A 3-year-old white male presented with his parents for an eye exam. His parents were concerned about their childs vision. They said that he can recognize objects and smiles at the face of a parent, but he seems to hold objects extremely close. They also said his eyes always shake; this began at about age 3 months.

The patients medical history is unremarkable. The child is fair skinned, more so than the parents but not excessively so. He has blond hair and light-colored eyes. He is an only child and according to the parents, there does not seem to be a family history of this condition.
Visual acuity measured 20/200 O.U. at distance with familiar figures and about 20/80 O.U. at near. Extraocular motility testing revealed horizontal nystagmus in all gazes. He does not display a head-turn, nor does he have a noticeable null point. There is a latent component when either eye is covered.
We were able to reverse his nystagmus on optokinetic (OKN) testing and were able to superimpose the OKN overtop of his nystagmus. His range of motion is full, and he does not have strabismus. The pupils were equally round and reactive, and there was no afferent pupillary defect. Cycloplegic retinoscopy was +2.00D in each eye. The anterior segment exam was essentially unremarkable.
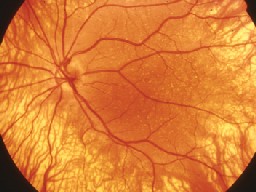
Dilated fundus exam revealed an obvious lack of pigmentation within the retinal pigment epithelium (RPE). The choroidal vessels and sclera were easily seen. Other significant findings are shown in the photos.
Dilated fundus exam (O.D. left, O.S. right) revealed an obvious lack of pigment in the RPE. Take a careful look at the macula in each eye.

Take the Retina Quiz
1. What is the likely diagnosis for this patient?
a. Ocular albinism.
b. Oculocutaneous albinism.
c. Congenital nystagmus.
d. Congenital motor nystagmus.
2. What caused his poor vision?
a. Lack of pigmentation in the RPE.
b. Macular hypoplasia.
c. Optic nerve hypoplasia.
d. Both a and b.
3. What other exam findings should you expect besides those noted above?
a. Megalocorneas.
b. Iris transillumination defects.
c. Abnormal angle structure.
d. Both b and c.
4. How likely will the child be mainstreamed when he attends school?
a. Too early to tell.
b. Not very likely.
c. Very likely.
d. He will probably need special classes for visually impaired children.
5. What is the likely inherited pattern for this childs condition?
a. Autosomal dominant.
b. Autosomal recessive.
c. X-linked recessive.
d. There is no inheritance pattern.
For answers, click here.
Discussion
Once we dilated this patients pupils and looked at his retina, the diagnosis was fairly obvious. The striking lack of pigmentation within the RPE is typical for albinism.
Albinism represents a hereditary group of disorders characterized by a congenital lack of melanin pigment within the uveal tract. Although albinism may be isolated to the eye, more typically it involves the skin and hair, a condition known as oculocutaneous albinism. These patients present with obvious lack of pigmentation in their skin, and their hair has a bleached white appearance.
When only the eye is involved, we refer to the condition as ocular albinism. The skin and hair may even appear normal.
Most cases of ocular albinism are inherited as X-linked recessive, although three other types of ocular albinism have been characterized. Up to 10 types of oculocutaneous albinism have been classified, so the genetics of this disease can be quite complex.
Although we classify albinism as ocular or oculocutaneous, histopathologically, it appears as though there is only one form of the disorder: the oculocutaneous form. In the oculocutaneous form, the pigment-containing cells, known as melanosomes, contain melanin, though not very much. In ocular albinism, the skin and eyes contain macromelanosomes and type IV melanosomes in the iris; these allow for the clinical differences between the two groups.
Despite clinical variations between the types of albinism, nystagmus and reduced acuity are usually present. This is due to the lack of pigmentation within the fundus and macular hypoplasia.
Macular hypoplasia is the most consistent feature of albinism. The macula and fovea become poorly differentiated, with the rods present more in the fovea and the cones distributed away from the fovea. The foveal pit may be reduced or not even present, there is an absence of macular yellow pigment, and the retinal vessels may cross through the macula.
Another common feature of albinism: iris translucency. We usually can observe this easily in patients with oculocutaneous albinism, even with minimal light levels shining into the eye. In some patients the iris may take on a pink or blue-pink hue that we can observe on external examination. These patients are quite photophobic.
The iris changes may not be so easily seen in patients with ocular albinism. These patients are often misdiagnosed with congenital motor nystagmus. Our patient had iris transillumination defects but they were not as striking as they often are.
Other features that are common with albinism include delayed visual maturation, strabismus and photophobia. Because of the nystagmus and macular hypoplasia, many patients do not improve beyond 20/100 to 20/200.
Parents often worry about whether their child can be mainstreamed with normal-sighted children into regular classrooms. Optokinetic testing may help determine the prognosis. As you spin the OKN drum, normal-sighted individuals develop an optokinetic nystagmus. In patients with nystagmus, if you can superimpose the OKN over top of their nystagmus, or reverse the direction of the nystagmus with the OKN (as we did with our patient), the visual prognosis for these children being mainstreamed into normalsighted classes is very good. This can be extremely good and important news for worried parents.
We explained our patients diagnosis to the parents. We recommended an evaluation with a dermatologist and suggested that the child have a low vision exam in the near future, at least before he starts school.

