowa T, Takahashi K, Fujinaga T. A case of solitary pulmonary metastasis of choroidal melanoma with an exceptionally long disease-free period. International Journal of Surgery Case Reports. 2013;4(10):849-51. 5. Tran E, Ma R, Paton K, et al. Outcomes of proton radiation therapy for peripapillary choroidal melanoma at the BC cancer agency. International Journal of Radiation Oncology, Biology, Physics. 2012 Aug;83(5):1425-31. 6. Marathe O, Jeffrey W, Lee S, et al. International Journal of Radiation Oncology, Biology, Physics. 2011 Nov 15;81(4): 1046-8. 7. Weidmayer, S. Choroidal Melanoma is a Life Sentence. Rev Optom. 2012 Jan 15;149(1):48-55. 8. Margo C. The collaborative ocular melanoma study: an overview. Cancer Control. 2004 Sept-Oct;11(5): 304-9. 9. Finger P. Small Choroidal Melanoma: To Treat or Not To Treat, That is The Question! New York Eye Cancer Center. 1995. Available at https://eyecancer.com/eye-cancer/research-articles/small-choroidal-melanoma-to-treat-or-not-to-treat-that-is-the-question/. |

