 |
A 47-year-old white female presented for a so-called routine exam, stating that she only needed her glasses updated. The patient said she had not noticed any recent changes in her vision, other than increased difficulty when reading. She also explained that vision in her right eye had been worse than the left eye for several years.
The patient denied any history of ocular trauma or surgery, and her medical history was unremarkable. She also reported experiencing much stress at her workplace.
On examination, her best-corrected visual acuity was 20/25 in the right eye and 20/20 in the left. Confrontation fields were full to careful finger counting in both eyes. Pupils were equally round and reactive, with no afferent pupillary defect. Motility testing was normal. The anterior segment exam was unremarkable.
Dilated fundus exam showed small cups with good rim coloration and perfusion in both eyes. The remainder of the fundus exam in the right eye was completely normal.
In the left eye, however, the fundus exam revealed a fine retinal stria, a suspicious lesion in the macula and retinal changes along the superior arcade (figures 1 and 2). Therefore, we ordered fluorescein angiography transitting the left eye (figure 3).
 |
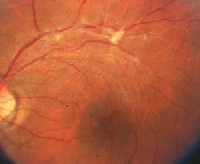 |
| 1. The fundus photo of the left eye shows a fine retinal stria, a suspicious lesion in the macula and changes along the superior arcade. | 2. The same image of the patients left eye is shown with 2x magnification of the macula. What is this suspicious lesion, and how do you account for the changes along the arcade? |
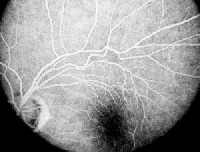 |
| 3. Mid-phase fluorescein angiogram in the left eye shows the changes as seen in the fundus photos. |
Take the Retina Quiz
1. What does the retinal stria in the macula represent?
a. Epiretinal membrane.
b. Serous retinal detachment.
c. Choroidal folds.
d. Proliferative vitreoretinopathy.
2. What does the change in the fovea represent?
a. Full-thickness macular hole.
b. Pseudomacular hole.
c. Cystoid macular edema.
d. Central serous chorioretinopathy.
3. What do the changes along the superior arcade represent?
a. Neovascularization elsewhere.
b. Fibrous tissue.
c. Retinal granuloma.
d. Tractional retinal detachment.
4. What is the etiology of the fundus changes in this patient?
a. Idiopathic.
b. Incomplete posterior vitreous detachment.
c. Stress.
d. Resolved branch retinal vein occlusion.
5. How should we manage this patient?
a. Observation and reassurance.
b. Pars plana vitrectomy and membrane peel.
c. Antihelmintics.
d. Grid laser photocoagulation.
For answers to this months quiz, please look below.
Discussion
The fine retinal stria seen in our patient was caused by an epiretinal membrane (ERM). An ERM represents a fibrocellular membrane that grows onto the surface of the internal limiting membrane.
ERMs most often are associated with a posterior vitreous detachment (PVD), but no PVD was present in our patient. Instead, we observed a localized area of traction and a dense, whitish area of fibrous tissue along the superior arcade. The fibrous tissue appeared similar to a small granulomaa nodular aggregation of inflammatory cells that results from infection or inflammation. However, the fibrous tissue in our patient more likely was a denser area of scar tissue from which the ERM originated.
The ERM extends into the macula, where we also observed a round, reddish elliptical lesion. The lesion looked like a macular hole, but its irregular shape, its location just off center of the fovea and the patients relatively good acuity suggested a pseudomacular hole.
A pseudomacular hole results because the ERM contracts around the macula, but spares the fovea. The color contrast between the ERM and the fovea simulates a full-thickness macular hole. Also, a full-thickness macular hole, which represents a full-thickness defect in the retina, typically is round and has a cuff of fluid around its edges. The lesion in our patient did not have the cuff of fluid, and its shape was more elliptical.
So, how do we explain these findings in a healthy, asymptomatic 47-year-old? And, what can we do about it? If we look at the fibrous tissue along the arcade, we see that there is a sheathed artery as it crosses the vein superiorly. Our patient most likely had a branch retinal vein occlusion (BRVO) at the site of this crossing.
As the hemorrhage from the BRVO resolved, scar tissue then developed in the form of an ERM. We may never know for sure what happened to this patient, as we did not see her when the BRVO occurred, and it appeared to be present for some time.
Should we be concerned that a BRVO may have occurred in a young, healthy patient? While BRVOs mostly occur in an older population and are strongly associated with hypertension and diabetes, they also can occur in younger patients.
In a study of 1,090 patients who had various forms of retinal vein occlusions, 16 (5%) of those occlusions occurred in patients younger than age 45, and 152 (45%) occurred in the 45- to 64-year-old group.1 There was a strong association with arterial hypertension and diabetes in both age groups. So, patients who present with branch or central retinal vein occlusion should undergo a medical evaluation.
Our patient said that her blood pressure has always been normal, and it measured 125/80 at the time of her visit. We decided to observe her, given that her acuity was good and appeared stable.
We discussed our findings with the patient and gave her a letter to give to her primary-care physician. However, she said that she had recently seen her doctor, who told her that her systemic health was normal.
We also prescribed new glasses with increased add power to address her near vision complaints.
Retina Quiz Answers: 1) a; 2) b; 3) b; 4) d; 5) a.
1. Hayreh SS, Zimmerman B, McCarthy MJ, Podhajsky P. Systemic diseases associated with various types of retinal vein occlusion. Am J Ophthalmol 2001 Jan;131(1):61-77.

