By 2050, the number of people in the United States with cataracts is expected to double from 24 million to about 50 million.1 This growing need for cataract surgery will occur simultaneously with a well-publicized shortage of nearly 122,000 physicians by the year 2032—and ophthalmology is one of the subspecialties that will be in the highest demand.2
There couldn’t be a better time for us to collaborate more regularly and comprehensively with our ophthalmology colleagues to meet our cataract patients’ needs. To provide the best possible results for our patients, surgeons will need to spend more time in the operating room, while ODs take charge of preoperative counseling and postoperative management.
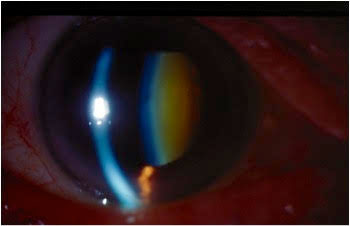 |
| When a patient has an advanced cataract ready for surgery, you need to have a surgeon ready for your referral. Click image to enlarge. |
Choosing a Surgeon
Trust is the cornerstone of any comanagement relationship and is equally paramount when patients’ outcomes are at stake. When seeking out a surgeon, first ask other local and trusted optometric colleagues where they send their patients. Additionally, a surgeon who already works in a collaborative practice with ODs will most likely be happy to comanage patients with you.
Before referring patients to a surgeon, first get to know that surgeon, their staff, affiliate doctors (ODs and MDs), and anyone else who will be involved in taking care of patients. Visit and observe the preoperative consult, the day of surgery and postoperative workflow. A referral office will likely require this for ODs who actively comanage surgery. This will also give you first-hand knowledge of the patient’s journey, so you can better prepare them prior to their referral.
You should also take the time to meet with and interview the surgeon. It is imperative that you agree on the surgical plans for your patient. Here you can ask a number of important questions to make sure you are on the same page:
- At what point will you recommend surgery?
- What type of cataract surgery do you offer patients, traditional or femtosecond laser?
- What types of intraocular lenses do you offer? What do you have the most experience with and how will this impact the options available to patients? Do you offer toric monofocal IOLs as an alternative to patients with corneal cylinder? Do you offer multifocal IOLs? If so, what type?
- Who qualifies for surgery?
- What is the patient’s out-of-pocket expense?
- Do you treat patients with concomitant diseases such as glaucoma or Fuchs’ dystrophy?
- Do you offer minimally invasive glaucoma surgery (MIGS) or other corneal procedures? Which ones? If yes, what are the results?
Discuss the refractive aspect of the cataract surgery and be comfortable with the IOL selection process, including the surgeon’s IOL preferences (monofocal, toric, multifocal, trifocal and extended-depth-of-focus). Be sure to agree on how best to educate patients on each of these options and make sure there is a clear path for the surgeon to receive your refractive recommendations at the time of the initial consultation, as this is integral to the preoperative discussion.
Before entering into a comanagement relationship, agree with the surgeon’s office in advance regarding the division of clinical labor to streamline the process for patients. This should include a protocol for routine postoperative management and a proactive plan for less common but more urgent issues that arise, ensuring patient safety and continuity of care following a procedure. This is an opportune moment to take responsibility for the preoperative and postoperative care.
In addition to meeting with the surgeon, get to know the administrative staff of the consulting surgeon. Office managers and administrators from both referring and consulting offices play a pivotal role in maintaining the comanagement relationship, as transferring clinical information between offices is vital to maintaining continuity of care. Simplifying this process will guarantee a seamless transition back to your office. Additionally, don’t forget to establish billing and coding processes prior to any referral so you get reimbursed properly for services you provide.
Which MIGS is Ideal?In the case of a glaucoma suspect with acceptable IOP, a stand-alone cataract surgery may be indicated. While the exact mechanism is unclear, most believe removing the cataract alone helps with increasing outflow.3,4 These patients’ IOP can therefore be monitored closely after surgery and treated if and when necessary. A well-controlled patient, who has been treated by one or a combination of modalities, including laser trabeculoplasty or topical medications, is the perfect candidate for a MIGS procedure. However, not all patients need the same degree of IOP-lowering effect, and not all surgeons perform all procedures. Most of the MIGS procedures performed by cataract surgeons today are focused on using an ab interno approach to increase trabecular outflow following phacoemulsification. Some of the more commonly used procedures in this category include the iStent Inject (Glaukos), Kahook Dual Blade (New World Medical), Hydrus Microstent (Ivantis) and Omni Surgical System (Sight Sciences). Each of these procedures are unique in their own right, yet they all require the same general operating room protocol, which involves the surgeon performing an angle procedure with intraoperative gonioscopy usually following a standard phacoemulsification.5 |
Laser vs. Traditional Surgery
Not only should you align your philosophies with the surgeon regarding the type of cataract surgery offered, you should also know how patients are educated on the different types of surgery. Both the referring optometrist and consulting surgeon have a responsibility to educate patients on their shared viewpoint as well as the reasons for recommending one procedure over another.
Femtosecond laser-assisted cataract surgery has been available for more than seven years, with thousands of surgeons using one of many available technology platforms. Optometrists recommending cataract surgery should be well versed on the advantages of this technology and be comfortable discussing with patients.
The light energy employed by the femtosecond laser assists the surgeon in creating the incisions into the eye, the capsulorhexis, the phacofragmentation and corneal arcuates for astigmatism management. This allows for reduction in energy and manipulation by the surgeon when in the operating room. It can also lead to faster recovery times with less postoperative restrictions for patients. The femtosecond laser can even lead to more consistent effective lens positioning when placing the IOL, allowing for higher predictability in refractive outcomes for patients.
Preoperative examination. A thorough and detailed preoperative exam is the most important component of making the appropriate recommendation for the refractive component of the cataract surgery. When determining whether a patient will benefit most from a traditional monofocal spherical IOL or a specialty toric or multifocal IOL, you should diligently identify and manage any ocular surface conditions that can potentially affect the outcome of cataract surgery. In particular, ocular surface disease and significant dry eye may require aggressive treatment before and after surgery. Additionally, other corneal considerations include pterygia, corneal dystrophies (both anterior basement membrane and Fuchs’), post-refractive corneal irregularities and Salzmann’s nodules. All of these may limit visual acuity following cataract surgery and should be addressed with the patient beforehand.
Likewise, patients with significant visual field changes from glaucoma or reduced visual acuity from retinal disease may also have post-cataract visual limitations. Again, you should prepare the patient and communicate with the surgeon prior to their initial preoperative evaluation.
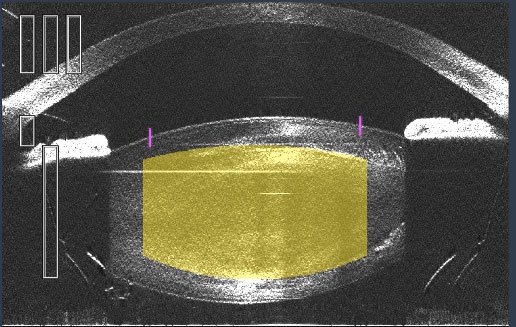 |
| This OCT image shows the lens during a femtosecond laser cataract procedure. Click image to enlarge. |
MIGS Considerations
For glaucoma or ocular hypertension patients who are ready for cataract surgery, the process has become a little more complicated with MIGS. This addition to the surgical process affords patients a great opportunity to reduce their dependence on IOP-lowering medications.3 Once you know your surgeon’s capabilities, MIGS preferences and candidacy protocols, you can educate your patients and make timely and appropriate referrals.
Prior to referring a patient for a surgical consult, assess the patient’s disease severity and stability and make an appropriate recommendation to both the patient and the comanaging surgeon. Depending on their individual needs, you may recommend phacoemulsification alone or combined with either a MIGS or a filtering procedure.
MIGS procedures have transformed the treatment protocol for glaucoma patients undergoing cataract surgery because of their ability to achieve consistent IOP control, independent of patient compliance, while lowering the incidence of both side effects and surgical complications.3 A variety of procedures are available (with several more in trials) that achieve IOP control by:
- Increasing trabecular outflow
- Reducing aqueous production
- Increasing subconjunctival filtration
Not only do these procedures provide safe and effective IOP control in combination with cataract surgery, they are also more accessible to surgeons because they do not require the use of large, expensive devices.4 Instead, many of the current options are easily kept in stock in the operating suite with little capital expense to the surgical center.
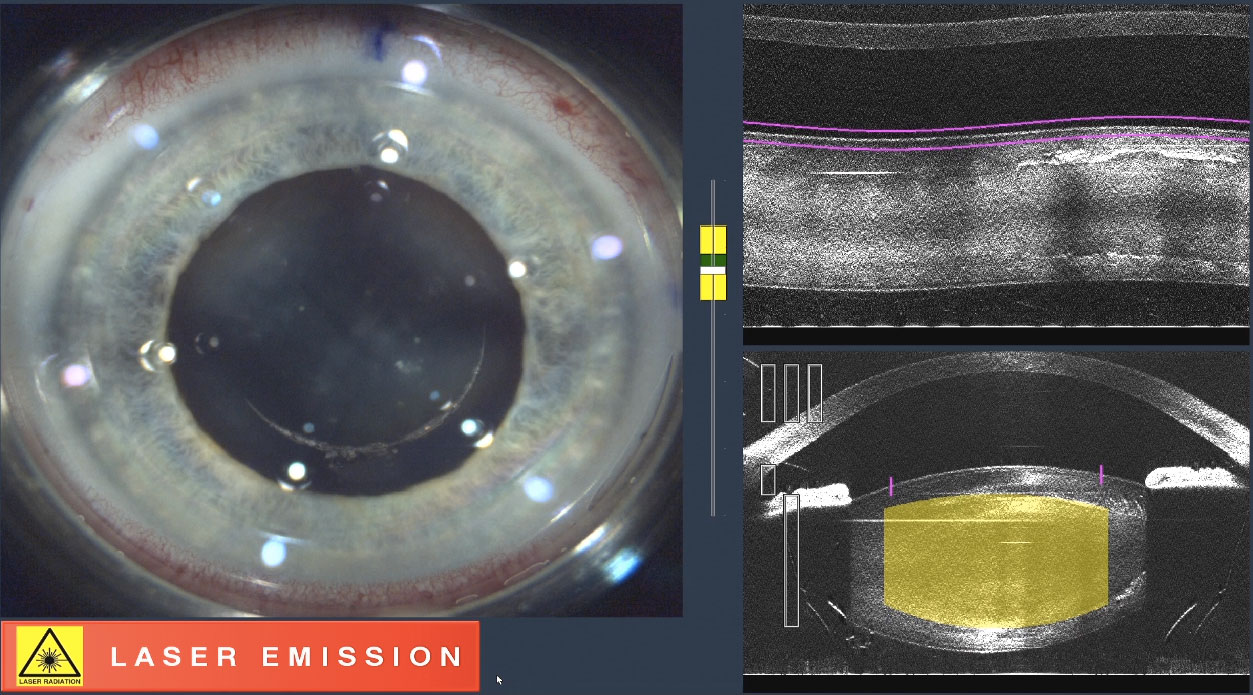 |
| Here, the femtosecond laser is creating a capsulorhexis. Click image to enlarge. |
Choosing the Right IOL
The comanagement of cataract surgery unequivocally calls for a refractive discussion between you and the surgeon. As the practitioner recommending surgery, you know best the visual requirements of the patient seeking a surgical consultation, while the surgeon may have never met them. You have the established relationship and understand the patient’s personality, occupation, hobbies and lifestyle.
Thus, you are in the best position to counsel patients on the optimal IOL options to fit their needs, characteristics and expectations. This is augmented by your robust knowledge of the surgeon’s IOL preferences discussed during your initial comanagement interview, which allows you to make proper recommendations consistent with the information the MD will provide.
This is especially important when suggesting a premium IOL, such as a toric or presbyopia-correcting IOL, considering these are out-of-pocket expenses for patients. Here you must collaborate with the surgeon to establish the criteria for patient candidacy for a premium IOL. Not every patient is a good candidate for every technology. Part of the preoperative consultation should include educating patients on available technology and discussing if they would be good candidates for the advanced options.
For example, if a patient has less than 1.00D of corneal astigmatism, they would not be an ideal candidate for a toric monofocal IOL. The lowest amount of cylinder available on most toric IOLs in the United States is 1.50D at the IOL plane. Accounting for effective lens positioning, this will neutralize 1.00D of cylinder at the corneal plane. If a patient has less, they would be a better candidate for a standard spherical IOL.
For presbyopia-correcting IOLs, your discussion with the comanaging surgeon will be more in depth with many different options. They are available in accommodating, bifocal (which can vary in add powers of +4, +3, +2.50), extended-depth-of-focus (EDOF) and newly FDA-approved trifocal designs. Each of these IOLs will act differently in the eye, and it is important to know which IOL your surgeon will offer to your patient so that you can prepare them accordingly.
To set your patients up for successful outcomes, you must recommend the best IOL options for each patient, whether they have presbyopia or not. You can identify ideal candidates for a presbyopia-correcting IOL with a focus on these three issues:
Motivation. A patient who is excited and motivated to be less dependent on their glasses or contact lenses is the first characteristic to look for. A patient who has worn glasses all of their life and is happy continuing to do so may not have the inclination to change.
Realistic expectations. Help the patient understand exactly what the IOL can and cannot do. The patient must be aware of any limitations before committing to surgery. Explaining this postoperatively will be perceived as a surgical failure, and patients will be unhappy. For example, even with a multifocal IOL, a patient may find they need to use glasses for certain tasks.
Depending on the chosen IOL, there will likely be a “sweet spot” for near vision tasks at a given working distance. This means patients may need readers if they are attempting a near task closer or further than this “sweet spot” focal distance. In addition, most multifocal IOLs are light dependent, so patients need to understand that optimal lighting will help them. If, however, they don’t have control of the lighting (e.g., in a dimly lit restaurant), they may need readers to assist.
 |
| Here is a multifocal option. Click image to enlarge. |
 |
| Here is a toric option. Click image to enlarge. |
Challenging Patients
Open communication with your consulting surgeon will make it easier to manage even the most challenging clinical situations, including patients who are post-refractive surgery, post-retinal detachment surgery or a patient with only one cataract that will need a balance Rx in their IOL. For these patients, you are truly in the best position to educate the consultant and drive the decision-making process for the refractive plan prior to the patient meeting the surgeon for the initial consultation.
As more patients present ready for cataract surgery and more surgeons are spending a greater portion of their time in the operating room, optometrists are poised to expand their role managing preoperative cataract consultations and postoperative surgical care. It is imperative that the optometrist maintains an open line of communication between their office, the patient and the consulting surgeon’s office. Making sure that all parties are on the same page will ensure a seamless transition to accomplish a happy postoperative outcome.
Dr. Stutman is the director of Optometric Services at Select Eye Care in Elkridge, MD.
1. National Eye Institute. Cataract Data and Statistics. nei.nih.gov/eyedata/cataract. Accessed October 17, 2019. 2. Association of American Medical Colleges. Desperately Seeking Surgeons. news.aamc.org/patient-care/article/desperately-seeking-surgeons. April 26, 2019. Accessed October 17, 2019. 3. Saheb, H, Ahmed, IIK. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23(2):96-104. 4. Fingeret M, Dickerson JE, The role of minimally invasive glaucoma surgery devices in the management of glaucoma. Optom Vis Sci. 2018;95(2):155-62. 5. Belovay GW, Naqi A, Chan BJ, et al. Using multiple trabecular micro-bypass stents in cataract patients to treat open-angle glaucoma. J Cataract Refract Surg. 2012;38(11):1911-17. |

