Get a Head Start on Specialty Contact LensesIn the August 2024 issue of Review of Optometry—our 48th annual Contact Lens report—experts provide the tips and tools you need to start offering specialty lenses at your practice. In two more features, the authors deep-dive into soft lens optics and CL complications. Check out the other articles featured in this issue:
|
When considering new services to incorporate into an optometric practice, specialty contact lenses (CLs) have certainly been one of the most implemented, as this niche matches our refractive skillsets very well. For many practitioners, adding specialty CL services can create a new focal point, making their practice stand out with a new category of patients whose vision was otherwise considered “just the way it is.” By providing custom lens fits to these patients, it can indeed widen the potential of what specialty lenses can offer—not simply for vision, but also to enhance quality of life.
As with many specialty fields, the implementation of custom CLs does not take off on its own organically; rather, it requires strategic planning fueled with passion and commitment in advocating these services to patients. Here are several key aspects for which you can build a specialty lens service and make it thrive in your practice.
Know Where the Heart Belongs
To get started with specialty CLs, you first need to feel passionate about it. Read as much as you can from journals and periodicals to get familiar with the technology and products. Attend conferences such as Global Specialty Lens Symposium, International Congress of Scleral Contact Lenses, Optometry’s Meeting, American Academy of Optometry, Vision by Design (by the American Academy of Orthokeratology and Myopia Control) as well as the International Keratoconus Academy. State and local optometric societies also provide valuable in-person education. Participating in hands-on workshops can be incredibly helpful in meeting with the various contact lens and equipment companies, along with the ability to network with colleagues and find a mentor or two to assist you in this journey.
 |
|
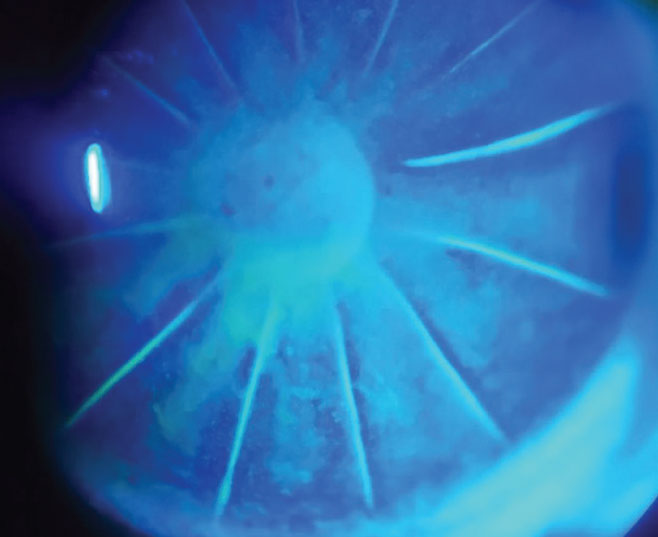
Slit lamp image of a patient status post radial keratotomy. Click image to enlarge. |
You will find that those of us in the specialty CL community are very welcoming and resourceful in helping beginning practitioners succeed. Residents or practitioners can also ask to visit some practices and shadow a more experienced colleague to observe their exam flow, see some patients and engage in a wet-lab setting. This happens quite frequently in our offices.
Online education has certainly flourished over the past few years. Organizations such as the Scleral Lens Education Society and the Gas Permeable Lens Institute have an abundance of online resources and provide monthly online webinars to expand your knowledge. These organizations also have in-person events and workshops to further your clinical acumen and experience. Many online CE providers also provide virtual courses such as Woo University, Eyes on Eyecare and CE Wire throughout the year, both on contact lenses and cornea/anterior segment conditions.
Know Your Audience
Familiarity with your patient base and how to cater specialty lens services to different patient demographics is key. Simply talking about specialty lenses without the context of why for patients is like selling a Cadillac to a teenager without a driver’s license. Be sure to impart to your patients that the virtues of specialty contact lenses go beyond just the core aspect of vision correction—what makes specialty lenses “special” is their therapeutic potential for patients of all ages.
 |
|
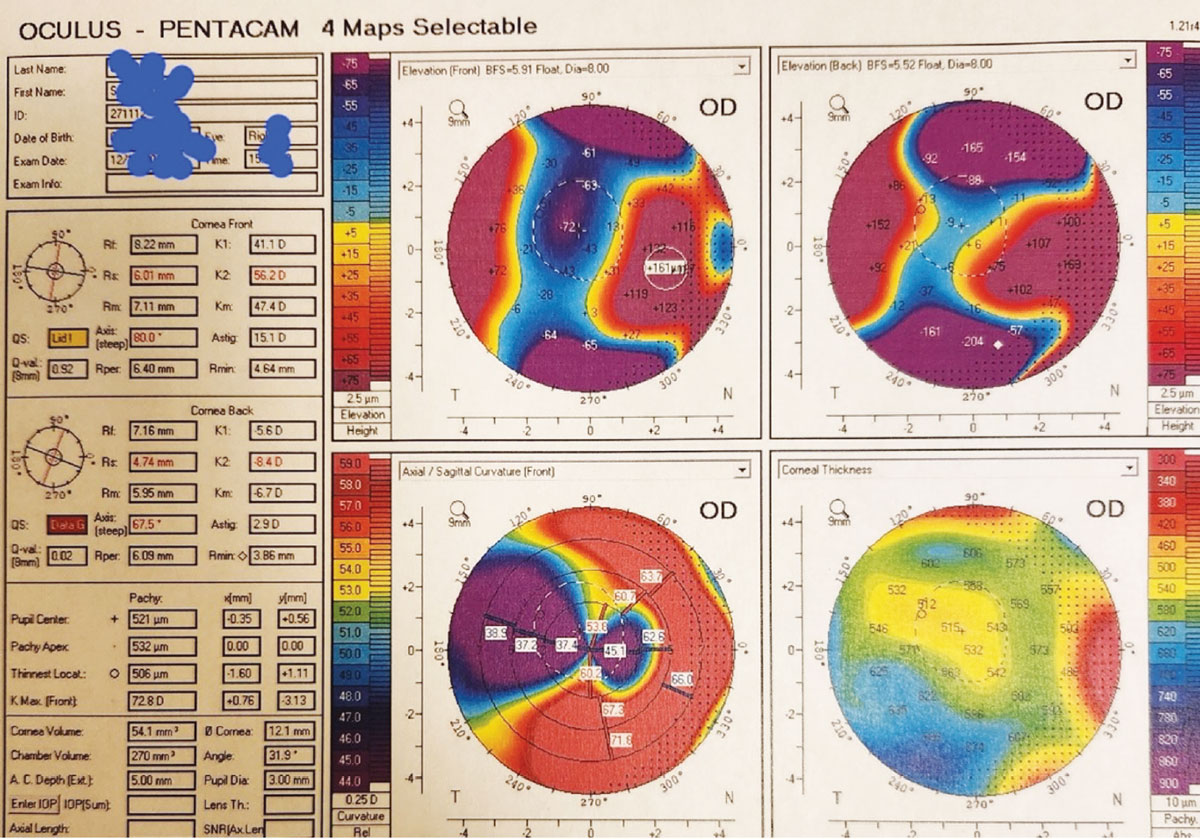
Topography image of a patient with severe irregular astigmatism post-PK. Click image to enlarge. |
For children, orthokeratology (ortho-K) is one of the most effective yet underrated rigid gas permeable (GP) lens modalities in the specialty lens toolbox.1 By using a reverse geometric design, ortho-K lenses can uniquely reshape the corneal contour for patients while sleeping. With the prevalence of childhood myopia accelerating, most ortho-K lenses have been specifically designed for myopia management, and this is the type most young patients are prescribed.2 In comparison with conventional spectacles and single vision contact lenses, what makes ortho-K a unique experience for children and their parents is that an ortho-K lens isn’t just a vision correction device—it can help them achieve independence in many daily activities or functions. Moreover, it can unlock possibilities they could hardly imagine with their current vision correction.
 |
|
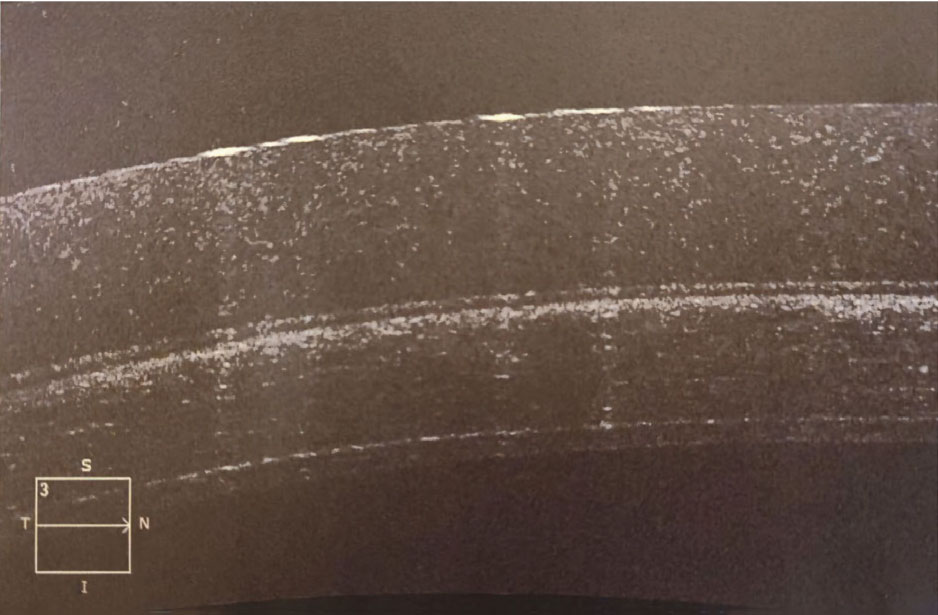
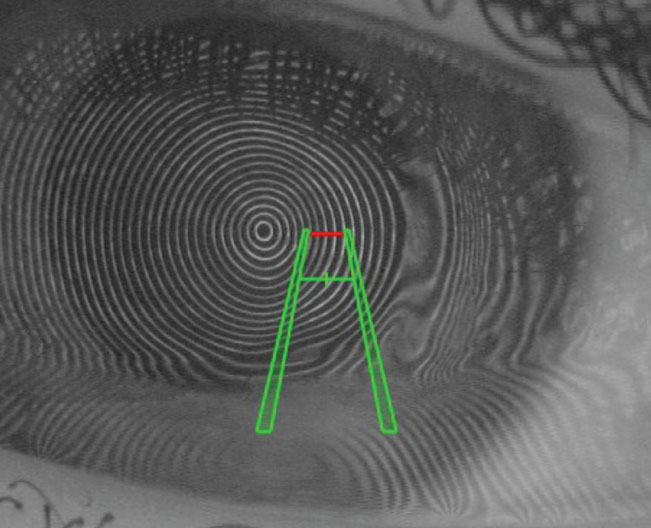
Anterior segment OCT of a specialty soft keratoconus contact lens on the eye demonstrating the thickness of the lens. Click image to enlarge. |
To achieve optimal distance clarity for patients with myopia, the central cornea is flattened based on the patient’s refractive error along with a compression factor (typically +0.50D by default) to allow clear and lasting unaided vision during daytime hours. Fascinatingly, robust clinical data shows that optic zone sizes and higher-order aberrations (HOAs) play emerging roles in slowing axial length progression in children.3-6 When optic zone was reduced, some studies showed that it positively correlated with the mid-peripheral steepening effect on the cornea, thereby yielding a greater amount of relative peripheral refraction generated. Nevertheless, it is important to note that this outcome is not universal, as large pupil size has been shown to increase the exposure of peripheral defocus signals as well, thereby halting greater axial length elongation.
The ortho-K outcome can also be subject to change based on patient’s age, level of myopia and other behavioral factors. HOAs, notably spherical aberration, have demonstrated clinically significant benefits in slowing axial length progression.5 While the exact mechanism is yet inconclusive, some theories suggest that HOAs are closely associated with peripheral defocus, which can directly impact the retinal image quality. Interestingly, the human retina appears to respond to and interpret retinal blur as a positive “go” signal that can help reduce axial length growth.
 |
|
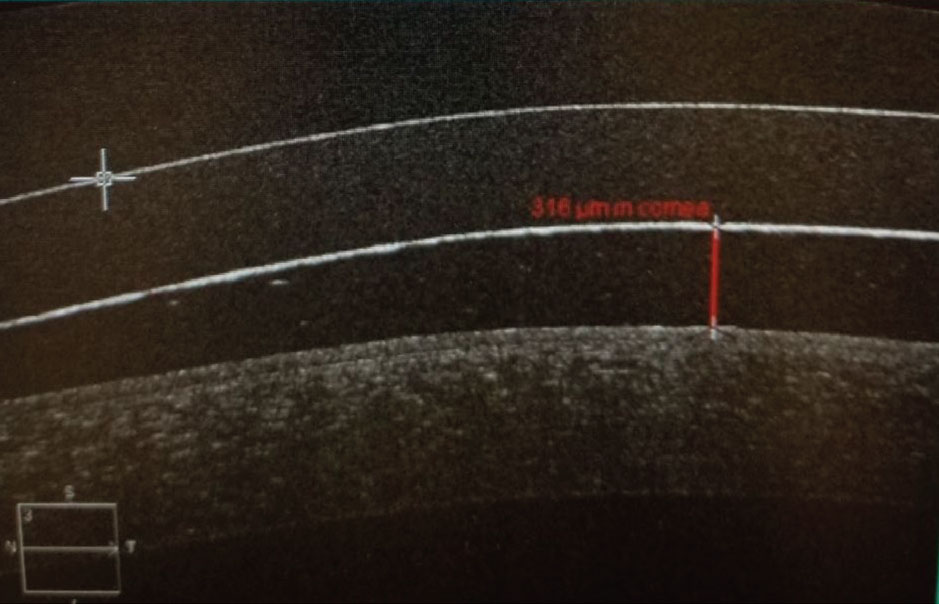
OCT image of a scleral lens evaluating lens vault over the cornea. Click image to enlarge. |
However, the use of ortho-K lenses is not limited to children or adults with myopia. Patients with astigmatism, hyperopia or those reaching presbyopic age who are in need of reading glasses may also be eligible for ortho-K lens wear for full distance correction or modified monovision. With the versatility of corneal remolding techniques by ortho-K, we fully believe and live by the ‘no-one-size-fits-all’ principle. By that nature, it truly encompasses the ability to indeed alter corneal shapes the way intended and, therefore, help patients achieve their desired vision for their lifestyles.
As an example, an eight-year-old child with progressive myopia would benefit from an ortho-K lens design with a distinct and uniform mid-peripheral steepening effect (also known as the bull’s-eye red ring) combined with a relatively small back optic zone size; this design will yield a greater level of myopic defocus signals and HOAs. To illustrate ortho-K’s versatility, consider also a 50-year-old patient who has been emmetropic all her life and is now emerging as a presbyope. She started experiencing reading difficulties at work as an accountant while also suffering from chronic dry eye symptoms and wanted to be more independent of glasses or contact lenses. Use of a hyperopic ortho-K lens design (i.e., central steepening and mid-peripheral flattening) with a modified monovision approach could help fulfill her unique vision needs. Offering this approach in turn will build loyalty.
 |
|
Image of a scleral lens on a post corneal transplant eye. Click image to enlarge. |
In our collective clinical experience, success and patient loyalty are not built solely by following monetary incentives. Rather, it is the journey of the specialty lens experience you provide that makes an overwhelmingly positive or even a life-changing outcome for patients that will foster trust and support. Doing well with specialty CLs isn’t simply about the science of the lenses; listening to your patients’ visual needs and helping them achieve their treatment goals is the art of mastering specialty lenses for all patients.
 |
|
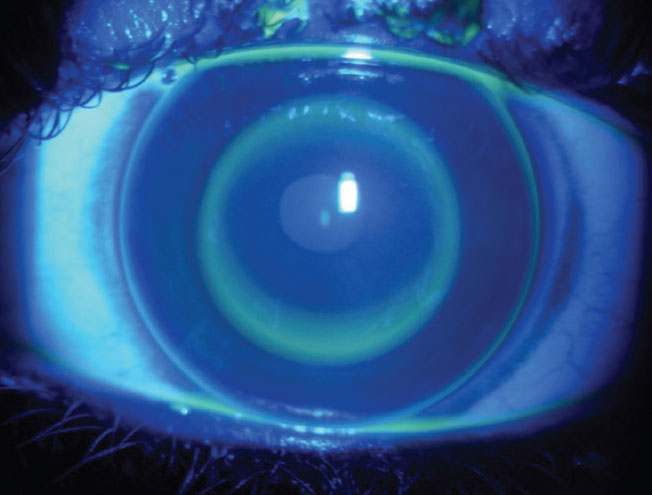
Demonstration of scleral lens vault using fluorescein dye. Click image to enlarge. |
Knowledge and Relationship with Lab Manufacturers
Many laboratories provide in-office wet labs and consultation. During the early phase of the learning process, lab consultants are great assets in guiding practitioners to navigate the roadmap of lens design and offer troubleshooting advice. Make sure your laboratory has a robust return policy, as you will need to make more lens changes at the beginning. Choose lens designs that allow the ability to customize lens parameters. Also be aware of added charges for lens customization, lens exchange fees as well as shipping costs when deciding on contact lens laboratories that you would like to partner with. Labs are also useful in providing patient education material.
The process of becoming an astute clinician with specialty lenses takes time and effort to feel comfortable in diagnosing and managing anterior segment complications that frequently occur when taking care of complex eyes. Keratoconus is the most prominent corneal disease requiring specialty contact lenses, but other conditions such as corneal dystrophies, corneal scarring, corneal transplants, irregular astigmatism and ocular surface disease also are a major part of specialty lens practice, so choosing your partnered laboratory should work for what kind of patients you will see.
 |
|
Placido disc corneal topography seen from a patient’s bird eye view. Placido disc evaluation is valuable in assessing the corneal contour and the quality of ocular surface. It can guide the selection of specialty CL design. Click image to enlarge. |
Lens Types
A specialty CL-driven practice also needs to offer multiple contact lens modalities. Scleral lenses are rightfully positioned as the primary option for most patients, but other options, including custom soft lenses, corneal GP lenses and hybrid lenses, are integral parts of a complete specialty CL practice. A subset of a specialty lens practice is prosthetic lenses for disfigured eyes and for functional needs. You should consider the patient’s needs, clinical findings, previous contact lens experience, eye anatomy, dexterity and finances to prescribe the appropriate lens modality and provide the best care for your patients.
 |
|
Decentration and distortion of mires in a corneal topography in vivo. Angle kappa should be considered. Guiding patients to blink and turning their heads contralateral to the eye measured helps address the issue. Click image to enlarge. |
When considering scleral lenses for patients with presbyopia, practitioners can sometimes be too focused on making a perfect fit, owing to the weight carried by the term ‘specialty contact lens.’ While it is certainly a vital factor to achieve successful clinical outcomes, it is also key to keeping patients informed and discussing with them what they want to achieve in daily life. They should also be cognizant of other possible scenarios for which patients’ expectations may warrant adjustment or alignment. For example, what is the patient’s occupation—are they a truck driver or computer engineer? What priority in life does the patient have? Does the patient mind compromising a bit of clarity at distance in exchange for more independence from reading glasses? All these questions merit further consideration when it comes to prescribing scleral lenses for patients with presbyopia.
Hybrid lenses can be used in patients with very discerning vision requirements as they provide crisp vision and comfort with the GP center and soft skirt combination. They are available as single vision, extended depth-of-focus and multifocal optics along with a version geared for the irregular cornea. Most hybrid lenses exist as six-month replacements. When used effectively, these lenses can distinguish you from other providers, as they are only available from doctor’s offices.
 |
|
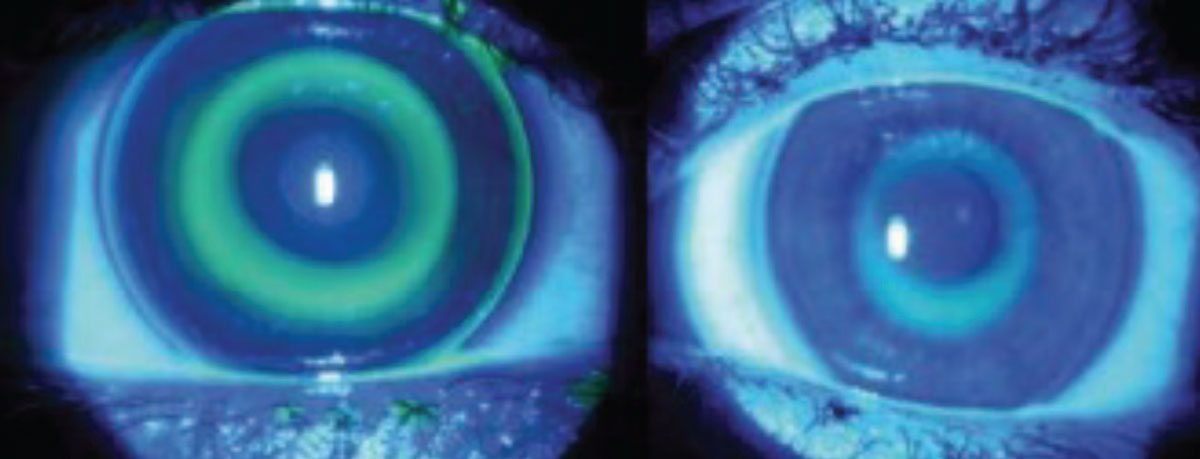
Optimal NaFl distribution for an orthokeratology lens fit in a young adult. Relatively larger back optic zone diameter can be considered to optimize the clarity of distance vision. Click image to enlarge. |
Cosmetic lenses are commonly perceived as multicolor lenses for appeal. However, cosmetic colored lenses have been documented in use for occlusion therapy to ameliorate migraine, photophobia—particularly for patients with iris atrophy or ocular albinism—diplopia as well as amblyopia.7
Get to Know Your Gadgets
Corneal topography and tomography have increasingly become indispensable tools with which to excel in specialty lens care. As easy as it seems to use these technologies, though, they are not necessarily recognized for their versatile functionality. We’ll break it down and explore the nuances of how to maximize the utility of these devices.
First, you need to invest in your practice. A slit lamp biomicroscope and fluorescein dye are all that is technically required to evaluate a contact lens; however, to provide the most up-to-date care, upgrading to an anterior segment OCT (AS-OCT) will allow for more precise on-eye lens analysis. We find AS-OCT helpful when troubleshooting and would recommend it for those new to specialty lens care, as it reinforces what you are seeing with the slit lamp. Having slit lamp imaging from a phone or camera adapter and AS-OCT images to transmit to laboratories can be very helpful when needing to make changes to lens parameters, following anterior segment conditions and for patient education.
 |
|
Comparison of the back optic zone diameter (BOZD) between 6.0mm and 4.8mm. Selection of a relatively smaller BOZD for children has shown to augment the amount of peripheral defocus signaling, which is believed to help slow axial length progression. Click image to enlarge. |
Topography, and preferably tomography, is important in diagnosing and managing corneal conditions. These technologies also give you valuable insight into the shape and corneal contour to assist you in designing your contact lenses, such as prolate vs. oblate shape, horizontal visible iris diameter (HVID) and corneal eccentricity. Specular microscopy instruments are important in diagnosing and following patients with endothelial disease and corneal transplants. Evaluating endothelial cell counts and viability of endothelial cells can help you determine the most appropriate CL modality or whether to refer for corneal endothelial surgical interventions, such as posterior lamellar surgery, that can address both Descemet’s membrane and endothelial deficit when indicated.
 |
|
Optimal NaFl distribution for an ortho-K lens fit in a child. Note that the mid-peripheral ring with NaFl pooling is designed to be more coincided with the pupillary margin to optimize the projected mid-peripheral defocus signal compared to the fit for young adults. Click image to enlarge. |
Corneoscleral imaging devices, collectively known as scleral profilometers, are great tools to possess and have become a vital part of specialty lens practice. It benefits clinicians to better understand scleral shape, which aids in designing specific types of specialty CLs, such as scleral and ortho-K lenses. In addition, aberrometry is emerging as yet another technological advancement to incorporate HOA correction in our lenses for those patients that require higher quality vision not possible with standard scleral lens optics.
Corneal Topography
Capturing good corneal topographic images gets you halfway to successful outcomes. Essentially, it is just like building a solid foundation when making a cake. While any topography can provide practitioners a general overview of the corneal contour, it is fundamentally crucial to minimize visual interferences by the lid apertures.
Gently holding patient’s upper and lower lids manually without pressing against the conjunctiva or soft orbital tissues during the capture of topographical images can accurately yield full exposure of the limbal-to-limbal aperture to help determine the lens diameter for any type of specialty lenses. In general, ortho-K lens diameter is approximately 0.5mm to 0.8mm smaller than the HVID. The average diameter ranges from 10.6mm to 11.0mm in most cases. At times, though, it can be customized as a trans-limbal design with a diameter beyond the limbus (greater than 11.5mm) for atypical corneal toricity or induced astigmatism to optimize lens stability and comfort.8
The use of corneal topography extends beyond the realm of GP and ortho-K lenses. When fitting multifocal or custom soft lenses, it has been customary for practitioners to have patients wear a trial pair and evaluate the overall fit in the slit lamp. While it is an essential step to assess lens movement, lens-lid interaction and fluid exchange underneath the lenses, what we can do to take this assessment a step further is to evaluate multifocal or custom soft lenses via corneal topographical imaging in vivo. After a trial lens is placed onto the patient’s eyes, wait for a minute and capture serial corneal topographical images. It can provide you four key pieces of information: distribution of multifocality, centration of multifocality in reference to the visual axis, neutralization of toricity and power distribution vs. baseline via comparison maps. All this information (though not exclusive to those mentioned) can be tremendously helpful in guiding whether a revision should be made and how it should be made. Moreover, it can help guide when to fit patients with decentered pupils for a custom decentered optical multifocal design, as compared with commercially available multifocal soft lenses.
 |
|
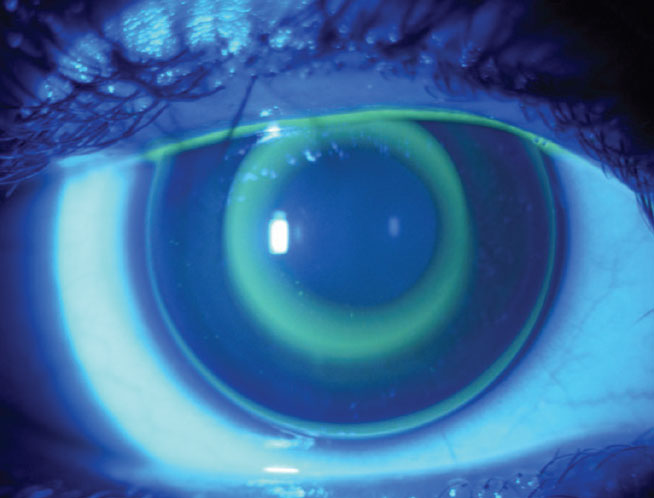
An overview of a four-map comparison depicting keratometry, pachymetry, anterior and posterior elevation. Click image to enlarge. |
OCT
The use of OCT has become increasingly more prevalent in the realm of scleral lens fitting and troubleshooting. Thorough knowledge of how the central and peripheral cornea changes in response to keratoconus and its progression can be useful in understanding how limbal clearance on the sclera should be accommodated in a scleral troubleshooting regimen.9
The advent of OCT can also be applied to measure the sagittal depth of the eye, which can help guide practitioners to determine patient candidacy for a commercially available soft CL or custom soft lens. While seemingly unconventional, studies found that soft lenses behave and interact with the eyes differently despite having the same base curves and in conditions with various temperatures.10,11 The differences in sagittal depth values among various spherical and toric lens designs help practitioners recognize how to account for each lens design based on its unique characteristics and make adjustments accordingly.
 |
|
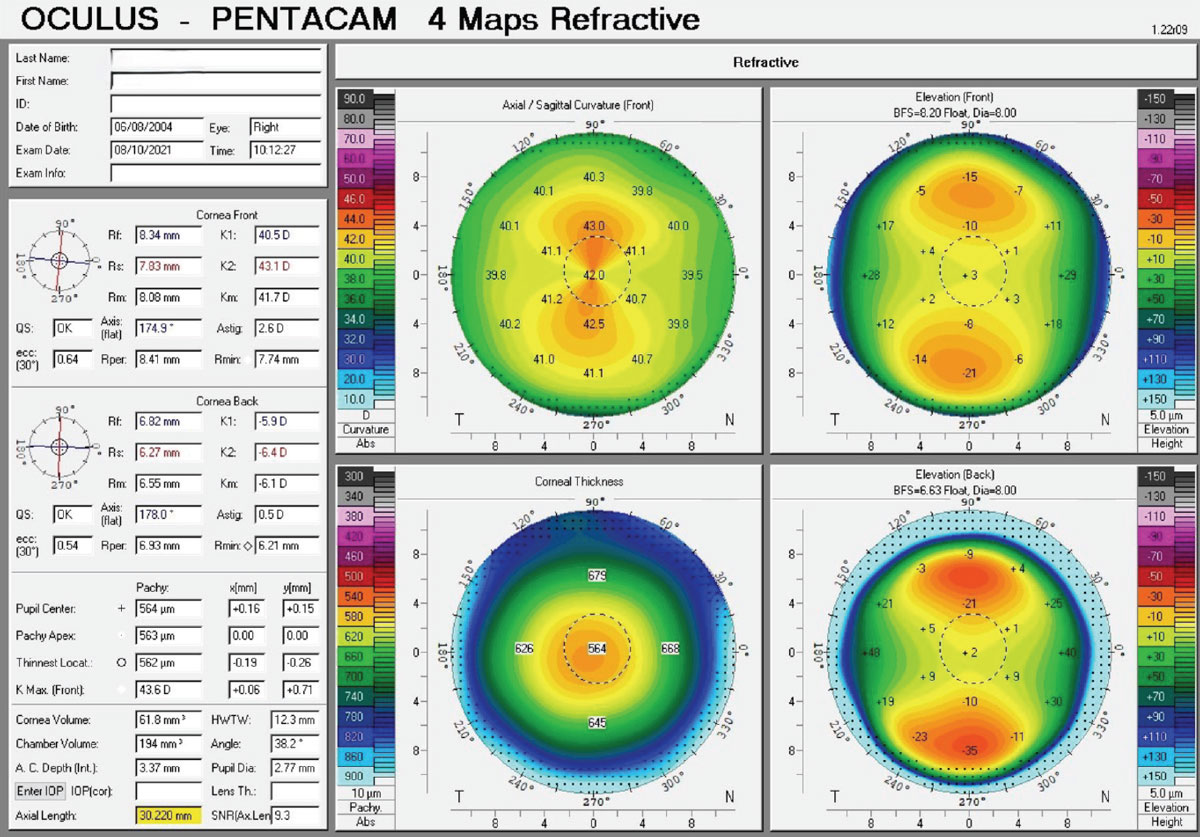
An overview of a two-map tangential comparison between the baseline and the treatment phase, showing the overall centration effect and axial length status. Click image to enlarge. |
Office Logistics and Billing
In addition to technological and scientific considerations, staff too plays a vital role in the success of a specialty CL practice. Staff should be kept up-to-date on lens technology, testing and care. They need to be thorough in lens ordering, lens processing, schedule logistics as well as lens exchanges and to reconcile invoices and monthly statements. Being comfortable with lens application and removal training and lens care products is paramount. They are not simply your technicians; they should possess personalities amenable to engaging with patients who may warrant advanced assessments, follow-up visits and guidance for lens care regimens. We give our patients samples of all products and provide them with a handout about lens care and where to purchase additional lens care solutions. A laminated card with application and removal instructions is also given at the contact lens dispense visit. Lens care is reinforced at every CL progress visit.
Make sure that your front desk support staff also stay abreast on the nuances of specialty CL services you provide in your office. Your staff should be confident and able to answer basic questions about specialty lenses and the services offered. Update your website to highlight these services so patients are aware and come prepared with questions prior to consultation.
 |
|
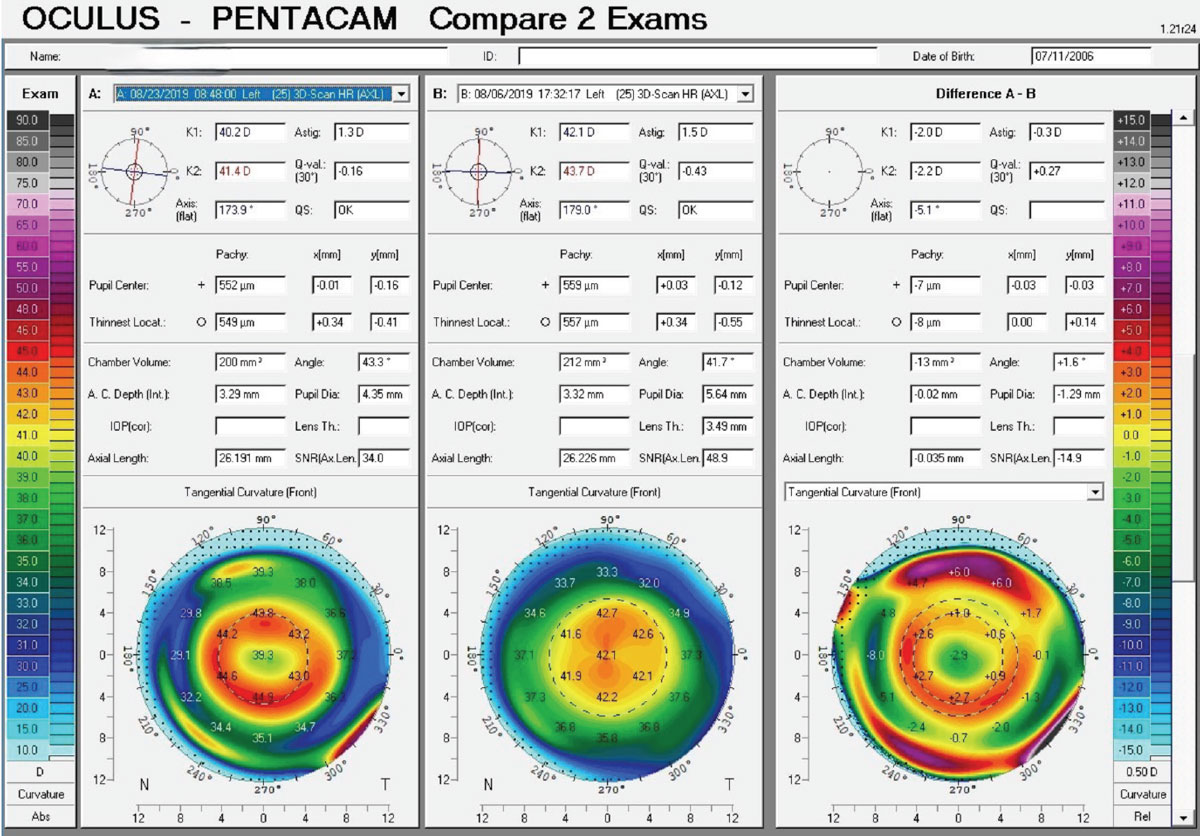
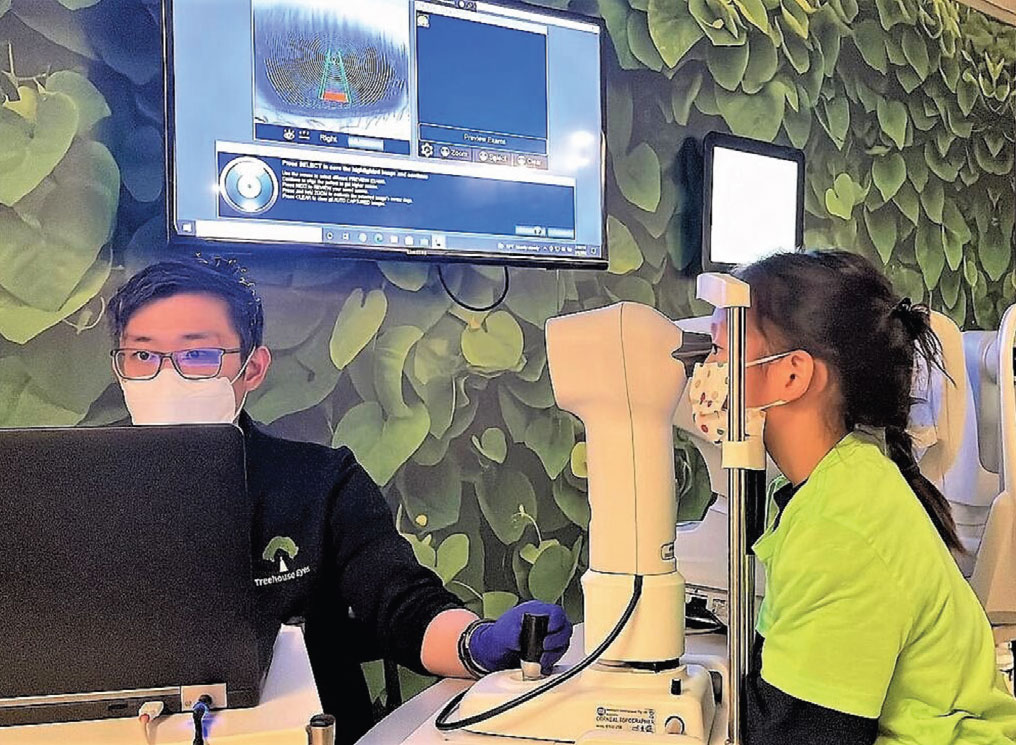
This child is having a corneal topography scan performed at an interim follow-up visit. Click image to enlarge. |
At times, specialty lenses can be tricky and challenging with billing and coding. Rules and regulations frequently change, so keep up-to-date on individual medical and vision care plans if you participate with them. Read your provider manuals very carefully as well as the agreement documents that you have signed.
It is essential to be transparent with patients regarding billing and payment policies. Also be comfortable with medical billing and coding, as this is critical to avoid trouble down the line and to, of course, maximize payment. Document everything in writing and provide patients with a signed copy prior to commencing the lens fitting process. Spell out all of your policies including returns, cancelation of the fitting process or switching lens modalities. Be cognizant of the warranty period and make the patient aware of this as well.
Referral Network
One of the main sources of patients to specialty CL practices are referrals from ophthalmology, optometry and other medical specialties; most eyecare practitioners do not provide specialty lens services in their practice. It is important to offer many different modalities and options to patients. Corneal GP lenses particularly are becoming less and less a part of most optometry practices. Corneal GP lenses uniquely provide many advantages compared with other CL types, including vision benefits, ease of insertion and removal, less costly lens care, typically lower cost to both provider and patient and excellent corneal physiology.
In our respective practices, we often arrange lunch-and-learn seminars and share about specialty CL services with other medical professionals. It creates great networking opportunities with people in other multidisciplinary settings and build the referral network. With the strong referral network, it helps distinguish us in our geographic regions and beyond to provide these services.
 |
|
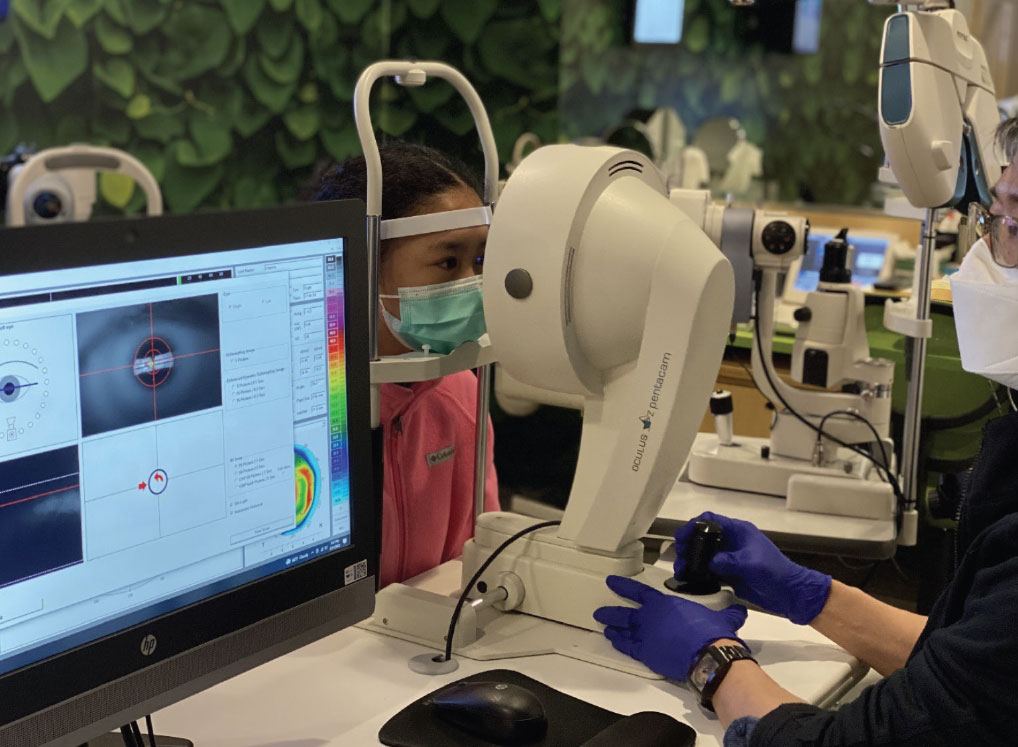
Another child was seen having a corneal tomography to reveal the anterior and posterior corneal status upon fitting with ortho-K lenses. Click image to enlarge. |
Takeaways
One of the greatest merits provided by specialty contact lenses is that they truly impact patients’ lives. To provide the best care for your patients, it requires a combination of knowledge, learning aptitude and dedication on your part. You do need to have a passion for specialty CLs to thrive. While they are seemingly categorized as simply “contact lenses,” they are also key, life-changing investments for which you have to be willing and motivated to dive into should you aim to make it impactful for patients while profitable for your practice. For that, practitioners should stay familiar with lens costs and chair costs. If you are losing the ROI doing specialty lenses, you will lose interest and footing very quickly. If you stay on top of it, treating these patients can be both humbling and rewarding with great returns.
Dr. Chan is the senior clinical director of Treehouse Eyes. He was the recipient of the Global Specialty Lens Symposium 2024 Rising Star Award in recognition of his leading role in cornea and contact lenses and was also named a Healio honoree in 2023. He lectures nationally and internationally about contact lenses and myopia management and presented the TEDx talk, ‘Myopia–Global Epidemic.’ He is a Fellow of the American Academy of Optometry and earned the International Academy Certification in Myopia Management. He serves as a Professional Affairs Consultant for Johnson & Johnson Vision and Essilor’s Myopia Taskforce. Financial disclosures include Euclid Vision Corporation, Topcon Healthcare, PECAA and Conexiant.
Dr. Sorkin is director of specialty contact lens services at Corneal Associates of New Jersey. He lectures nationally and internationally on contact lenses, ocular therapeutics and corneal disease. He serves as president of the Essex County Optometric Society and serves as a member of the board of directors of the New Jersey Society of Optometric Physicians (NJSOP), also serving as a member of the medical advisory board of the International Keratoconus Academy (IKA). He is a Fellow of the Scleral Lens Education Society (SLES) and is adjunct clinical faculty at Salus University and the New England College of Optometry. He was named New Jersey Optometrist of the Year in 2018 by NJSOP. Financial disclosures include Avellino, Bausch + Lomb SVP, BostonSight, Dompé, the IKA, Santen, the SLES and Tarsus.
1. Vincent SJ, Cho P, Chan KY, et al. CLEAR-orthokeratology. Cont Lens Anterior Eye. 2021;44(2):240-69. 2. Xiang ZY, Zou HD. Recent epidemiology study data of myopia. J Ophthalmol. 2020;2020:4395278. 3. Li X, Zuo L, Zhao H, et al. Efficacy of small back optic zone design on myopia control for corneal refractive therapy (CRT): a one-year prospective cohort study. Eye Vis (Lond). 2023;10(1):47. 4. Guo B, Cheung SW, Kojima R, Cho P. Variation of Orthokeratology Lens Treatment Zone (VOLTZ) study: a two-year randomized clinical trial. Ophthalmic Physiol Opt. 2023;43(6):1449-61. 5. Lau JK, Vincent SJ, Cheung SW, Cho P. The influence of orthokeratology compression factor on ocular higher-order aberrations. Clin Exp Optom. 2020;103(1):123-8. 6. Lau JK, Vincent SJ, Cheung SW, Cho P. Higher-order aberrations and axial elongation in myopic children treated with orthokeratology. Invest Ophthalmol Vis Sci. 2020;61(2):22. 7. Collins RS, McChesney ME, McCluer CA, Schatz MP. Occlusion properties of prosthetic contact lenses for the treatment of amblyopia. J AAPOS. 2008;12(6):565-8. 8. Huang R. Fitting trans-limbal ortho-K to prevent ptosis-induced astigmatism. Contact Lens Spectrum. www.clspectrum.com/supplements/2023/scleral-and-specialty-contact-lens-case-reports/fitting-trans-limbal-ortho-k-to-prevent-ptosis-induced-astigmatism. Published October 1, 2023. Accessed June 1, 2024. 9. Mas-Aixala E, Gispets J, Lupón N, Cardona G. The variability of corneal and anterior segment parameters in keratoconus. Cont Lens Anterior Eye. 2016;39(6):466-70. 10. van der Worp E, Lampa M, Kinoshita B, et al. Variation in sag values in daily disposable, reusable and toric soft contact lenses. Cont Lens Anterior Eye. 2021;44(6):101386. 11. Fujimoto MJ, van der Worp E, Kinoshita B, et al. Daily disposable soft lens sagittal depth and other lens parameter changes measured at room temperature (20 °C) and on-eye temperature (34 °C). Cont Lens Anterior Eye. 2024;47(3):102160. |

