Get a Head Start on Specialty Contact LensesIn the August 2024 issue of Review of Optometry—our 48th annual Contact Lens report—experts provide the tips and tools you need to start offering specialty lenses at your practice. In two more features, the authors deep-dive into soft lens optics and CL complications. Check out the other articles featured in this issue:
|
Despite the wide range of successful mass market products, many patients continue to need specialty contact lens (CL) care. However, it’s not always easy to build a thriving practice. I have started two of them: one in an ophthalmology group and the other in an optometric private practice. There is potential for anyone who enjoys the challenge of specialty contact lenses and who is willing to put in the effort. Here are some tips to help you make it happen.
1. Expertise and Education
Specialty CL patients need and deserve a high level of care. They may have disfigured corneas, endured unwanted surgical complications or suffer from conditions that hitherto could not be ameliorated.1 Many of these people are hurting emotionally and need our empathy as much as our prowess. Others simply have a tricky prescription that’s poorly served by off-the-shelf contact lenses.
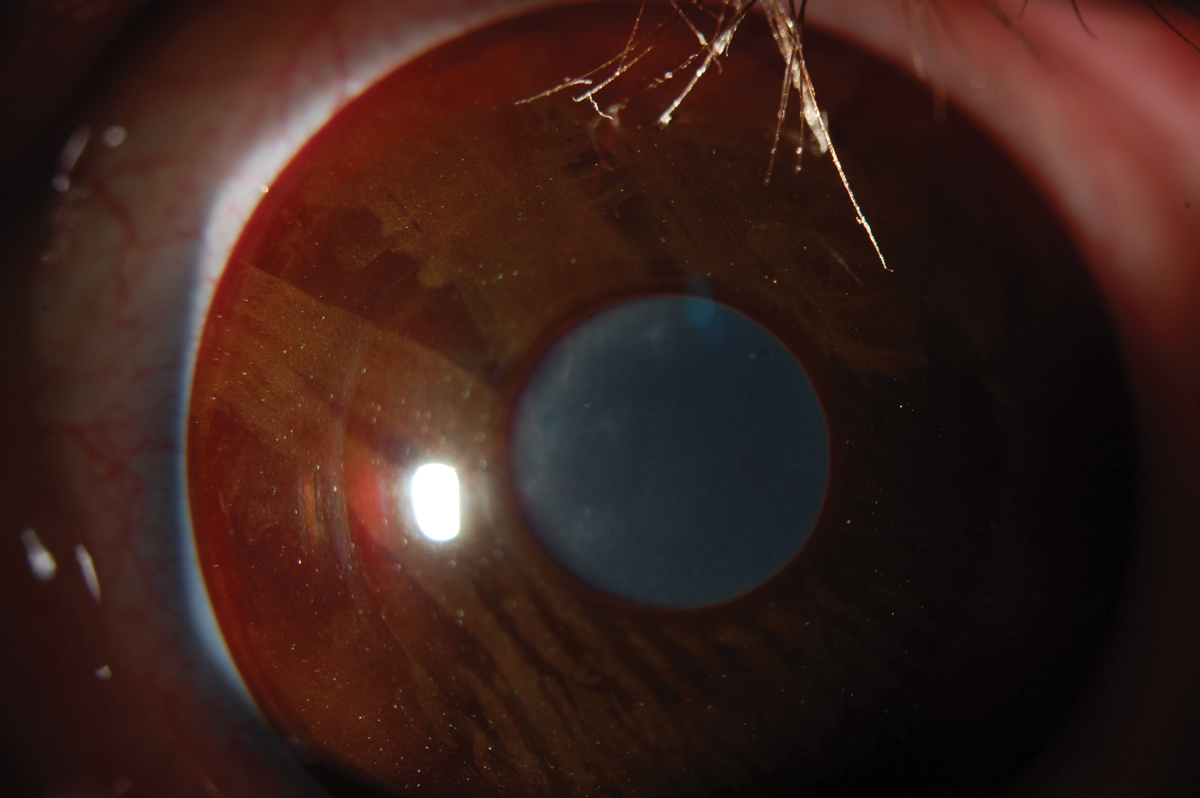
Who are the patients that you will be serving? Their diagnoses include: keratoconus, keratoglobus, pellucid marginal degeneration, corneal dystrophies and degenerations, corneal scarring due to prior trauma or infection, post-corneal transplantation, dry eye disease, ocular surface disease, post-refractive surgery (LASIK, PRK, RK), irregular astigmatism, high astigmatism, presbyopia, children with myopia, normal cornea patients unsuccessful with other CL modalities, exposure keratitis, high ametropia, anisometropia and iris anomalies (e.g., aniridia, coloboma) (Figure 1).
How you develop this skillset depends on your training. Fortunately, my contact lens education during optometry school was strong, and I bolstered that with additional cornea and contact lens coursework for my Master of Science in Physiological Optics. My research project and master’s thesis were on the topic of keratoconus. Then during my residency, I spent one afternoon per week fitting irregular corneas in a specialty contact lens clinic. Others may spend an entire year in an accredited cornea/contact lens residency. Upon completion, they are ready to see any type of CL patient and should be confident enough to fit lenses.
If you did not develop enough advanced experience in these areas during your training, there are plenty of opportunities to do so after graduation. These can include the following:
• Use your laboratory. This can include both the account representatives and the telephone-based consultants. They can help you with the nuances of fitting their lenses as well as practice management. Many laboratories also sponsor webinars and in-office or group wet labs with hands-on training.
• Observe a busy specialty contact lens practice. I have hosted many colleagues over the years. The practical information learned from observing even a half day of specialty lens fits will be valuable. Seek out someone who sees them all day, every day. Those of us who do this for a living are happy to help.
• Invite a specialty CL expert to your practice. Sometimes a laboratory can help you set this up. I personally have enjoyed assisting my colleagues with some of their most challenging fits.
• Immerse yourself by reading journal and magazine articles. Review of Cornea and Contact Lenses is jam-packed with detailed information five times per year.
• Dedicate an entire continuing education conference to attending CL courses. Many of the larger meetings, e.g., the American Academy of Optometry’s (AAO) or Optometry’s Meeting, offer several days-worth of CL courses. Other meetings cover all types of specialty lens topics in one conference. While there, take a “hands-on” fitting workshop or an interactive course. If you do this for several years, you will become an expert in the design and fitting of these lenses.
• Consult a textbook. The comprehensive texts review every type of specialty contact lens, as well as all types of CL fittings.2-4 However, email newsletters often provide the most current information for the clinician, as they provide links to the latest research, summary articles and new technologies.
• For elite competency, pursue a higher certification. Although these programs may initially seem challenging, peer review/collaboration is the only way to become the best of the best. For overall knowledge (you can always select contact lens cases to write), pursue the Fellowship in the AAO. For just scleral lenses, consider the Fellowship in the Scleral Lens Education Society (SLES). For a comprehensive specialty lens experience, the Diplomate of the AAO Section on Cornea, Contact Lenses and Refractive Technologies offers the best process in the US. What’s great about these programs is the ability to meet others—whether candidates like yourself or existing Fellows/Diplomates—who share your passion for specialty contact lenses.
 |
|
Fig. 1. A soft prosthetic contact lens for aniridia. Click image to enlarge. |
2. Good Relationships
If you want to help patients who need specialty lenses, they need to find a way to your chair. Good referral sources include optometrists, cornea specialists, general ophthalmologists, oculoplastic surgeons, neuro-ophthalmologists, oncologists, endocrinologists, rheumatologists, hematologists, otolaryngologists, pediatricians, primary care providers, opticians and the colleagues and patients of your own practice.
To spread the word regarding your offerings, use personal practice visits, letters, emails, phone calls, texts, your website and social media (for example, a local Facebook page). You can also advertise using print media, television and radio. Make sure that your practice appears on the doctor locator page of organizations like the Gas Permeable Lens Institute (GPLI), SLS and National Keratoconus Foundation (NKCF). These groups also provide excellent practitioner and/or patient education. Word-of-mouth can also be a practice-builder. For example, an OD colleague on maternity leave asked me if I would see her specialty CL patients while she was out. Another optometrist friend recently retired and asked if I would take on her keratoconus patients.
Following the referrals, good working relationships with the referring doctors help sustain the best care for the patient—and lead to future referrals. Collegial communication is so important. For example, I frequently exchange text messages with the ophthalmologists with whom I comanage. Once the fitting is complete, I send a summary report to the referring provider, thanking them and providing an update.
Another benefit to joining a group like AAO Diplomate is the built-in network of experts from throughout the country and world. When a colleague’s patient moves into my area, they know they will be in good hands with me and vice versa.
3. Diagnostic Lenses
Although we are fitting more and more specialty lenses empirically, their complexities often dictate an initial on-eye fitting. That saves a visit for the patient and chair time for your practice. For a full-scope specialty contact lens practice, at least one type of fitting set is needed in each of these categories:
- Corneal spherical GP
- Corneal keratoconic GP
- Corneal reverse geometry GP
- Scleral GP
- Multifocal corneal GP: aspheric*
- Multifocal corneal GP: translating*
- Multifocal soft: center distance
- Multifocal soft: center near
- Multifocal soft: myopia control
- Orthokeratology GP*
- Keratoconic soft
- Hybrid
*if recommended by your lab
 |
|
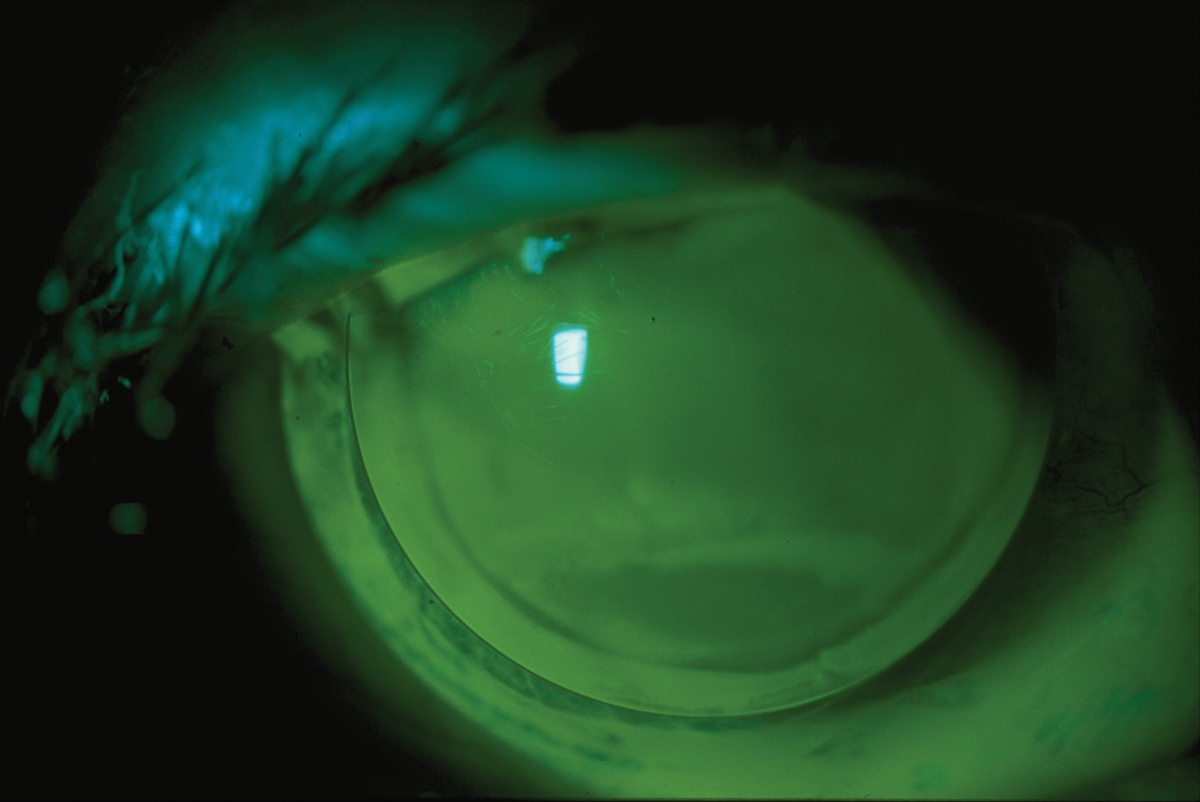
Fig. 2. No specialty CL practice is complete without a concentration in corneal GP contact lenses. Click image to enlarge. |
4. Practice Support
It is important that your practice is fully on board with supporting a specialty CL service. There must be adequate spacing and good employees to help. In addition, the staff need to be sensitive towards the patients’ emotional needs. Many of them can’t see well with glasses due to their serious ocular condition and require a good deal of patience. If they call to replace a lost or broken contact lens, their request must be addressed immediately.
If you are an associate and want to start this service, communicate your interest and passion in specialty contact lenses to your employer immediately. Of course, this might begin at the interview when you describe your expertise in this area and how it can better serve and add value to the practice.
5. Scheduling Considerations
The practice must understand that these visits are not routine. They take longer, and more attention must be made to their scheduling. For scleral lens dispensing visits, a 30-minute lens settling period must be built into the schedule. In my practice, those patients are given an appointment time 30 minutes prior to when they will see me. I then overlap appointments to ensure maximum efficiency. For the initial patient evaluation, meanwhile, we book 30 to 45 minutes, and tell them that between the testing, fitting and lens settling, they may be in the office for up to two hours. This visit may include:
- Complete history of contact lens wear (prior records with current contact lens parameters are important).
- Thorough history of contact lens care, since sometimes it is poor CL care and compliance, rather than the fit, that led to discomfort.
- Corneal topography/tomography.
- Refraction.
- Pachymetry/specular microscopy.
- External ocular photography.
- Visual acuities and entrance testing.
- Slit lamp examination with sodium fluorescein and lid eversion.
- Measurement of horizontal visible iris diameter (HVID).
- Contact lens trial fitting.
- Comprehensive education/reassurance regarding the patient’s condition, including handouts.
Other testing on the first day that may be used includes keratometry, aberrometry, OCT, meibography, axial length measurement (for myopia management) and scleral profilometry.
6. Layout/Supplies
Your office should ideally possess a nice, comfortable, clean, well-lit room dedicated to CL training and education. The supplies you will need include:
- A stand-up and a flat mirror, the latter for helping apply scleral lenses.
- GP and soft CL rinsing and soaking solutions.
- Preservative-free solution to fill a scleral lens.
- Large and small contact lens suction cups/DMV insertion/removal tools.
- Handout explaining insertion, removal and care.
- Sodium fluorescein.
- Extra contact lens cases.
- A scleral lens insertion stand.
- A handheld cobalt blue light.
- Chairs for the patient and staff member.
- Gloves and plexiglass shield (post-pandemic).
- GP daily cleaner and hydrogen peroxide for the disinfection of reusable trial lenses.
Many advanced contact lens practices also possess a radiuscope, lensometer, hand magnifier, laboratory-strength contact lens cleaner, and/or a modification unit with polish, suction cups and spinner tools. It’s difficult to say when exactly these should be incorporated into your practice, but I think you can’t have the best specialty CL practice without them.
 |
|
Fig. 3. It is important to demonstrate items that facilitate scleral lens insertion; without them, some patients may discontinue lens wear. Photo: Dalsey Adaptives. Click image to enlarge. |
7. A Motivated, Empowered Staff
Often, what separates the great practices from the good ones is the staff. When interviewing, select them for their empathy and their positive disposition. The skills they need can be trained.5
Your staff members are an extension of you. With a positive encounter, the patient’s takeaway will be a good impression of the practice and a positive attitude toward contact lenses.6-8 For example, it is important that you impart to staff your philosophy on CL care and follow-ups so that your patients will receive the message that you want conveyed. During case history, they should ask patients how they clean their lenses “from the time they start until the time they finish;” then compassionately correct them if they’re deviating from your instructions. Although patients may be initially embarrassed by their noncompliance, they ultimately appreciate how much we care about their eyes.6
A good staff member is vital to successfully completing the contact lens application/removal/education visit (Figure 3). It is the patient’s first experience applying contact lenses (or a new type of lenses, such as sclerals), and they may be nervous. If it doesn’t go well, they are more likely to drop out of contact lenses, even if the vision and fit are excellent. This encounter isn’t easy at first, and this is especially true for specialty CL patients, as they may struggle to see. A good technician uses a positive attitude, patience, contact lens knowledge and a good sense of humor to put the patient at ease. A successful dispensing visit lays the foundation for years of healthy contact lens wear.5 Often, a close bond will form between the technician and patient during the insertion and removal session, which is beneficial to both parties—and to the practice. Analogous to a dental hygienist in a dentist’s office, your technician may spend more time with your patients than you do.
At my practice, insertion and removal typically are not done on the first day, but rather when the patient comes back to pick up their lens. Remember they have been there for up to two hours and are exhausted after that first day. Also, some patients elect not to order the CL at all on the first day after we have completed the testing. So, performing insertion and removal on that day is not prudent.
Train at least one staff member to understand the medical and vision insurance plans that you accept. It is beneficial to verify benefits prior to the first visit and then obtain pre-authorization for potential coverage of medically necessary contact lenses. This is especially important for vision plans, where materials are more likely to be completely or partially covered. In my practice, I initially provided my specialty contact lens coordinator videos, articles, courses and webinars. The information may be overwhelming at first, but a well-trained and capable staff member will master it. The ultimate goal is for them to be more familiar with coding and billing than the doctor. The practice will reap the benefits.
Specialty contact lens designs include parameters that spherical lenses do not have. And what’s more, the terminology for these numbers may differ from lab to lab. A staff member must understand the technical terms and abbreviations well enough to order the lenses accurately, because every parameter matters with these lenses.
A large practice may have four separate individuals performing these important functions; in a small practice, it may be the same person, with help from the doctor. Regardless of how many staff members are involved, their attention to detail is vital to the success of any specialty contact lens practice.
Once they gain some experience, involve them. Ask them for their input. Some of their ideas may impress you. Then reward them for their contributions. I recently nominated my technicians for a national award (2023 Contact Lens Institute; www.contactlensinstitute.org/resources/awards), which they received. We hosted an in-office reception for them, inviting family, friends and referring doctors.
Worth the Effort
The rewards of fitting specialty contact lenses go beyond financial. These patients continue to challenge and inspire me. It is gratifying to restore sight, correct vision, enhance comfort, improve appearance and prevent myopia progression. These lenses have brought immense satisfaction not only to my patients but also to their doctor.
Dr. Gromacki is a fellow of the American Academy of Optometry and a diplomate in the Cornea, Contact Lens and Refractive Technologies section. She serves as the director of the Contact Lens Service at a subspecialty group practice in Maryland. In the past year, she has received consulting fees from Alcon, Bausch + Lomb SVP, Glaukos, Johnson & Johnson Vision Care and Tarsus, as well as speaking fees from Bausch + Lomb SVP, GPLI, Glaukos, Johnson & Johnson Vision Care, PSS Eyecare and Wink Productions.
1. Gromacki SJ, Seligson V. Diagnosing keratoconus without a topographer. Optometric Management. 2014;49(6):47-50. 2. Bennett ES, Henry VA. Clinical Manual of Contact Lenses (5th ed). New York: Wolters Kluwer; 2020. 3. Bennett ES and Weissman BA. Clinical Contact Lens Practice (2nd ed). New York: Lippincott Williams & Wilkins; 2005. 4. Hom MM, Bruce AS. Contact Lens Prescribing and Fitting with CD-ROM. Boston: Butterworth-Heinemann; 2006. 5. Gromacki SJ. Want to build a top CL practice? Contact Lenses Today. 2015;17:3. 6. Gromacki SJ. A good tech means good care. Contact Lens Spectrum. 2004;19(10):25. 7. Gromacki SJ. Instructions for scleral lens application. Contact Lenses Today. 2013; November 3:3. 8. Gromacki SJ. Contact Lens Training Today. Rev Optom. 2011;148(5):73-6. |

