 |
In all the excitement of writing the last column for Focus on Refraction, it somehow slipped by us that it was the 50th! When I (Dr. Taub) was originally approached by the editors to help identify authors for a new column that focused on refraction and prescribing, I immediately raised my hand for the assignment and drafted Dr. Paul Harris as a partner in crime. We wrote together, typically taking turns in writing and editing, for seven years. Once he stepped away, I found a new writing partner in Dr. Pam Schnell, and we have been at it for another two and a half years. We have covered a spectrum of topics and tools that we use to help in prescribing decisions and have even waxed the philosophical (just a bit).
For our 51st column, we wanted to do a “clip show” and highlight some of the past 50 columns as a refresher for those of you who might have missed them. They are all available on the Review of Optometry website, so you can dig in at your leisure. Here’s a key point or two from each.
Buff up Your Buffers (Dec. 2020)
There are two important buffers the body has implemented in the visual system to help reduce the impacts of stress: low hyperopia and low exophoria. In prescribing, especially for school-aged children, keeping the two values of +0.50D and four exophoria in your consciousness is quite crucial. Similar to overdraft protection for your bank account as a buffer from overspending, keeping enough plus and exophoria helps from overtaxing the visual system. Accidentally over-minusing in search of that extra line of visual acuity or pushing plus on a hyperope are obvious ways to blow out your buffers.
Prescribing for Young Children (April 2020)
Just because you measure something does not mean that you need to take action. Vision changes in children over time and can do so significantly in the first few years of life. Prescribing early can interfere with natural development and emmetropization. Every optometrist has a comfort level in their prescribing that is based on their experience in patient care. Presented in this column is research from a group of optometrists who practice following the developmental/behavioral model. The takeaway is that as patients increase in age from three months to seven years, doctors become more proactive in prescribing.
Take it to the Limit (Dec. 2017)
As mentioned above, over-minusing is common and can damage visual development. While we are often proud that the patient can see the 20/15 line with each eye, how many extra clicks were needed to attain that visual acuity? Giving too much minus can also cause trouble with binocular vision/accommodation. Please keep in mind the impact of your prescribing.
Addition by Subtraction: Cutting the Cyl (Dec. 2022)
We have all had patients who show small amounts of cylinder at axis 90 or 180, and we often prescribe it without hesitation. What if we didn’t? We have found that eliminating the small cyl and providing the spherical equivalent does not change the visual acuity. Prescribing the cyl can embed it, making it harder to remove from future prescriptions and condemning the child to a lifetime of astigmatism when it could have been avoided.
 |
|
Simulation of significant cylindrical blur. Photo: Phillip Tribble, Southern College of Optometry. Click image to enlarge. |
Make Way for Yoked Prism (April 2021)
Prism seems to scare the heck out of many doctors. They run from it and crawl into the fetal position at the thought. Well, what if we told you that prism prescribed with both bases in the same direction can be used therapeutically to influence visual and body posture and behavior? We have successfully used yoked prism for patients with brain injury, special needs and even strabismus. The changes are typically immediate, impactful and force the patient to adapt to the altered visual input.
Double the Glasses, Double the Success (Feb. 2022)
Some of the most challenging patients to work with are those who have suffered a brain injury. They can complain of photosensitivity, visual field loss and trouble seeing out of their glasses. Brain-injured patients often have trouble with fine eye movements, which can include putting their eyes in the appropriate locations to see out of the various aspects of their lenses. Given that this population often uses bifocals or progressive addition lenses, one of the easiest ways to alleviate symptoms is to provide the patient with separate glasses for distance and near.
Fresnel Prism to the Rescue (April 2018)
Diplopia is a common complaint for patients with brain injury secondary to trauma or stroke. It can be challenging to manage due to the spectrum of reasons for the diplopia and the progression of improvement. Fresnel prism can be used for short-term alleviation of the condition. It has the benefit of being able to be changed frequently and easily, in contrast to ground-in prism, as the magnitude of the prism hopefully decreases. Fresnel prism can also be used in a leapfrogging manner therapeutically.
Low-Tech TBI Rehabilitation (April 2017)
Patients who have suffered brain injuries often have issues with focusing. We have heard this described in so many ways, from “something just does not feel right” to “the words keep moving” to “I can’t concentrate on reading.” In these cases, we break out the “magic tape” and apply binasal occlusion to the patient’s glasses. Of course it isn’t magic, but when it works, it certainly can seem like it to the patient.
While there are many theories why binasal occlusion works, we subscribe to the concept that for these patients, there is just too much visual noise, as there is a duplication of information in the center due to the overlapping visual fields. Binasal occlusion simply reduces the amount of visual input, allowing the patient to deal with less throughout the healing process.
Little Occlusion Goes a Long Way (Dec. 2016)
The type of occlusion that we highlighted in this column is different than the binasal occlusion mentioned above. Spot or strip occlusion is sometimes the only treatment option when a brain-injured patient cannot put two images together; their brains are just not ready for that challenge. This first step is temporary and allows for the patient to have improved function in other therapies, as well as in navigating their environment. Generally, within a few weeks, we can transition to Fresnel prism.
Looking Through Rose-Colored Glasses (Feb. 2023)
Photosensitivity can be life-changing. Can you imagine the constant pain from not only light outside but also from the lights that hang in almost any public venue? Using custom tints with saturations that range from light blockage (15%) to dark (60% to 80% blockage), we have the power to give patients their freedom back. The most common colors that we employ are a yellow-orange (FL-41) and blue. The changes in visual comfort are immediate and can even help patients with migraines in which light is a trigger.
 |
|
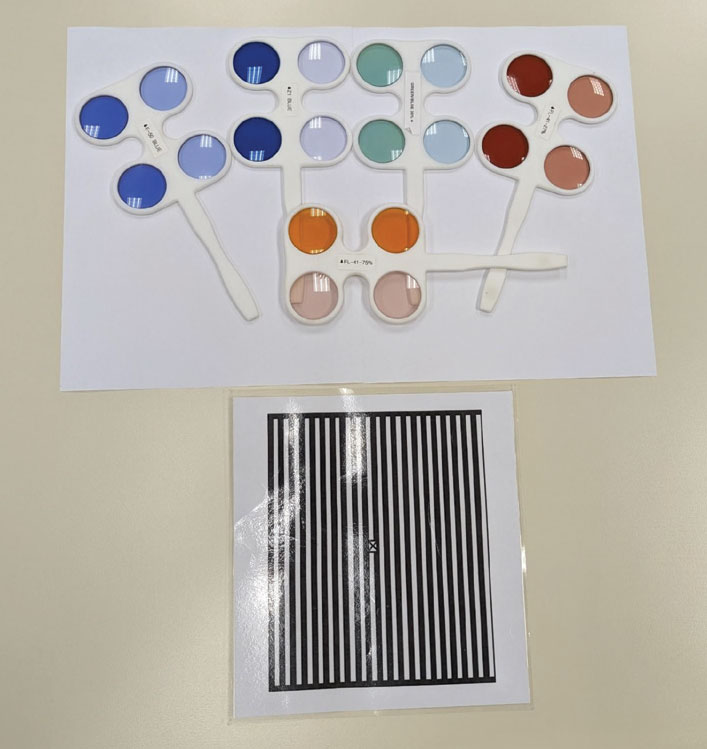
A variety of tints from the Chadwick Optical ABI flipper set and the Bowan grating card. Click image to enlarge. |
Visuoscopy Review (Aug. 2023)
Over the years, we have discussed a variety of exam techniques to aid in the diagnostic process. Visuoscopy takes about 30 seconds and provides insight into fixation ability and why your patient might not be capable of seeing 20/20. Knowing whether fixation is decentered or unsteady helps in the treatment decision-making tree and provides insight that you would not otherwise have gotten through your normal exam routine.
Aiming for 100
Dr. Taub’s grandfather, when asked how he was doing, used to respond that “the first 100 years are the hardest.” Well, we can say that the first 50 columns were honestly not the hardest, but exactly the opposite; we had so much fun writing them! They represent our philosophy regarding the visual process and how we practice, and we have been honored to share them with you all—or “y’all” if you live in the South like we do! We look forward to the next 49 on our way to 100!
Dr. Taub is a professor and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury. Dr. Schnell is a professor at SCO and teaches courses on ocular motility and vision therapy. She works in the pediatric and vision therapy clinics and is co-supervisor of the Vision Therapy and Pediatrics residency. Her clinical interests include infant and toddler eye care, vision therapy, visual development and the treatment and management of special populations. They have no financial interests to disclose.

