 |
We often think about our dry eye patients’ daytime experiences and how these may exacerbate their symptoms. But in fact, the greater culprit may be lurking in a patient’s nighttime environment. Consider that 61% of symptomatic dry eye patients across the spectrum of disease severity have compromised lid closure.1
If you have a patient whose dry eye is not improving despite treatment, it’s time to consider inadequate eyelid closure, sometimes referred to as nocturnal lagophthalmos. This form is far less obvious, as this under-identified and under-treated condition is caused by nocturnal evaporative stress (NES) and is highly prevalent in refractory dry eye.1
Causes
Our eyes don’t produce as many tears while we’re sleeping, which automatically puts patients in a dry eye state during sleep.2 Closed lids protect the eye from desiccation.3 However, many patients’ lids don’t adequately close at night. Several factors contribute to the development of NES, many of which are directly linked to inadequate lid seal (ILS). These include floppy eyelid syndrome, surgical cosmetic procedures and injections, lid deformities, age-related lid laxity, dermatochalasis, senile ectropion and Graves’ disease.3,4
In addition, patients with NES often have another condition, such as meibomian gland dysfunction (MGD), that contribute to the disease. Environmental factors likewise should be considered. A fan in the bedroom, CPAP devices or forced air heat can make symptoms worse. Newer research indicates that even in the majority of patients who show no apparent lid abnormalities, insufficient lid seal is present and leads to nighttime dryness.5
 |
|
The Korb-Blackie light test can detect ILS by determining if the patient’s closed lids are protecting the ocular surface and preventing evaporation during sleep. Click image to enlarge. |
Diagnosis
Despite our busy schedules and heavy patient loads, investigating NES in new dry eye patients as well as refractory cases is time well spent. This can be as easy as asking patients how their eyes feel when they first wake up. If they say their eyes feel fine in the morning but get worse throughout the day, we can usually rule it out. Conversely, if the patient indicates their eyes feel particularly bad upon waking, ILS is the likely diagnosis.
The Korb-Blackie light test is probably the most simple and straightforward way to detect ILS if you feel the need for a confirmatory test beyond morning symptoms. This test helps you determine whether a patient’s seemingly closed eyelids are actually protecting the ocular surface and preventing evaporation during sleep.6 Simply darken the room and place a transilluminator against the patient’s closed outer upper eyelids. As you direct the light toward the interpalpebral fissure, look for light leakage along the lid and between the lashes.6 Repeat on the second eye.
The more light that leaks, the worse the seal and the greater the exposure. In fact, research shows that nocturnal lid seal insufficiency is associated with desiccating stress and greater symptom severity.7 It is also useful to ask the patient to squeeze their eyes shut to determine whether complete closure is even possible.
Another useful test is the lid snap. To test elasticity, simply pull down the patient’s lower lid and let it snap back into place. If the lids return to their normal position slowly, the patient has poor lid performance, putting them at greater risk of having problems at night.
 |
|
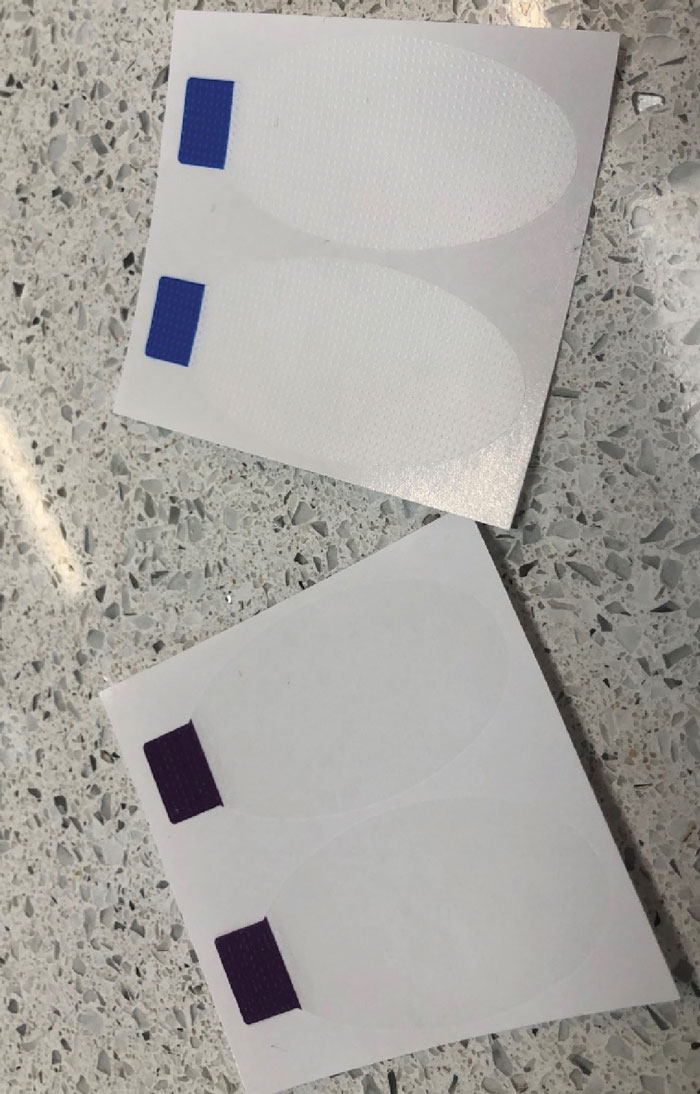
SleepTite, a daily disposable lid seal, is a single-use, hypoallergenic device that holds the eye closed to prevent NES due to inadequate lid closure. Click image to enlarge. |
Treatment
If you are trying to treat a patient’s ocular surface disease but not managing their ILS, there is an uphill battle to climb, as you’re often treating the resulting inflammation, corneal staining or desiccation, MGD and blepharitis without treating the cause. For that reason, a treatment that addresses the lids would be ideal; however, until now, these options were limited.
Other than surgery, there’s sleep masks, but they only work for select patients. Sleep masks don’t address the cause—inadequate light seal—but they may provide a brief moisture chamber if the patient is able to maintain them throughout the night. Other options include instillation of gels or ointments before bed, but these don’t create a long enough seal to prevent NES. A re-evaluation of the bedroom environment can also help, such as eliminating ceiling fans, but many patients say it helps them sleep. Directing all fans and vents away from the bed and keep bedding pillows and mattresses clean and as free from dust mites as possible can help.
There’s also a daily disposable lid seal, SleepTite, which is a single-use, hypoallergenic, latex-free device intended to hold the eye closed to prevent NES due to inadequate lid closure. Each card has two eye covers that can be applied universally to either eye. Instructions are straightforward and it’s best to begin with having the patient close one eye overnight.
Patients are instructed to place the eye cover over the closed eye. The tab can be oriented laterally or medially for best fit. Gently seal the cover by running a finger around the entire edge of the oval. Upon awakening, the patient easily removes the eye cover by gently grasping the colored tab and pulling in a downward direction so that the eye is not opened during removal. The device should then be discarded. If they find they are not getting up often during the night and the device is working well for them, they can transition to bilateral placement.
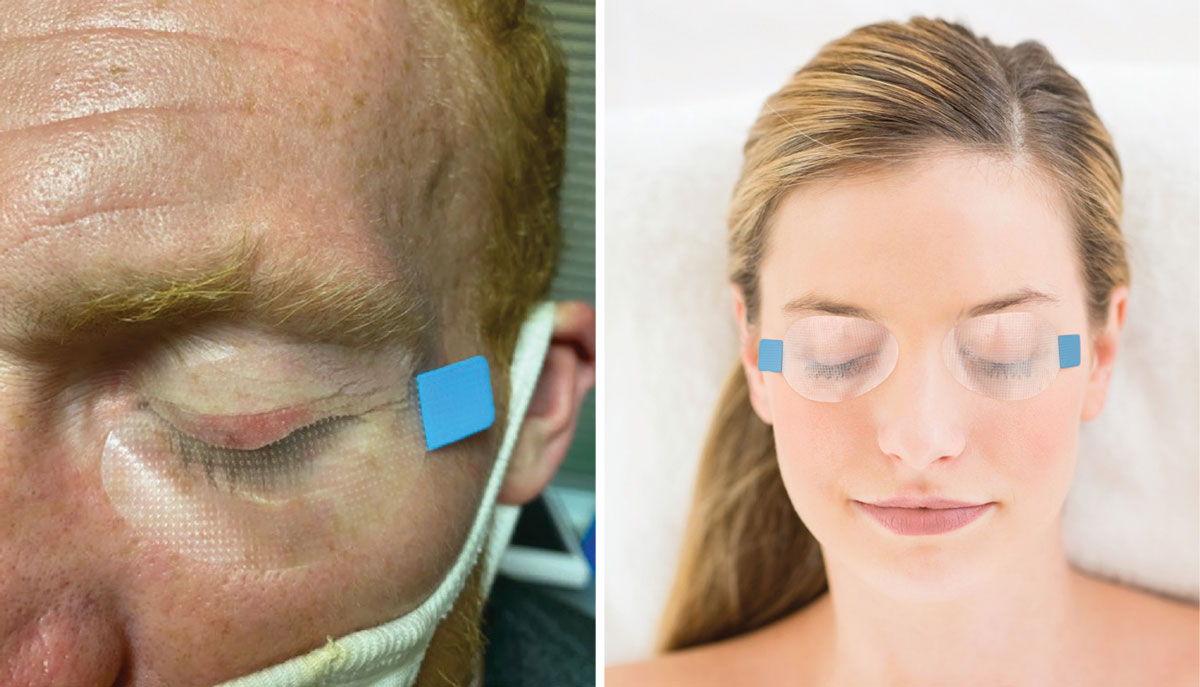 |
SleepTite being used post-amniotic membrane placement on the left. Most patients should begin by closing one eye each night, although some will be able to apply it bilaterally in time, as shown on the right. Click image to enlarge. |
In my experience, not only has this product been the single most effective treatment for recalcitrant dry eye, it has also changed people’s lives and their need for chronic therapy. Many even comment that it has allowed them the best sleep they’ve had in decades, likely due to the lack of light entering the eye. By treating the cause of ocular surface desiccation and MGD, you can often relieve these patients of multiple adjunctive therapies.
We only recently discovered that inadequate lid closure occurs in patients who appear to have normal lid structure and performance. It’s a seemingly small discovery, but it’s one that can make a significant difference in patient outcomes and is likely to be the number one cause of morning symptoms in those who don’t respond to ocular surface disease therapies.
Dr. Karpecki is medical director for Keplr Vision and the Dry Eye Institutes of Kentucky and Indiana. He is the Chief Clinical Editor for Review of Optometry and chairman of the affiliated New Technologies & Treatments conferences. A fixture in optometric clinical education, he provides consulting services to a wide array of ophthalmic clients. Dr. Karpecki’s full disclosure list can be found here.
| 1. Korb D, Blackie C, Nau A. Prevalence of compromised lid seal in symptomatic refractory dry eye patients and asymptomatic patients. Invest Ophthalmol Vis Sci. 2017;58:2696. 2. Blackie CA, Korb DR. A novel lid seal evaluation: the Korb-Blackie light test. Eye Contact Lens. 2015;41(2):98-100. 3. McNab AA. The eye and sleep. Clin Exp Ophthalmol. 2005;33(2):117-25. 4. Latkany RL, Lock B, Speaker M. Nocturnal lagophthalmos: an overview and classification. Ocul Surf. 2006;4(1):44-53. 5. Gauba V, Curtis ZJ. Sleep position and the ocular surface in a high airflow environment. Saudi J Ophthalmol 2014;28:66-8. 6. Korb D, Blackie C. The Korb-Blackie lid light test. Invest Ophthalmol Vis Sci. 2013;54:942. 7. Korb, D. Blackie, C. Nau, A. Prevalence of compromised lid seal in symptomatic refractory dry eye patients and asymptomatic patients. Invest Ophthalmol Vis Sci. 2017;58:2696. |

