 |
A 50-year-old Hispanic male reported that he has been experiencing blurred vision and distortion in his left eye for the past two months. He said a similar episode occurred in his right eye a few years earlier but resolved on its own after several weeks. He said his vision was not improving, and he wanted to learn the cause of this latest episode.
The patient has been HIV-positive since 1993. He said that he takes a cocktail of medications, but he could not remember their specific names. His T cell count was in the 400s, and his viral load was undetectable.
Best-corrected visual acuity was 20/30 O.U. Confrontation fields were full to careful finger counting O.U. The pupils were equally round and reactive, and there was no afferent pupillary defect in either eye. Amsler grid testing revealed a small area of central metamorphopsia O.U.; the left eye was worse than the right. The anterior segment exam was unremarkable O.U. Intraocular pressure measured 10mm Hg in each eye.
 |
 |
|
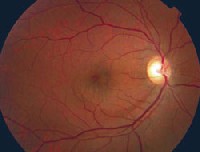
1,2. The posterior pole of each eye (O.D. left, O.S. right) showed these suspicious findings. The macula in the right eye showed mottling at the level of the RPE. More obvious macular changes were present O.S. |
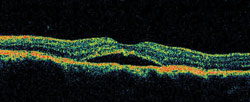
Dilated fundus exam revealed a clear vitreous in each eye. Each optic nerve showed a moderately large cup; this was greater O.D. than O.S. The vessels appeared normal O.U. The macula in the right eye showed mottling at the level of the retinal pigment epithelium, or RPE (figure 1). More obvious macular changes were present O.S. (figure 2). The periphery was normal in both eyes with no open holes, tears, breaks, subretinal fluid or retinal detachment. Optical coherence tomography (OCT) showed the changes seen in figure 3.
 |
|
3. OCT on the first visit showed these peculiar findings in the macula. |
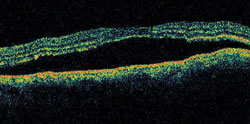 |
| 4. The OCT on a follow-up visit showed these changes. Our patient noted that his eyesight was worsening. |
1. What do the macular findings in the left eye represent?
a. Pigment epithelial detachment.
b. Neurosensory retinal detachment.
c. Cystoid macular edema.
d. Active retinitis.
2. What does the OCT show?
a. Pigment epithelial detachment.
b. Neurosensory retinal detachment.
c. Cystoid macular edema.
d. Active retinitis.
3. What is the correct diagnosis?
a. Idiopathic central serous chorioretinopathy.
b. Choroidal neovascular membrane (CNVM).
c. Acute syphilitic placoid chorioretinitis.
d. Cystoid macular edema.
4. What is the pathophysiology of this condition?
a. Increased perfusion within the choriocapillaris.
b. Blockage within the RPE.
c. Neovascularization due to increased levels of vascular endothelial growth factor.
d. Infection from Treponema pallidum.
5. How should we manage this patient?
a. Continued observation.
b. Laser photocoagulation.
c. Intramuscular penicillin.
d. Photodynamic therapy.
6. What else can be seen in the fundus photograph?
a. RPE mottling in the right eye.
b. Large cup-to-disc ratio.
c. Nerve fiber layer defect.
d. All of the above.
For answers, go to bottom of page.
Discussion
The macula in the left eye shows a small puddle of fluid involving the fovea. This represents a detachment of the neurosensory retina from the RPE. OCT confirmed this finding. These findings are classic for idiopathic central serous chorioretinopathy (ICSC), also called central serous retinopathy.
ICSC typically occurs in 20- to 45-year-old males who exhibit type A personalities.1 Although our patient is age 50, it does not change our diagnosis; ICSC has been reported in patients as old as age 60.2 It occurs more commonly in males than females (a 10-to-1 ratio), and there is often a strong relationship between ICSC and emotional stress, although we do not know whether stress triggers the condition.1 Migraine headaches also have been associated with the onset of these neurosensory detachments.
On examination, the macula usually exhibits a round or oval area of elevation of the neurosensory retina. This can be very subtle and easily missed if the detachment is small or if there is a very shallow amount of subretinal fluid.
Before OCT was available, fluorescein angiography (FA) was the gold standard for confirming a diagnosis of ICSC. The typical staining pattern is a focal spot of hyperfluorescence early in the angiogram. This represents a small micro-pigment epithelial detachment (PED). The hyperfluorescence increases, and the area of the neurosensory detachment has a subtle glow. But, the neurosensory detachment never completely hyperfluoresces as a larger PED would. A classic smokestack appearance occurs in about 10% of patients.1 Multiple areas of hyperfluorescence are sometimes seen, mainly in patients who have had recurrent episodes of ICSC.
We performed OCT on our patient instead of FA. OCT highlights the extent of the neurosensory detachment and confirms the absence of a CNVM. If there is a question about whether the patient has ICSC or another entity, both FA and OCT can help you in your differential diagnosis.
We do not fully understand the pathophysiology of ICSE. Although it manifests as a retinal problem, the underlying disease process most likely begins in the choriocapillaris. A localized area of increased permeability damages the overlying RPE, which then produces the micro-PED; this is followed by the neurosensory detachment. Systemic diseases, such as lupus and uncontrolled hypertension, also can lead to increased permeability in the choriocapillaris; thus, the fundus appears similar to ICSC. HIV-positive patients, like our patient, also may present with neurosensory retinal detachments.3
Most patients who have ICSC improve within six months without treatment. Laser photocoagulation at the site of the RPE detachment is recommended to seal off the area of leakage in patients whose condition does not improve. More recently, photodynamic therapy with Visudyne (verteporfin, Novartis Ophthalmic) has shown success in treating recalcitrant ICSE.4
We initially chose to observe our patient, but he presented two months later with a larger neurosensory detachment. FA showed diffuse areas of leakage, so we chose to treat him with PDT. The detachment resolved within a month, and visual acuity returned to 20/25.
Our patient has a moderately large cup-to-disc ratio in each eye; this is greater O.D. than O.S. A prominent nerve fiber layer defect, seen as a darker wedge-shaped area, radiated inferiorly from the optic nerve O.D. This was suspicious for glaucomatous optic nerve cupping. Threshold visual field testing revealed a small superior nasal defect O.D., but we were not too concerned given that the patients IOP measured 10mm Hg O.U.
We plan to observe the patient to see if he develops progressive optic neuropathy. Although IOP measured 10mm Hg on several follow-up exams, damage to the optic nerve may have occurred previously, when IOP may have been much higher. HIV has also been associated with lower IOP.5
1. Gass JDM. Stereoscopic Atlas of Macular Disease: Diagnosis and Treatment. 4th ed. St Louis: CV Mosby, 1997:52-70.
2. Schatz H, Madeira D, Johnson RN, McDonald HR. Central serous chorioretinopathy occurring in patients 60 years of age and older. Ophthalmology 1992 Jan;99(1):63-7.
3. Spalding JM. Central serous chorioretinopathy and HIV. J Am Optom Assoc 1999 Jun;70(6):391-8.
4. Taban M, Boyer DS, Thomas EL, Taban M. Chronic central serous chorioretinopathy: photodynamic therapy. Am J Ophthalmol 2004 Jun;137(6):1073-80.
5. Arevalo JF, Munguia D, Faber D, et al. Correlation between intraocular pressure and CD4+ T-lymphocyte counts in patients with human immunodeficiency virus with and without cytomegalovirus retinitis. Am J Ophthalmol 1996 Jul;122(1):91-6.
Answers: 1) b; 2)b; 3)a; 4)a; 5)d; 6)d.

