 |
History
A 6-year-old black female presented for an evaluation of a red and painful eye with excessive discharge.
She had been seen in the E.R. and referred to the office with a generic diagnosis of conjunctivitis.
Her systemic history was noncontributory.
Diagnostic Data
Her best-uncorrected acuity was 20/100 O.D. and 20/100 O.S. at distance and near. External examination was normal and there was no evidence of afferent pupillary defect.
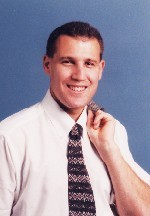
The pertinent anterior segment findings are demonstrated in the photograph.
Applanation intraocular pressures measured 19mm Hg O.U. The dilated fundus findings were normal in both eyes.
Your Diagnosis
How would you approach this case? Does this patient require additional tests? What is your diagnosis? How would you manage this patient? What is the likely prognosis?
 |
| A 6-year-old black female presented with the clinical appearance shown here. |
Discussion
Additional tests include evaluation of the conjunctiva for follicles and papillae, lid eversion to rule out membrane formation, staining of the cornea with sodium fluorescein to assess the status of the epithelium, inspection of the cornea for subepithelial infiltrate, and palpation of the lymph nodes to rule out lymphadenopathy. Laboratory testing includes a gram stain, cytologic examination of a conjunctival scraping, and culture and sensitivity.1-4
The diagnosis in this issue is gonococcal conjunctivitis with significant epithelial keratopathy and subepithelial infiltration. The patient was admitted, placed on I.V. ceftriaxone, 1g q.2.h., for five days, lid scrubs with aggressive lavage q.h. followed by the administration of topical ciloxan. The patient improved in 24 hours and was followed every day for the five days of her stay. The conjunctivitis was considered completely resolved in two weeks.
Bacterial conjunctivitis, which is uncommon, is characterized by a rapid onset of unilateral conjunctival hyperemia, lid edema and mucopurulent discharge. The second eye typically becomes involved 1-2 days later.1-5 Bacterial conjunctivitis can be classified into three clinical types: acute, hyperacute, and chronic. The most common conjunctival pathogens include Staphylococcus, Streptococcus pneumoniae, Haemophilus species, Moraxella, Corynebacterium diphtheriae, Neisseria species and enteric gram-negative rods.4
Neisseria gonorrhoeae and N. meningitidis are gram-negative intracellular diplococci. In corneal and conjunctival scrapings, they are found within epithelial cells. Gonorrheal conjunctivitis is a significant concern since the organism can invade through an intact epithelium.3 Corneal infection often is peripheral, and can progress to perforation and endophthalmitis. In the adult, ocular gonorrhea is accompanied by a copious, weeping, hyperpurulent discharge.1 -5 Keratitis is common with the conjunctivitis. The transient, usually peripheral, subepithelial infiltrates that might be seen likely represent a type III hypersensitivity reaction.
The most common cause of hyperacute bacterial conjunctivitis is N. gonorrhoeae.4 This disease is an oculogenital disease seen primarily in neonates, sexually active adolescents, and young adults. The clinical course includes profuse, thick, yellow-green purulent discharge, painful hyperemia, chemosis of the conjunctiva, and tender preauricular nodes.4
The treatment of hyperacute bacterial conjunctivitis is directed to the specific pathogen. Conjunctival scraping for gram stain and culture on blood and chocolate agar is strongly suggested. If gram-negative diplococci are seen, suspect gonococcus. Gonococcal conjunctivitis is treated with both topical and systemic antibiotics; an effective regimen includes intramuscular ceftriaxone 1g followed by a 2-3 week course of oral tetracycline or erythromycin (cross coverage for chlamydia).1-4 Patients with corneal involvement require daily follow up.1-5
1. Rhee DJ, Pyfer MF. Acute conjunctivitis. In: Rhee DJ, Pyfer MF. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 1999: 119-121.
2. Burden G, Bryant S. Conjunctivitis. In: Burden G, Bryant S. Laboratory and Radiologic Tests for Primary Eye Care. Boston: Butterworth-Heinemann, 1997: 36-38.
3. McLeod, S. Bacterial Keratitis. In: Yanoff M, Duker JS. Ophthalmology. Philadelphia: Mosby, 1999: 5.8.1-5.8.10.
4. Rubenstein JB. Disorders of the Conjunctiva and Limbus. In: Yanoff M, Duker JS. Ophthalmology. Philadelphia: Mosby, 1999: 5.1.1-5.1.22.
5. Hawley HB. Gonorrhea. Finding and treating a moving target. Postgrad Med 1993; 94(2):105-11.
|
Next Month in the Mag Feedback |

