Cornea ReportCheck out the other feature articles in this month's issue: |
With constant, eye-drying, unblinking screen use becoming ever more the norm, ocular surface disease (OSD) is more prevalent than ever. As OSD worsens, patients can start to develop recurrent corneal erosions (RCE), a painful condition that exposes their corneal nerve endings. These patients will likely complain of eye pain upon awakening, with accompanying photophobia and epiphora. They may also present with conjunctival injection, blurred vision and difficulty even keeping their eyes open. It is not unusual to note a drastically worsened Snellen acuity.
The optometrist’s job is to ensure patients’ health and vision. RCE can compromise both. Management of those susceptible to this condition requires a correct diagnosis and close follow-up to care for and treat not only the RCE but any underlying conditions, such as epithelial basement membrane dystrophy (EBMD) and dry eye disease (DED), that play a role in its recurrence.
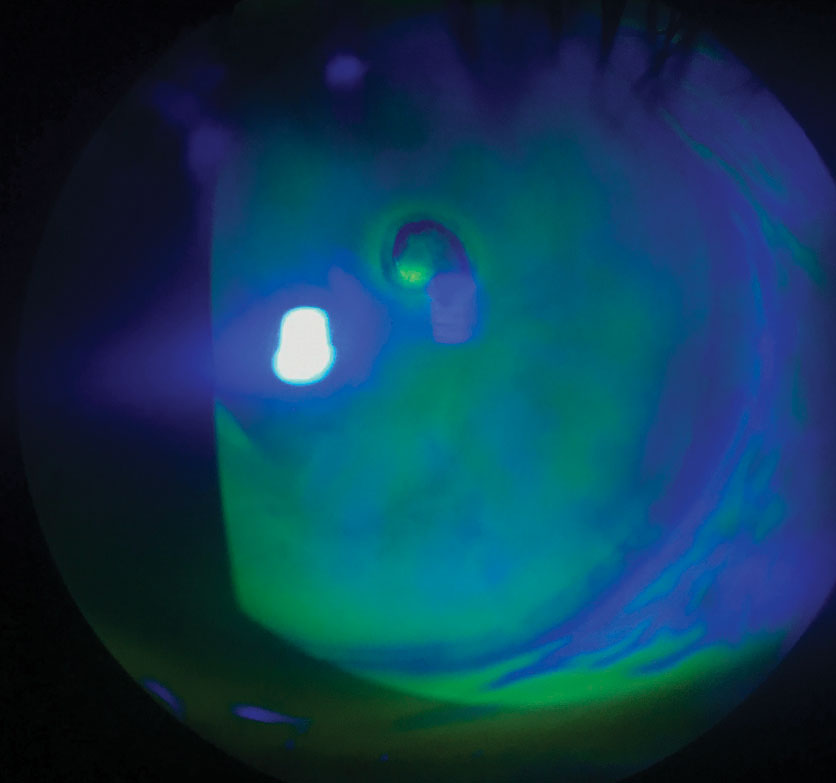 |
| This positive fluorescein staining shows a central epithelial defect with healing margins and inferior pooling from RCE at the patient’s second visit. |
Day One Do’s and Don’ts
The epithelial cells must heal before you can add a steroid to control the inflammation. Most often, once the defect is healed, the stromal edema will resolve as well. At the patient’s initial visit, place a bandage contact lens (BCL) for comfort. If chemosis is present, a lens with a base curve of 8.6mm is usually necessary.
To prevent infection, apply a broad-spectrum antibiotic drop, such as a fluoroquinolone, until the next visit; however, it is inadvisable to use Besivance (besifloxacin 0.6%, Bausch + Lomb) in the case of an epithelial defect due to the formulation of the suspension. Besifloxacin 0.6% is formulated with DuraSite (InSite Vision), a polycarbophil, edetate disodium dihydrate and sodium chloride vehicle.1 Be mindful of reported adverse effects including corneal edema and glaucomatous damage.1,2 DuraSite blocks the trabecular meshwork and can be toxic to the ocular surface when used in medications prescribed at a large and intensive dose.2 Prescribed at low doses, drugs that contain DuraSite may cause corneal edema, inflammation and adverse effects even after only a single dose.3 The suspension has a bioadhesive delivery system, which allows for longer drug release time; therefore, it should be avoided in RCE patients.4
Starting treatment with one drop of a topical fluoroquinolone every two hours may be necessary if the chance of infection is higher. Reduce it to one drop four times a day once the erosion begins to heal and until the BCL is removed.
Prescribing an oral antibiotic such as doxycycline 50mg (one tablet taken twice daily), aids the healing process and prevents the risk of perforation. Normally, you’d be concerned about perforation if an ulcer is present; however, even with RCEs, doxycycline can be an effective treatment aid.5 By chelating metal ions that are structurally essential for the corneal epithelium, doxycycline irreversibly inhibits corneal matrix metalloproteinases (MMPs), such as MMP-2 activity since it is Ca2+ dependent, as the antibiotic partially extracts the tightly bound ion from the active hemidesmosome site of the protein.6 In addition to inhibiting MMP activity, it also inhibits the synthesis of MMPs and proinflammatory cytokines, such as IL-1.6
The broad-spectrum antibiotic also kills migratory keratocytes responsible for the formation of scar tissue, which in turn allows full coverage of epithelial basal cells to form and the development of stratified epithelium. Researchers observed this at a minimum concentration of 100µm, which is similar to that required in other tissues.6 In addition, by using doxycycline at a low dose of 50mg BID, the benefit is still seen without the negative side effects of gastritis and phototoxicity.
Be sure to ask the patient about their job and daily activities. If they report that they’re frequently in a dusty or dirty environment or engage in heavy lifting, it may be necessary for them to wait to return to work until the epithelium heals to lower the chance of infection. Once the epithelium is healed, the doxycycline can be discontinued; however, it is safe to keep the patient on the antibiotic for a full month or more at this low dose until the risk is minimized. Recommending over-the-counter pain relievers, prescribing a topical cycloplegic or suggesting a cold gel pack will also keep the patient more comfortable.
Two-day Follow-Up
These patients need close monitoring and should return for a follow-up visit within two days. Be sure the patient knows to call if they experience any reduction in vision, as you may want to see them sooner than scheduled. Removal of the BCL may be necessary to fully assess the healing defect with subsequent staining of fluorescein. If the cells are present but irregular, it may be safe to only use artificial tear lubrication, over-the-counter ointment QHS and continue the doxycycline for the full course of treatment. If the defect is still present, a replacement BCL should be placed on the eye; however, if the defect is larger or is not healing well, other treatment courses may be necessary.
Dealing with Complications
If the defect is slow to heal, or does heal but the epithelium breaks down again, it’s time to turn to a complication protocol. Usually, if the epithelium regresses, it does so following the removal of the BCL where the cells are not fully adherent yet. In one study of 13 clinically successful cases where an 8.6mm BCL was used for an abrasion for an average of 24.9 hours, five cases had persistent corneal epithelial defects, despite clinical improvement or reported resolution of symptoms.7 Another showed that treatment with only a bandage contact lens had a 25% recurrence rate.8 If this occurs, consider using an amniotic membrane. This is used often in our practice to aid the restoration of the epithelium faster while reducing the risk of haze.
Using Amniotic Membranes
Studies show that amniotic membranes are helpful in the healing process through anti-inflammatory cytokines and peptides that promote tissue repair.8,9 They acheive this by reducing both inflammation and scarring as well as angiogenic actions (by inhibiting MMPs).8,9 However, they are not considered a curative treatment.8,9
Currently, three manufacturers offer these products, which come in both dehydrated and cryopreserved forms, each with their own benefits and drawbacks. However, for a diagnosis of RCE, either membrane would support the epithelial healing process.10
The Prokera (Bio-tissue) is a cryopreserved amniotic membrane recognized for wound healing, inhibiting angiogenesis, reducing inflammation and minimizing corneal scarring and pain.11 It has anti-inflammatory effects and contains neurotrophic factors that may promote corneal nerve regeneration.11 Due to its considerable diameter, it covers large areas of epithelial defects as well as the limbus.11 Some patients may tolerate the large ring better with taping of the upper eyelid closed or partially closed. The product comes in Slim or Plus options. The Slim is slightly more comfortable for the patient and is therefore typically used initially. If the Slim dissolves in less than a week and the defect is still present, a Plus can be used.
Follow-up should be within four to seven days, giving the epithelial defect time to restore. If the defect is smaller or the patient cannot tolerate the ring, a dehydrated membrane is a good option.
The BioDOptix (Integra) is a dehydrated amniotic membrane that retains devitalized cellular components and has growth factors, such as vascular endothelial growth factor (VEGF), platelet-derived growth factor and insulin-like growth factor, as well as interleukins and tissue inhibitors of metalloproteases shown to modulate inflammation.12,13 It comes in 2cm x 3cm or 1.5cm x 2cm sizes.
To use this membrane, first lubricate the cornea with an artificial tear. Carefully grab the edge of the membrane disc with a pair of jewelers forceps and place the stromal (dull) side of the disc down on the lubricated cornea over the epithelial defect. A pair of paddle forceps works best for this since the tips are flat, thus reducing the risk of tearing the membrane. If the cornea is lubricated well enough, the disc should immediately adhere to the surface and rehydrate on contact. Do not try to smooth wrinkles or bubbles if any are present. A BCL can then be placed directly over the membrane for added protection and comfort.
The AmbioDisk (Katena) is also a dehydrated amniotic membrane. The product comes in 9mm, 12mm and 15mm sizes. The membrane is preserved in a process known as purion, in which key restorative elements such as epidermal growth factor, interleukin-10, VEGF and many others are preserved from their original state.14 The allograft is placed with the basement membrane side down, adjacent to a dry corneal surface, which can then be smoothed out with non-toothed forceps. A bandage contact lens or suture material can be used to allow the membrane to retain adherence to the cornea.
With any of these procedures, it is imperative that the patient keep the eye lubricated with preservative-free artificial tears, not only for comfort, but for healing purposes. The patient’s current antibiotic and steroid drop regimen is fine to keep after placing the membrane on the eye.
Research shows that using an amniotic membrane rather than a BCL allows the patient to potentially go longer before recurrence of the erosion. One study resulted in a 25% recurrence rate within one year after a three-month treatment period with a bandage contact lens, while in a similar study, after treatment with an amniotic membrane, only a 10% recurrence rate was seen within one year.8,15
If an amniotic graft is used, be sure to follow up within five to seven days, giving the membrane time to promote surface healing.
About this SeriesTo help optometrists strengthen their protocols for managing conditions that require ongoing—perhaps life-long—care, this series explains the steps to take after confirming a diagnosis, from day one through long-term management. Each installment in the five-part “Now What?” series will cover a different chronic condition: March—My Patient Has Glaucoma...Now What? April—RCE May—diabetic retinopathy June—scleritis July—AMD Be sure to check www.reviewofoptometry.com for any articles you may have missed. |
Fourth Follow-up
At the five-to-seven day follow-up, if the epithelial defect is still present, place another amniotic membrane; however, if the epithelium is healed but the cells are irregular, a bandage contact lens can give enough coverage for the epithelium to smooth over until it is completely adherent. Throughout the process, lubrication is key, which should be stressed to the patient. In addition to the oral antibiotic and broad-spectrum antibiotic drop, using preservative-free artificial tears will support a healthy environment for the cornea to heal. Once the membrane or BCL is permanently removed, the patient should add an over-the-counter ointment at bedtime, such as Muro 128 sodium chloride (Bausch + Lomb) ointment to prevent a breakdown of the epithelium overnight. Since Muro 128 ointment is a hypertonic agent, it provides better coverage and relief from any corneal edema present, while also being preservative-free, unlike other over-the-counter gels and ointments.
If inflammation is still present or anterior stromal haze has developed, add a steroid such as loteprednol, fluorometholone or prednisolone acetate twice daily, until the inflammation has resolved and the haze is reduced. Even if a little inflammation and haze presists, once the epithelium is present, adding a low-dose steroid has its benefits.16 Research shows MMPs accumulate in tears of patients with any ocular surface disease and are mainly made from granulocytes.16 MMPs are especially abundant when accompanied by a coinciding systemic or autoimmune disease that involves ocular tissue and exacerbates an inflammatory response.16 There is a greater upregulation of MMPs in corneal disorders where collagen is destroyed and MMP-2 and MMP-9 are widely present in patients who have corneal melts and recurrent corneal erosions. Signaling of IL-6 is then activated which induces the inflammatory response of the corneal stroma.17
Steroid drops can be used to control this cascade reaction by reducing inflammation, thus decreasing the amount of MMPs present in the tear film which then diminishes the trans-signaling of IL-6. Overall, when the tear film has a minimal amount of MMPs present, epithelial adherence to the basement membrane is greatly increased.
A Recurring DiagnosisThe initial evaluation is key, as is gaining the patient’s history of both the current episode and all prior ones. Since the erosions are a known diagnosis and are recurrent, it is important to re-examine the patient with a new perspective and capture any underlying conditions. Instilling a Fluress or proparacaine drop will help with the patient’s comfort while you examine them. The story of an RCE is usually easily predicted: frequent eye pain upon awakening, with accompanying photophobia and epiphora. The patient may also complain of conjunctival injection, blurred vision and difficulty keeping their eye open. If there is accompanying EBMD or DED, the complaints may also consist of asthenopia, fluctuating vision and burning, which more often occurs at the day’s end. Upon initial examination, staining with fluorescein may show a loss of epithelium, thus a positive epithelial defect, if the RCE is active. If the epithelial cells are healing by the time the patient appears for a visit, you may only see irregular epithelial cells in the place of the RCE, which can still cause irritation and discomfort. If there is a defect, it should be measured, as this is how the healing process is quantitatively assessed and tracked. Note whether it is a true defect with positive staining of fluorescein or rather, pooling of fluorescein. If it is pooling, the epithelial cells are intact; however, there may be stromal loss or a depression present, which causes the pooling. If unsure, use a dry cotton tip applicant to soak up the fluorescein; if no staining is seen, the epithelial cells are fully intact; however, if the area re-stains, an epithelial defect is present. Be sure to also note the amount of inflammation present: is there conjunctival injection only or are their stromal folds and inflammation underlying the epithelial defect as well? Are fine keratic precipitates visible with an anterior chamber reaction and is the upper lid showing erythema and edema as a protective reaction to the erosion? Pay attention to the size, shape and pattern of the eroded epithelium. Stained tracks among the corneal epithelium are an indication to evert the upper eyelid to check if a foreign body is present, which would change the diagnosis from a true RCE. If the patient has tried to endure the erosion without treatment for several days, more of an inflammatory response is expected. This also puts the patient at a higher risk for infection. Do not let an overabundance of inflammation steer you away from the proper initial course of action, and be certain to note any signs of infection, such as infiltrates or an ulcer, before proceeding with treatment, as this would drastically alter your course of treatment and management. |
Getting to the Root
ODs must address the underlying condition of the recurrent erosion, whether it’s previous trauma, EBMD or a form of chronic OSD (e.g., ocular rosacea, blepharitis, meibomian gland dystrophy, exposure keratitis).
Do not forget to examine the fellow eye closely, as some erosions can be thought to have only occurred from previous trauma when the patient actually has EBMD. This is an autosomal dominant condition where point mutations in the TGFBI gene on chromosome-5 are considered responsible for some erosions. EBMD can also be known as map-dot-fingerprint dystrophy, Cogan’s microcystic dystrophy or anterior basement membrane dystrophy. In this dystrophy, extra sheets of basement membrane extend abnormally into the epithelium. In turn, the epithelium growing anteriorly becomes entrapped in the extra sheets causing clumping and poor adherence.18 This can cause poor vision, constant discomfort and foreign body sensation, glare and halos, and of course recurrent corneal erosions. If there is previous anterior stromal haze or scarring from trauma or numerous erosions, the prognosis for a good outcome may decline. Often, if there is already corneal haze and scarring, the epithelium may not heal well. Likewise, if DED is a factor, the epithelial cells may regenerate at a slower rate, which increases the chance for the epithelium to break down and heal with residual anterior stromal haze or scarring.
In most cases, the RCE will continue to occur unless the underlying condition is managed and addressed. Moreover, there can be more than one etiology, as many times EBMD and DED are both collaborating factors in the recurrent erosions. Prescribing a dry eye drop such as Xiidra (lifitegrast, Shire) or Restasis (cyclosporine, Allergan), along with 2,000mg daily dose of omega-3 fatty acids will help reduce any unwarranted inflammation of the lid margin. Therapy can also include warm compresses with lid massage, artificial tears four to six times daily, and Muro 128 ointment at bedtime. If anterior blepharitis is diagnosed, lid hygiene will need to be discussed as well.
Avenova spray is a great tool for the lid margin, along with tea tree oil shampoo (for Demodex) or over-the-counter lid scrubs. For more severe cases, autologous serum can be prescribed, which is compounded from the patient’s own blood. The serum contains a mixture of growth factors and cytokines, similar to the human amniotic membranes, and should be kept cold at all times while being dosed every two hours while awake.19 Research shows that by addressing the DED, the incidence for recurrent erosions are significantly reduced.19
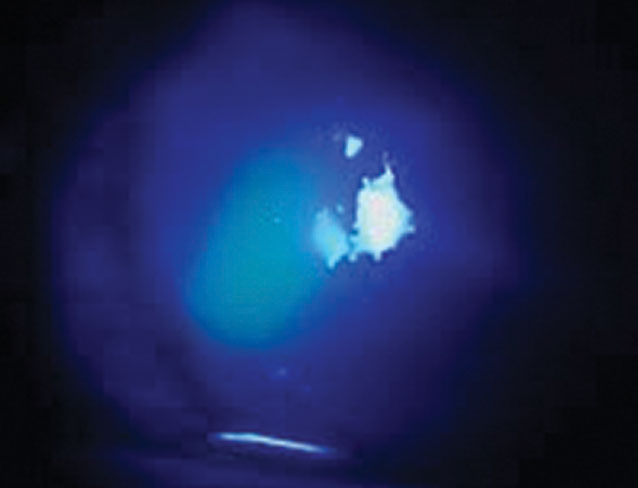 |
| This active RCE, seen with positive fluorescein staining, shows an epithelial defect nasally, measuring 1.5mm x 2.4mm. |
Lifestyle Changes
Patient education plays a large role in not only the healing of an RCE but also the prevention of one. The patient needs to understand that corneal erosions can be an ongoing issue and may not always have the best outcome if severe enough. Use the explanation that the surface skin cells of the cornea have sloughed off because they are loose and non-adherent; this creates a visual for the patient to better understand.
Once healed, it is important to prevent further episodes from occurring, which is why clinicians prescribe dry eye therapy, especially the ointment at bedtime. After the patient understands the importance of the prophylactic treatment, they are much more willing to be compliant.
The difficulty comes, however, when the patient does not heal well and has residual anterior stromal haze affecting the quality of the vision. Sometimes all that is needed is an updated spectacle or contact lens prescription or the use of a low-dose steroid for several weeks to minimize the haze. During the management of an RCE, if the patient is not healing well, starting the conversation early is beneficial, as their expectations will be realistic for the final visual outcome. Reassure them that you are applying every measure for a good outcome and stress the magnitude of the rigorous drop schedule. If the haze is severe, at times, a specialty contact lens such as a scleral or hybrid lens can help the patient gain better best-corrected vision. The quality of the tear film should never be taken for granted, as it can greatly enhance the vision, especially if there is residual haze; therefore, treatment for dry eye disease should be initiated.
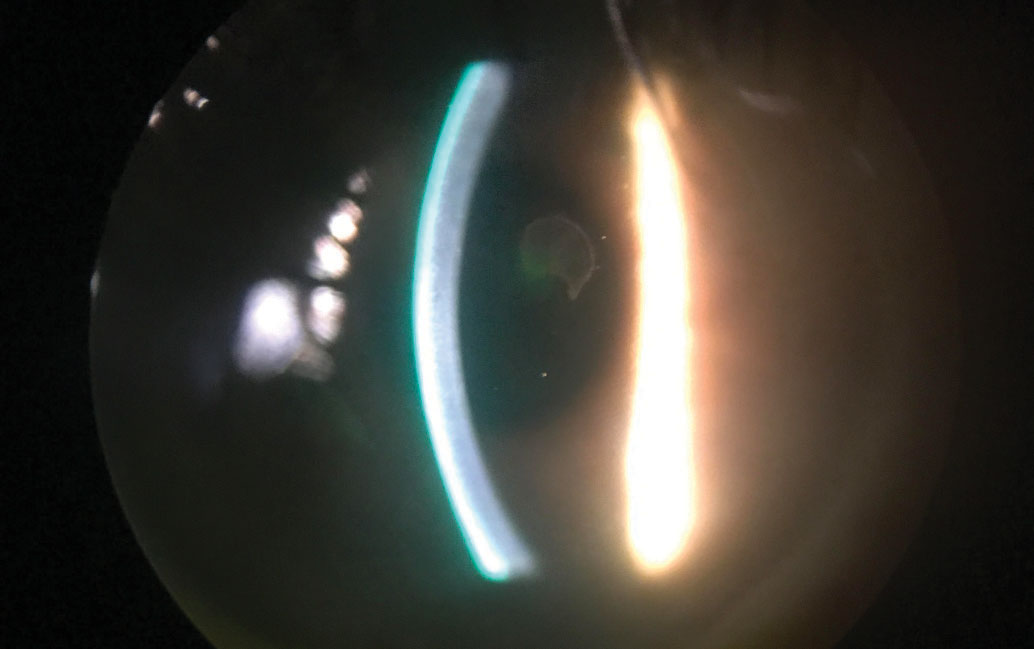 |
| This patient has a central epithelial defect with healing margins. It’s slightly difficult to discern whether it is a true defect without fluorescein staining. Click image to enlarge. |
Surgical Intervention
If the erosions continue and medical treatment fails, a surgical procedure may be necessary. Clinicians may need to coordinate with local corneal specialist; however, depending upon the procedure, some can be completed in-office.
Anterior stromal puncture (ASP) is a treatment that is useful for RCEs that occur in the peripheral cornea and can be done in the exam lane. Due to the risk of corneal scarring, it is not recommended when the erosion is central or mid-peripheral. Superficial punctures are made with a 25- or 27-gauge bent needle, piercing the epithelium to Bowman’s layer in 0.5mm spot treatments. This can also be done using a Nd: YAG laser, giving short bursts of energy to the cornea, which are more repeatable and shallower, thus diminishing the amount of scarring created than if by hand.19 In one review, ASP did have a recurrence rate of 40% and needed additional treatment.20
Epithelial debridement is also an in-office procedure that is commonly done, in which a Merocel spear and blunt spatula are used to remove the central 7mm to 10mm of loose, central epithelium.19 A bandage contact lens or an amniotic membrane can then be placed on the eye, along with the appropriate drop regimen; however, due to the high recurrence rate, this procedure is usually combined with extra steps.
Superficial keratectomy (SK) is an out-patient procedure, usually done in the operating room, in which the loose epithelial cells are removed with a Merocel spear, ensuring that the eye is not undertreated. This is then followed by treatment of the underlying basement membrane with a diamond burr which rejuvenates the membrane to allow strong, anchoring adhesions to the new epithelial cells when healing.21 After the SK, the postoperative care management in regards to lubrication and the BCL or amniotic membrane will be similar to the treatment and management for an RCE. The patient will also be on a soft steroid, antibiotic and NSAID taper schedule over several weeks.
Phototherapeutic keratectomy (PTK) is another common surgical option in which the epithelium is removed either by hand or an argon fluoride excimer laser. The laser is then used to emit ultrashort pulses of 193nm to ablate the irregular areas and opacities on a submicron level of Bowman’s layer and the outer 5µm to 7µm of the stroma, without damaging the middle stroma.22 This allows for the epithelium to regrow and form strong adhesions to the anterior stroma.19
PTK is widely used for corneal opacities, such as corneal scars, Salzmann’s nodular degeneration, recurrent erosions and EBMD. This procedure with the excimer laser removes enough of the superficial Bowman’s layer to allow formation of a new basement membrane with stronger adhesion structures.22 The postoperative care for PTK is the same as with SK.
It is important to keep all physicians caring for the patient (e.g., referring doctor, primary care physician, rheumatologist) informed of the diagnosis and treatment. Many underlying conditions can affect the health of the ocular surface, especially autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, or diabetes mellitus. If the patient has one of these medical conditions, they can be expected to heal slower and may need to be monitored more closely as it is not uncommon to hit a roadblock during the treatment process.
When writing a letter, be sure it is informative but succinct. It should include the diagnoses, treatment and management, as well as your concern for healing in relation to the patient’s systemic conditions. It is always beneficial to correspond with other physicians as this opens the path of friendly communication between colleagues, allowing them to know you can be a reliable referral source and have the patient’s best interest in mind.
Other considerations to keep in mind are any systemic medications that the patient may already be taking that could inhibit the healing process of the erosion. Medications such as antihistamines, anticholinergics or anxiolytics and antidepressants are commonly prescribed and cause extra overall dryness, as well as ocular surface dryness and irritation. Be sure to view the entire picture and recognize what treatment is best suited for that particular patient.
Recurrent corneal erosions are common and are something that we, as clinicians, can treat and manage. There are many treatment options from over-the-counter ointments to prescription drops and oral medication, from bandage contact lenses to human amniotic membranes, as well as many environmental additions that can all help in the healing of RCEs.
Dr. Finch Crouch is an optometrist at Eye Centers in Louisville, Kentucky.
1. Highlights of Prescribing Information: Besivance. www.accessdata.fda.gov/drugsatfda_docs/label/2009/022308lbl.pdf. April 2009. Accessed March 11, 2019. 2. Ness P, Mamalis N, Werner L, et al. an anterior chamber toxicity study evaluation Besivance, AsaSite, and Ciprofloxacin. Am J Opthalmol. 2010;150(4):498-504. 3. Opitz D, Harthan J. Review of azithromycin ophthalmic 1% solution (Azazite) for the treatment of ocular infections. Ophthalmology and Eye Diseases. 2012:4(2):1-14. 4. Goecks T, Werner L, Mamalis N, et al. Toxicity comparison of intraocular azithromycin with and without a bioadhesive delivery system in rabbit eyes. J Cataract Refract Surg. 2012;38(1):137-45. 5. Wang L, Tsang H, Coroneo M. Treatment of corneal erosion syndrome using the combination of oral doxycycline and topical corticosteroid. Clinical and Experimental Ophthalmol. 2008;36(1):8-12. 6. Smith V, Cook, S. Doxycycline – a role in ocular surface repair. Br J Ophthalmol. 2004;88(5):619-25. 7. Buglisi J, Knoop K, Levsky M, Euwema M. Experience with bandage contact lenses for the treatment of corneal abrasions in a combat environment. Military Medicine. 2007;172(4):411-13. 8. Huang Y, Sheha H, Tseng S. Self-retained amniotic membrane tranplantation for recurrent corneal erosion. J Clin Exp Ophthalmol. 2013;4:272. 9. Shimmura S, Shimazaki J, Ohashi Y, Tsubota K. Antiinflammatory effects of amniotic membrane transplantation in ocular surface disorders. Cornea. 20(4):408-13. 1 May 2001. 10. Cook M, Tan E, Mandrycky C. Comparison of cryopreserved amniotic membrane and umbilical cord tissue with dehydrated amniotic membrane/chorion tissue. J Wound Care. 2014;23(10):465-74. 11. John T, Tighe S, Sheha H, et al. Corneal nerve regeneration after self-retained cryopreserved amniotic membrane in dry eye disease. J Ophthalmol. 2017:640498. 12. Werner S, Gross R. Regulation of wound healing by growth factors and cytokines. Physiological Reviews. 2003;83(3):835-70. 13. Liu J, Sheha H, Fu Y, et al. Update on amniotic membrane transplantation. Expert Rev Ophthalmol. 2010;5(5):645-61. 14. Koob T, Lim J, Zabek N, Massee M. Cytokines in single layer amnion allografts compared to multilayer amnion/chorion allografts for wound healing. J Biomed Mater Res Part B. 2015;103(5):1133-40. 15. Fraunfelder F, Cabezas M. Treatment of recurrent corneal erosion by extended-wear bandage contact lens. Cornea. 2011;30(2):164-66. 16. Smith V, Rishmawi H, Hussein H, Easty D. Tear film MMP accumulation and corneal disease. Br J Ophthalmol. 2001;85(2):147-53. 17. Sakimoto T, Sawa M. Metalloproteinases in corneal diseases: degradation and processing. Cornea. 2012;31(Suppl1):S50-6. 18. Edell E, Bernfeld E, Woodward M, Bunya V. Epithelial basement membrane dystrophy. American Academy of Ophthalmology. eyewiki.aao.org/Epithelial_basement_membrane_dystrophy. February 17, 2017. Accessed March 1, 2019. 19. Miller D, Hasan S, Simmons N, Stewart M. Recurrent corneal erosion: a comprehensive review. Clinical Ophthalmology. 2019;13(2):325-35. 20. Reidy J, Paulus M, Gona S. Recurrent erosions of the cornea: epidemiology and treatment. Cornea. 2000;19(6):767-71. 21. Piracha A. The benefits of pre-treating corneas. Review of Ophthalmol. 2010;16(4). 22. Garg S, McColgin A, Steinert R. Phototherapeutic Keratectomy. American Academy of Ophthalmology. www.aao.org/munnerlyn-laser-surgery-center/phototherapeutic-keratectomy-3. November 12, 2013. Accessed March 12, 2019. |

