Because we see so many patients in a day, we tend to forget that simply writing a script is not enough to ensure medication compliance. While we will never be able to get all of our patients to comply with their drug regimens, by becoming familiar with these seven patient excuses for non-compliance, we will be able to significantly increase ad-herence.

Writing out a prescription is not enough to ensure ophthalmic drug compliance.
1. I dont understand my condition/need for treatment.
Though not intentional, after managing countless glaucoma and red-eye patients, its easy to forget what its like to be the one sitting in the opposite chair. If we were to record and re-listen to some of our conversations with patients about their diagnosis and treatment and even time those conversations, we might be surprised at what wed uncover. Wed probably learn that half the information we thought we clearly stated, really wasnt. We might also discover that:
The conversation was much shorter than originally perceived.
The patient had very little (if any) time to ask questions.
Half of the conversation was in doctor language, not patient-friendly language.
The following five prescription writing commandments illustrate just what level of exam room education is necessary:
Explain to your patient in detail what his condition is and why the selected treatment is necessary. Our patients are not clinicians, and therefore do not understand the medical language we often use when discussing their diagnosis and treatment plan. If patients dont understand, and we dont make a point of enabling them to understand, they will not comply with our instructions. To prevent this from being a factor, we must use detailed laymans terms, and invite our patients to interrupt with any questions.
Use visual aids. These can include digital photos, drawings, brochures, pictures from books and scanned and printed materials. All these can help our patients understand their diagnosis and can help emphasize the need for treatment.
Establish a time line for treatment and for re-evaluation of their existing condition.
Provide explicitly written in-structions. This way, your patients can understand what they need and how to use their medication(s). Ver-bally reinforce what youve written.
Make up simple office forms that highlight these five steps, so that your patients buy into the treatment you are proposing mentally and financially. (See Sidebar.) Its amazing how quickly patients recall their medications and proper dosage when they know their doctor is referencing the sheet.
2. I dont know how my health insurance works.
If you do not make yourself aware of your patients health insurance coverage and in turn make him aware, you will ultimately lose many drug compliance battles. For instance, I had a patient with recurrent iritis secondary to a systemic condition. The severity of the patients iritis warranted a brand name steroid medication. I made this very clear to the patient. In examining her health insurance, I discovered that the company would only pay for the generic alternative. Had I not educated the patient about the necessity of the brand name and looked into her insurance, she would have been in for a very unexpected financial surprise, and I probably would have received an angry telephone call.
Instead, I faxed a letter to her insurance company with data to support my name brand request. As a result, they granted her coverage. In following-up with her insurance company the same day, I was also able to establish how long it would take for a ruling on my request. This response enabled me to know how many samples she would require in the interim.
3. Why should I spend money on something that may not work?
To prevent this non-compliance issue, start your patients on samples of the drug. This approach works especially well with long-term medications such as antihistamines and mast-cell stabilizers.
I write a formal prescription for the medication, but tell the patient to initiate use with the sample first. The patient is instructed to closely monitor their symptoms and look for noticeable improvements during five to seven consecutive days of use. If the medication works well, I instruct them to fill the prescription. If there is no improvement, I ask them to call me, and schedule a follow-up visit. At their follow-up, I will often switch samples and start a new five to seven day evaluation.
Develop a Medication Compliance Form
It sounds elementary, but imagine handing the patient a professional piece of paper with:
The date.
The patients name.
The name of his condition.
The medication.
Frequency of usage.
Medication time line.
Follow-up.
This sheet should also have some pictures that demonstrate the proper technique for instilling ointment and drops. The final key toward gaining compliance with this type of handout is to make sure you provide a copy to your patient, and place the original form in the patients chart.
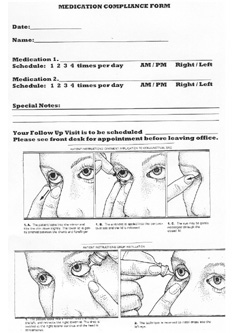
Dr. Marossys patient office form gains adherence because it promotes the patients ability to recall their regimen.
Technique photographs courtesy: Atlas of Primary Eyecare
Although this process would certainly not work in many clinical situations (such as glaucoma), it works very well for allergies. Compliance will increase enormously because patients have proven to themselves that there is improvement with the medication, and that the medication is necessary to help their symptoms. You suddenly have motivated and compliant patients who start referring others to your office because of your expertise and unique approach to letting them try before they buy.
While we can manage education in the examine room, we cannot manage what our patients do once they leave the office. The following illustrate the non-compliance excuses we hear after weve sent our patients on their way and what we can do when we hear them.
4. I forgot to take it.
Cognitive function is another issue involved in noncompliance with medication. According to one study, the number one reason glaucoma patients, in particular, did not take their topical medications was because they forgot.1 As previously discussed, developing a copy of the drug information sheet should help with memory, but there are four other simple ideas you can use to aid in cognitive retention.
Have the patient bring a family member or close friend in the exam room when you discuss the treatment plan. (With new HIPAA guidelines, the patient must consent via verbal confirmation or signed consent form to allow another person to be present.)
Have the patient set an alarm in the house or on a wristwatch at the specific time(s) the medication is to be administered.
Have the patient coordinate medication dosing with planned daily meals.
Instruct them to incorporate medication usage with something else regularly done. For example, if the first thing the patient does each morning is to make coffee, tell them to put the medication next to the coffee filters.
5. Id rather suffer than have to deal with the side effects.
We sometimes forget that our patients have different tolerance levels, sensitivities and concerns. Side effects especially tend to be a major issue with many patients who take long-term medications. For example, some of my female glaucoma patients with blue or green eyes often refuse to take Xalatan (latanoprost, Pharmacia) because theyre afraid it will cause their iris color to change to brown.
Having discovered this cosmetic concern, I now present many of my glaucoma patients with a cafeteria plan (an assortment of drugs in the same class), so they can find something they are fairly comfortable with right off the bat and ultimately comply with.
6. I cant put my medication in.
A few months ago, I saw an elderly patient with glaucoma who was not taking the drops I had prescribed, nor would she tell me why. She indicated that she understood the importance of taking her medication and what the side effects were, so I knew I had communicated effectively in the exam room. Secondly, she was cognitively sharp, so I deduced memory was not an issue. And finally, since she had purchased the medication, I knew a lack of finances was not the problem.
The only conclusion I could draw was that she was having problems instilling her drops. Since I knew she was a very proud and independent woman, I asked her daughter, who had accompanied her, if she would leave the exam room, so that I could talk with her mother one-on-one. Once the daughter left, I asked the patient to show me how she put the drops in. Sure enough, she could not lift her arm to do it. After I showed her how to instill them while lying down, she confessed that she hadnt said anything initially because she was afraid her daughter would think she couldnt take care of herself and would ultimately place her in a nursing home.
While the physical inability to instill her medicine was not her fault, the fact that she did not initially tell me about it was. Aside from coming up with alternatives to employ medication, what you should also take from this story is that non-compliance is often not cut-and-dry and may require some detective work.
7. I cant afford it.
Nobody wants to admit financial problems. Its embarrassing. To save face, these patients will understandably avoid explaining why they are not complying. But as in the previous case with the patient who had trouble instilling her medication, we must remember to examine each individual case and use deductive reasoning to find out if money is behind their non-compliance. While this is probably the most difficult issue, we can do three practical things to help these pat-ients obtain their medications and comply with our instructions.
State Programs. There are currently 41 state-run drug assistance programs designed to assist seniors, low-income individuals and those with special needs (Alaska, Colorado, Idaho, Mississippi, Nebraska, North Dakota, Oklahoma, Utah and Virginia do not). Although, I have not personally had to utilize state programs, I would certainly suggest looking into it. This can be done by visiting www.rxassist.org (a Volunteers in Health Care site). Simply click on State Programs, and you will be able to find out what is offered and whom to contact in your state.
Drug Discount Cards. While some pharmaceutical companies currently offer drug discount cards, I have found that the only card that may cover ophthalmic drugs is the Nonprofit Warehouse card. The card is free and does not require registration, enrollment or an application process. It can provide savings of up to 50% off the pharmacys price for prescription generics and 15% for prescription brand name medications, and it can be used to obtain prescriptions not covered by the patients insurance company.

Forty-one states offer drug assistance programs.
Further, while the patient cannot use the card in conjunction with their insurance or any other discount card, it can be used in place of the patients insurance or co-pay, should it give them a better price. The card is supposed to be valid in almost 50,000 pharmacies nationwide. Patients can obtain the card at: www.nonprofitwarehouse.com.
Patient Assistance Programs. PAPs are offered by pharmaceutical companies that either discount or provide certain medications free of charge to patients who dont have health insurance or who dont have a prescription benefit plan through their health insurance. As physicians, we must establish the severe medical and financial needs of these patients by filling out the individual forms offered by each pharmaceutical company. These forms can be found at: www.rxassist.org/default.cfm. Simply scroll down and click on Search Programs, and there are a number of search criteria you can use to find out if the ophthalmic medication(s) your patients need are available. I keep an inventory of the most popular PAP forms in an easily accessible place in my office. After the forms have been filled out (keep in mind, this may necessitate another appointment), they need to be immediately faxed. And on the same day, you need to follow-up immediately to find out when they will be processed, so you can know how to manage the case in the interim.
At this point, I turn to my bank of samples. While some optometrists get into the habit of giving out samples to everybody, I reserve my samples based on the amount of a specific medication I get and the number of severe cases, both medical and financial, that present. For example, in dealing with emergency patients who have corneal ulcers or iritis, I am sure to keep a small, highly coveted stock of those samples on hand. And because glaucoma can often be both a medical and financial issue for my patients, I tend to reserve those as well.
Of course, non-compliance will forever be an ongoing battle in every practice. But if we focus our attention on using our therapeutic privileges, obey the five prescription writing commandments and educate ourselves on the other non-compliance issues that plague our patients, we might just have a shot at winning the war in the long run.
Dr. Sarah Marossy currently practices in Coeur d Alene, ID. She also lectures on a national level.
1. Taylor, SA, Galbraith SM, Mills, RP. Causes of non-compliance with drug regimens in glaucoma patients: a qualitative study. J Ocul Pharmacol Ther 2002 Oct;18(5):401-9.

