 The topic of nutrition and the eye has garnered a lot of
attention during the last five to 10 years. Several groundbreaking studies,
including the Age-Related Eye Disease Study (AREDS) and the Lutein Antioxidant
Supplementation Trial (LAST), demonstrated mixed results and suggested that
certain supplements can effectively protect against many ocular diseases, while
other supplements offer no protection at all.
This paper provides an overview of specific micronutrients
and their role in the prevention and/or treatment of age-related macular
degeneration, cataract and glaucoma.
The topic of nutrition and the eye has garnered a lot of
attention during the last five to 10 years. Several groundbreaking studies,
including the Age-Related Eye Disease Study (AREDS) and the Lutein Antioxidant
Supplementation Trial (LAST), demonstrated mixed results and suggested that
certain supplements can effectively protect against many ocular diseases, while
other supplements offer no protection at all.
This paper provides an overview of specific micronutrients
and their role in the prevention and/or treatment of age-related macular
degeneration, cataract and glaucoma.
Macronutrients and Micronutrients
With instant access to Internet and other multimedia news sources, patients are becoming actively involved in seeking natural remedies for various health conditions. There is little doubt that your patients “are what they eat,” and eating nutritious foods facilitates both a healthy mind and body. But, what nutrients should your patients consume, how much of a given nutrient should they consume, and should those nutrients be consumed in the form of food or supplement? Because there are so many advertising campaigns on “proper nutrition,” it is no surprise that many patients are lost in a sea of alleged facts and figures.
Food provides the energy and nutrients needed for human growth and survival. Macronutrients (carbohydrates, proteins and fats) and micronutrients (vitamins and minerals) together contribute to the human body’s total energy pool. Frequently, your patients will meet daily macronutrient requirements, but fall well short of daily micronutrient requirements.1 This scenario is fairly problematic; adequate micronutrient intake is critical to overall systemic health and longevity. Additionally, excessive macronutrient intake can directly contribute to obesity and a host of potentially life-threatening conditions.
So, the question arises: Can a micronutrient pill or supplement in addition to adequate macronutrient intake help your patients meet their nutritional needs? The answer is more complicated than a simple “yes” or “no.” Theoretically, nutritional supplements can deliver an ideal level of micronutrients to the body. But, what about the benefits of “hidden nutrients” that researchers might have not yet identified contained within foods? All foods have their own unique composition and play a vital role in maintaining systemic health. But, the amount of macro- and micronutrients contained within any given food is of fundamental importance. As such, excessive intake of one particular nutrient could cause more detriment than benefit. For example, it would be completely negligent to suggest, “If a glass of wine a day is good, then an entire bottle should be even better.” The Institute of Medicine of the U.S. National Academy of Sciences established tolerable upper intake levels (UL) of many common micronutrients in 1997 because of the advent of nutrient-fortified foods and patients’ increasing intake levels of multivitamin supplements. (See “Recommended Dietary Allowances and Tolerable Upper Intake Levels of Commons Micronutrients.”)2
| Recommended Dietary Allowances and Tolerable Upper Intake
Levels of Common Micronutrients2
| |||
| Micronutrient*
|
Recommended daily dietary allowances for men (19 to 50
years of age)
|
Recommended daily dietary allowances for women (19 to 50
years of age)
|
Tolerable daily upper intake levels for all men and women
|
| Vitamin A
|
900mcg
|
700mcg
|
3000mcg
|
| Vitamin C
|
90mg
|
75mg
|
2000mg
|
| Vitamin D
|
5mcg
|
5mcg
|
50mg
|
| Vitamin E
|
15mcg
|
15mcg
|
1000mg |
| Vitamin B6
|
1.3mg
|
1.3mg
|
100mg |
| Niacin
|
16mg
|
14mg
|
35mg |
| Choline | 550mg
|
425mg
|
3.5g |
| Iron
|
8mg | 18mg
|
45mg |
| Selenium
|
55µg
|
55µg | 400µg |
| Zinc
|
11mg
|
8mg
|
40mg |
| * No tolerable upper intake level has been determined for vitamin K, thiamine, riboflavin, vitamin B12, pantothenic acid, biotin or the carotenoids. | |||
Nutrition and AMD
• Vitamin C. Humans do not have the ability to manufacture vitamin C naturally and depend on external sources to meet daily intake requirements.3 This antioxidant is proven to protect protein, lipids, carbohydrates and nucleic acid from free radical damage.3 Despite the popular conception that citrus fruits, such as oranges or grapefruits, are the best sources of vitamin C, yellow sweet peppers actually top the list.3 Additionally, Brussels sprouts, kiwis, strawberries, cantaloupes and papayas are good sources of vitamin C. Several recent studies, including AREDS, have suggested that vitamin C intake protects against retinal damage.4-6 AREDS participants were randomly assigned to an 80mg q.d. zinc group, an antioxidant combination group (500IU vitamin C, 400IU vitamin E and 15mg beta-carotene q.d.), an antioxidant combination plus zinc group or a placebo group, depending on the level of AMD severity. Participants with moderate AMD in the antioxidant combination plus zinc group were 25% less likely to experience AMD progression than participants in the placebo group.
|
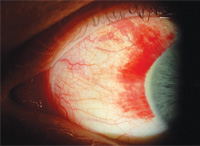
| Conjunctival hemorrhage in an otherwise healthy patient who
reported taking aspirin and a large quantity of caffeine for a headache. Such
isolated episodes do not require advanced testing; however, recurrent
conjunctival hemorrhage can be indicative of nutrient deficiency, including
lack of vitamin C.
|
• Carotenoids. Alpha- and beta-carotene are provitamin A carotenoids, which means that the body can convert them into vitamin A. Good sources of alpha- and beta-carotene include carrots, spinach and winter squash. Non-provitamin A carotenoids include lycopene, lutein and zeaxanthin. Lycopene is chiefly found in tomatoes and tomato products. Dark green vegetables, such as kale, spinach, collard and broccoli, are good sources of lutein and zeaxanthin, both of which are found in the retina. Lutein and zeaxanthin prevent a substantial amount of blue light from entering the eye, so they likely help prevent oxidative damage, which causes AMD.12 Researchers from the Carotenoids in Age-Related Eye Disease Study (CAREDS) concluded that diets rich in lutein and zeaxanthin may protect against AMD in healthy women younger than 75 years of age.13 The data suggested that consuming at least 6mg lutein and zeaxanthin q.d. from fruits and vegetables may decrease the risk of AMD by up to 57%.14,15
• Omega-3 fatty acids. Dietary intake of omega-3 fatty acids is essential because humans cannot synthesize it. Fish and fish oil are excellent sources of omega-3s. One very recent study proposed that consumption of fish and other foods rich in omega-3 fatty acids may be associated with a lower risk of AMD.16 However, its authors suggested that a lack of existing research and quality trials make it difficult to determine the amount of omega-3 fatty acid intake necessary to prevent AMD development.
 |
|
This patient presented with cortical, nuclear sclerotic and
posterior sub-capsular cataracts. Long-term use of multivitamins might protect
against both nuclear and cortical cataract development. |
Although cataract extraction is a relatively easy and safe procedure, delaying or preventing cataract development preserves patients’ visual function and quality of life. Ascorbate levels in the aqueous humor are higher than plasma levels, so certain micronutrients might protect the crystalline lens from oxidative damage—but, which ones? The answer is complicated because cataract formation is multifactorial.
The Nurses’ Health Study found that a high dietary intake of lutein and zeaxanthin yielded a 22% reduction in risk for cataract surgery.17,18 Additionally, this study suggested that participants who took vitamin C supplements for more than 10 years were 45% less likely to require cataract surgery than participants who received a placebo. Similarly, researchers from the Blue Mountains Eye Study found that long-term use of daily multivitamins protected against the development of nuclear and cortical cataracts.19
However, the Beaver Dam Eye Study found no relationship between the incidence of nuclear sclerotic cataract and increased dietary intake of vitamin C, vitamin E, alpha-carotene or beta-carotene, except when other risk factors (i.e., excessive smoking and systemic hypertension) were present.20 Nevertheless, the study did suggest that vitamin C reduced cataract formation in participants who smoked heavily or had elevated glycosylated hemoglobin levels.20 And more recently, AREDS showed that high doses of vitamin C, vitamin E and beta-carotene had no effect on incidence of either cataract development or extraction during an approximate six-year period.21 Clearly, many of these studies have yielded inconsistent results. The differences in patient outcomes could be due to inherent variations in study populations. Additional research and analysis likely is required to determine optimum nutritional intake levels.
Nutrition and Glaucoma
Despite demonstrating proper compliance with glaucoma medications, some patients might continue to experience progressive optic nerve damage. These patients are likely candidates for complementary and/or alternative medicine. Several herbal supplements are recommended for glaucoma patients, including Ginkgo biloba and bilberry as well as the highly controversial cannabinoids (tetrahydrocannabinol, cannabidiol and cannabinol).
• Ginkgo biloba. Ginkgo biloba has been reported to increase blood flow in the ophthalmic artery in healthy subjects.22 Interestingly, one study showed visual field improvement in patients with normal tension glaucoma who received 120mg/day of Ginko biloba for four weeks.23 However, this finding has yet to be confirmed by additional laboratory research.
• The cannabinoids. Several studies have shown that cannabinoids lower IOP by enhancing uveoscleral outflow.24-27 One study showed that a single sublingual dose of delta-9-tetrahydrocannabinol lowered IOP by an average of 3.8mm Hg after two hours vs. a placebo. However, the results demonstrated no statistically significant IOP reduction in participants who took either 20mg or 40mg of cannabidiol. In fact, participants who took 40mg of cannabidiol actually experienced an average transient increase in IOP of 2.7mm Hg after four hours.28
Nutritional supplements appear to offer significant ocular benefits for patients with AMD, cataract and glaucoma. However, few absolute conclusions and recommendations can be drawn from the recent explosion of research in the field of nutrition and eye. Nonetheless, as additional research is published, more robust conclusions on specific recommendations for nutritional supplement intake will become more readably available.
Mrs. Vyas is a registered dietitian, licensed dietitian and nutritionist. She currently practices at the Provena St. Joseph Hospital in Elgin, Ill. Dr. Gunvant is an assistant professor at Southern College of Optometry in Memphis, Tenn. and an adjunct assistant professor at the University of Louisville and the University of Memphis. They thank Ms. Meredith Cohler for her help in organizing this article.
1. Mahan K, Escott-Stump S. Krause’s Food and Nutrition therapy, 12th ed. St. Louis: Saunders Elsevier, 2008:532-62.
2. The United States Department of Agriculture. Summary Tables: Dietary Reference Intakes. Available at: www.nal.usda.gov/fnic/DRI/DRI_Energy/1319-1331.pdf?debugMode=false (Accessed August 31, 2009).
3. Carr AC, Frei B. Toward a new recommended dietary allowance for vitamin C based on antioxidant and health effects in humans. Am J Clin Nutr. 1999 Jun;69(6):1086-107.
4. Schmidt-Erfurth U. Nutrition and retina. In: Augustin AJ (ed). Nutrition and the Eye—Basic and Clinical Research. Basel, Switzerland: Reinhardt Druck, 2005:120-47.
5. Reiss GR, Werness PG, Zollman PE, Brubaker RF. Ascorbic acid levels in the aqueous humor of nocturnal and diurnal mammals. Arch Ophthalmol. 1986 May;104(5):753-5.
6. Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001 Oct;119(10):1417-36.
7. Beatty S, Koh H, Phil M, et al. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2000 Sep-Oct;45(2):115-34.
8. Brown NA, Bron AJ, Harding JJ, Dewar HM. Nutrition supplements and the eye. Eye. 1998;12 (Pt 1):127-33.
9. Richer S. Antioxidants and the eye. Int Ophthalmol Clin. 2000 Fall;40(4):1-16.
10. Carsten H. Nutritional Supplementation to Prevent Cataract Formation. In: Augustin AJ (ed). Nutrition and the Eye—Basic and Clinical Research. Basel, Switzerland: Reinhardt Druck, 2005:108.
11. Taylor HR, Tikellis G, Robman LD, et al. Viatmin E supplementation and macular degeneration randomized controlled trial. BMJ. 2002 Jul 6;325(7354):11.
12. Richer S, Stiles W, Statkute L, et al. Double-masked, placebo-controlled, randomized trial of lutein and antioxidant supplementation in the intervention of atrophic age-related macular degeneration: the Veterans LAST study (Lutein Antioxidant Supplementation Trial). Optometry. 2004 Apr;75 (4):216-30.
13. Moeller SM, Voland R, Tinker L, et al. Associations between age-related nuclear cataract and lutein and zeaxanthin in the diet and serum in the Carotenoids in the Age-Related Eye Disease Study, an Ancillary Study of the Women’s Health Initiative. Arch Ophthalmol. 2008 Mar;126(3):354-64.
14. Stahl W. Macular Carotenoids: Lutein and Zeaxanthin. In: Augustin AJ (ed). Nutrition and the Eye—Basic and Clinical Research. Basel, Switzerland: Reinhardt Druck, 2005:70-88.
15. Lutein Information Bureau. Lutein and Age-Related Macular Degeneration. Available at: www.luteininfo.com/eye (Accessed August 31, 2009).
16. Chong EW, Kreis AJ, Wong TY, et al. Dietary omega-3 fatty acid and fish intake in primary prevention of age-related macular degeneration. A systematic review and meta-analysis. Arch Ophthalmol. 2008 Jun;126(6):826-33.
17. Chasan-Taber L, Willett WC, Seddon JM, et al. A prospective study of vitamin supplement intake and cataract extraction among US women. Epidemiology. 1999 Nov;10(6):679-84.
18. Chasan-Taber L. A prospective study of carotenoid and vitamin A intake and risk of cataract extraction in US women. Am J Clin Nutr. 1999 Oct;70(4):509-16.
19. Kuzniarz M, Mitchell P, Cumming RG, Flood VM. Use of vitamin supplements and cataract: the Blue Mountains Eye Study. Am J Ophthalmol. 2001 Jul;132(1):19-26.
20. Lyle BJ, Mares-Perlman JA, Klein BE, et al. Antioxidant intake and risk of incident age-related nuclear cataracts in the Beaver Dam Eye Study. Am J Epidemiol. 1999 May 1;149(9):801-9.
21. Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E and beta carotene for age-related cataract and vision loss: AREDS report no. 9. Arch Ophthalmol. 2001 Oct;119(10):1439-52.
22. Chung HS. Ginkgo biloba extract increases ocular blood flow velocity. J Ocul Pharmacol Ther. 1999 Jun;15(3):233-40.
23. Quaranta L, Bettelli S, Uva MG, et al. Effect of Ginkgo biloba extract on preexisting visual field damage in normal tension glaucoma. Ophthalmology. 2003 Feb;110(2):359-64.
24. Jarvinen T, Pate DW, Laine K. Cannabinoids in the treatment of glaucoma. Pharmacol Ther. 2002 Aug;95(2):203-20.
25. Porcella A, Maxia C, Gessa GL, Pani L. The synthetic cannabinoid WIN55212-2 decreases the intraocular pressure in human glaucoma resistant to conventional therapies. Eur J Neurosci. 2001 Jan;13(2):409-12.
26. Beilin M, Neumann R, Belkin M, et al. Pharmacology of the intraocular pressure (IOP) lowering effect of systemic dexanabinol (HU-211), a non-psychotropic cannabinoid. J Ocul Pharmacol Ther. 2000 Jun;16(3):217-30.
27. Zhan GL, Camras CB, Palmberg PF, Toris CB. Effects of marijuana on aqueous humor dynamics in a glaucoma patient. J Glaucoma. 2005 Apr;14(2):175-7.
28. Tomida I, Azuara-Blanco A, House H, et al. Effect of sublingual application of cannabinoids on intraocular pressure: A pilot study. J Glaucoma. 2006 Oct;15(5):349-53.

